Taiwan's Centers for Disease Control (TCDC) recently announced four new locally transmitted cases of dengue fever, one each in Xizhi District of New Taipei City, Fengshan District of Kaohsiung City, and Wandan Township of Pingtung County.
The TCDC estimates that there may be a hidden source of this mosquito-transmitted virus in these communities.
Taiwan's public is urged to cooperate with health authorities' prevention and control measures, implement mosquito-breeding site elimination and control measures, and seek medical attention immediately if they develop suspected symptoms.
According to statistics from the TCDC, as of November 10, 2025, there have been a total of 29 confirmed local dengue fever cases this year, residing in Kaohsiung City (14 cases), Taoyuan City (7 cases), Tainan City (3 cases), Pingtung County (2 cases), Yilan County, Taipei City, and New Taipei City (1 case each).
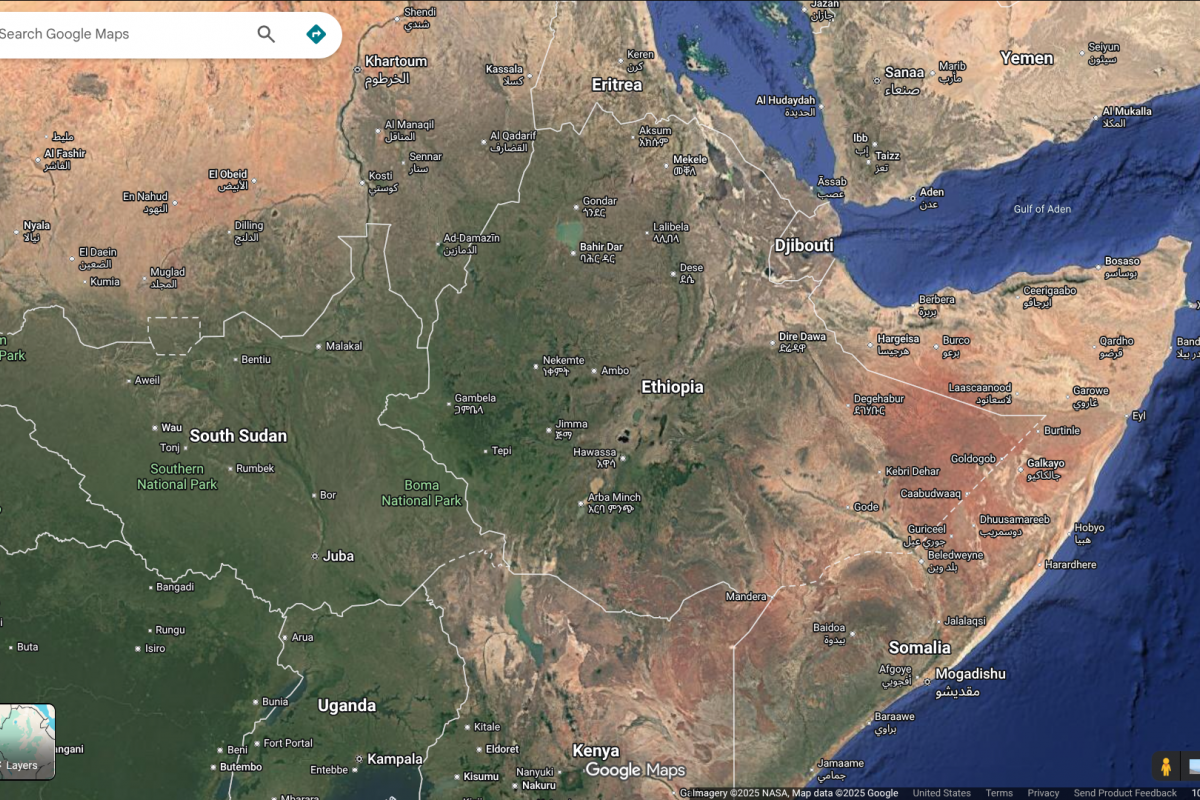
In addition, there have been a total of 223 imported cases, the third-highest number for the same period over the past six years. Most of these cases originated from Southeast Asian countries, with Indonesia (61 cases) being the most common, followed by Vietnam (56 cases), the Philippines (29 cases), and Thailand (23 cases).
