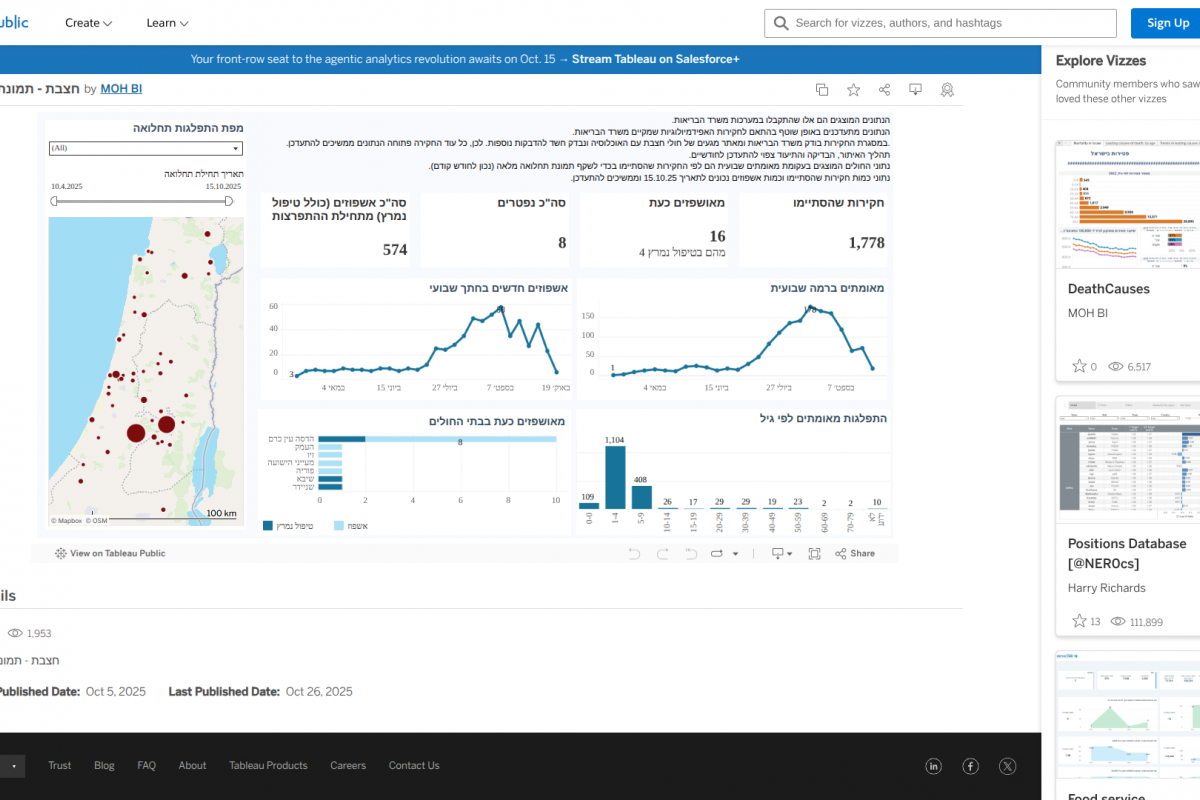
The Nipah virus, one of the world's deadliest viral pathogens, can lead to a variety of clinical outcomes in humans, ranging from asymptomatic infections to severe respiratory illnesses and fatal encephalitis, says the World Health Organization (WHO).
The WHO estimates its case fatality rate for this virus is between 40% and 75%.
During 2025, related fatalities were confirmed in Bangladesh and India.
Unfortunately, no preventive vaccines are available for this virus that is transmitted to humans from bats or pigs as of November 2, 2025.
Recently, a new defense strategy against the Nipah virus has been developed in collaboration with the Coalition for Epidemic Preparedness Innovations (CEPI), the University of Oxford, and the Serum Institute of India Pvt Ltd., the world's largest vaccine manufacturer.
Their goal is to create the largest investigational-ready reserve of a Nipah virus vaccine candidate.
CEPI funding of up to $7.3 million will support SII for process development and manufacturing of the University of Oxford's ChAdOx1 NipahB vaccine candidate.
Dr. Umesh Shaligram, Executive Director, Serum Institute of India, commented in a press release in October 2025, "The collaboration with CEPI and the University of Oxford to develop and manufacture an investigational reserve of the ChAdOx-Nipah vaccine candidate marks a significant step forward in our pandemic preparedness efforts."
"Leveraging our proven manufacturing capabilities and past success with the ChAdOx platform, we are proud to help establish the world's largest investigational reserve against the Nipah virus—one of the deadliest pathogens known. Our aim is to ensure that life-saving doses reach those most in need, particularly across the Global South."
SII will manufacture doses for use in a Phase II clinical trial in a Nipah-affected country, and create an investigational reserve of up to 100,000 doses, which could be deployed under emergency use during a future Nipah virus outbreak, helping to generate critical data and potentially halt an epidemic in its tracks.
SII will supply the Phase II doses to the University of Oxford, which is conducting the clinical trials. These mid-stage trials are set to be the first Phase II trials for a Nipah virus vaccine candidate anywhere in the world.
Earlier in 2025, the CEPI and the U.S. Department of Defense launched a joint effort against Nipah virus treatment and prevention.