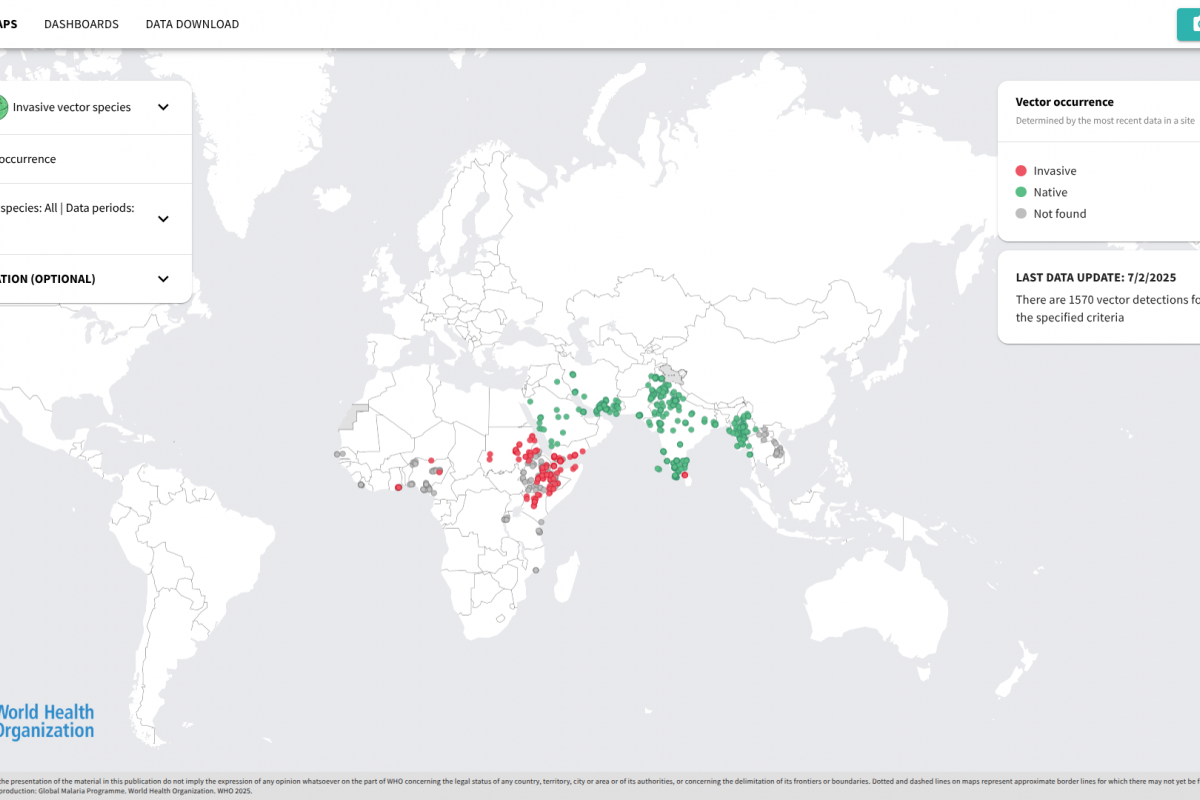
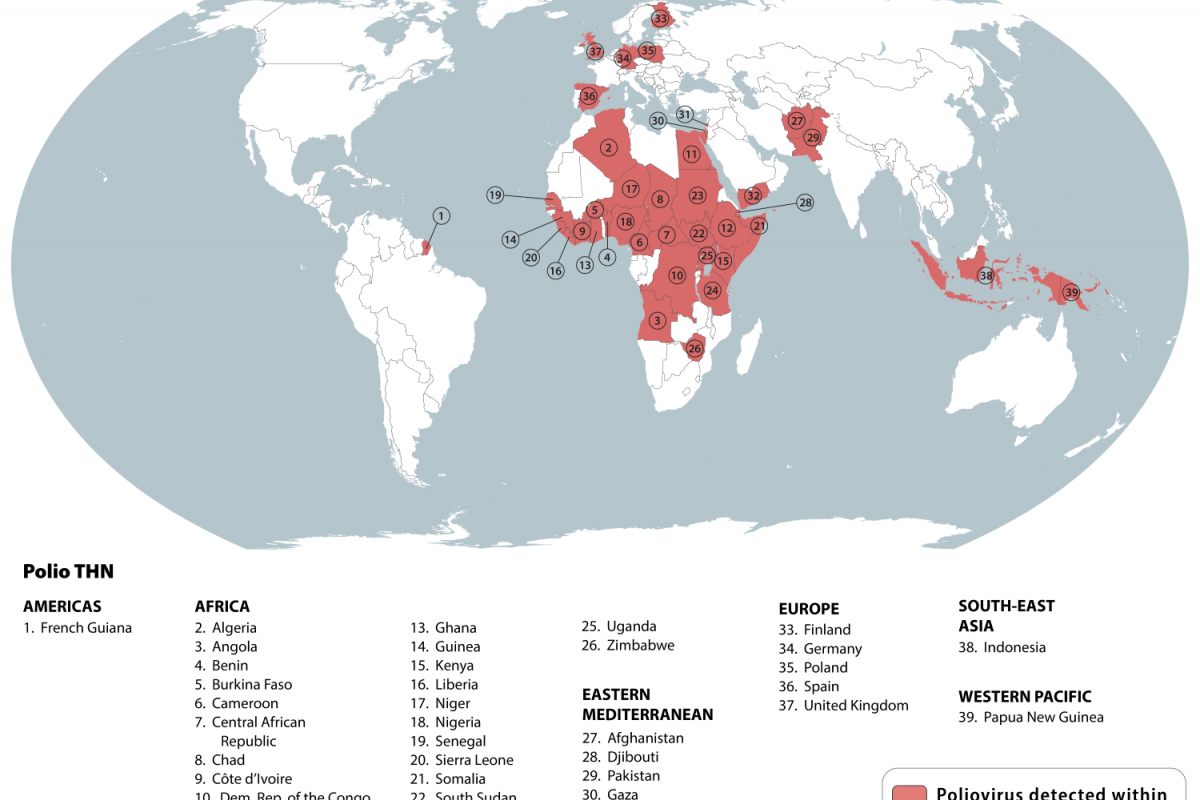
The global dengue fever epidemic continues in 2025, with over 4.43 million cases already reported.
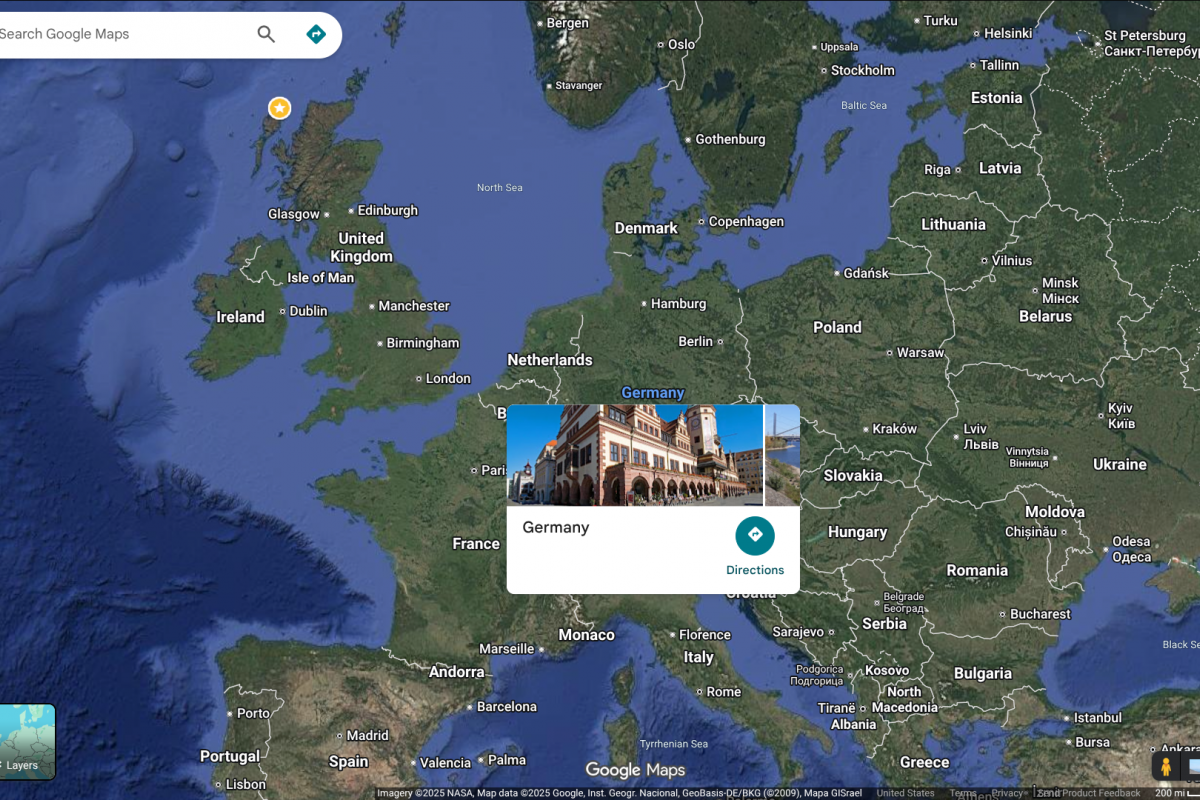
To alert international travelers to their health risk, the U.S. CDC has issued a Travel Health Notice regarding dengue outbreaks. As of November 13, 2025, the CDC has not included Taiwan.
From a disease prevention option, the second-generation QDENGA vaccine is authorized in a total of 41 countries.