In 2025, mainland Europe saw a notably high number of locally acquired chikungunya virus cases, primarily in France and Italy. Chikungunya outbreaks in 2025 highlight the growing health risk of mosquito-borne diseases to residents and visitors in Europe.
This represented a significant increase compared to previous years, driven by the presence of the Aedes albopictus mosquito vector and favorable summer conditions.
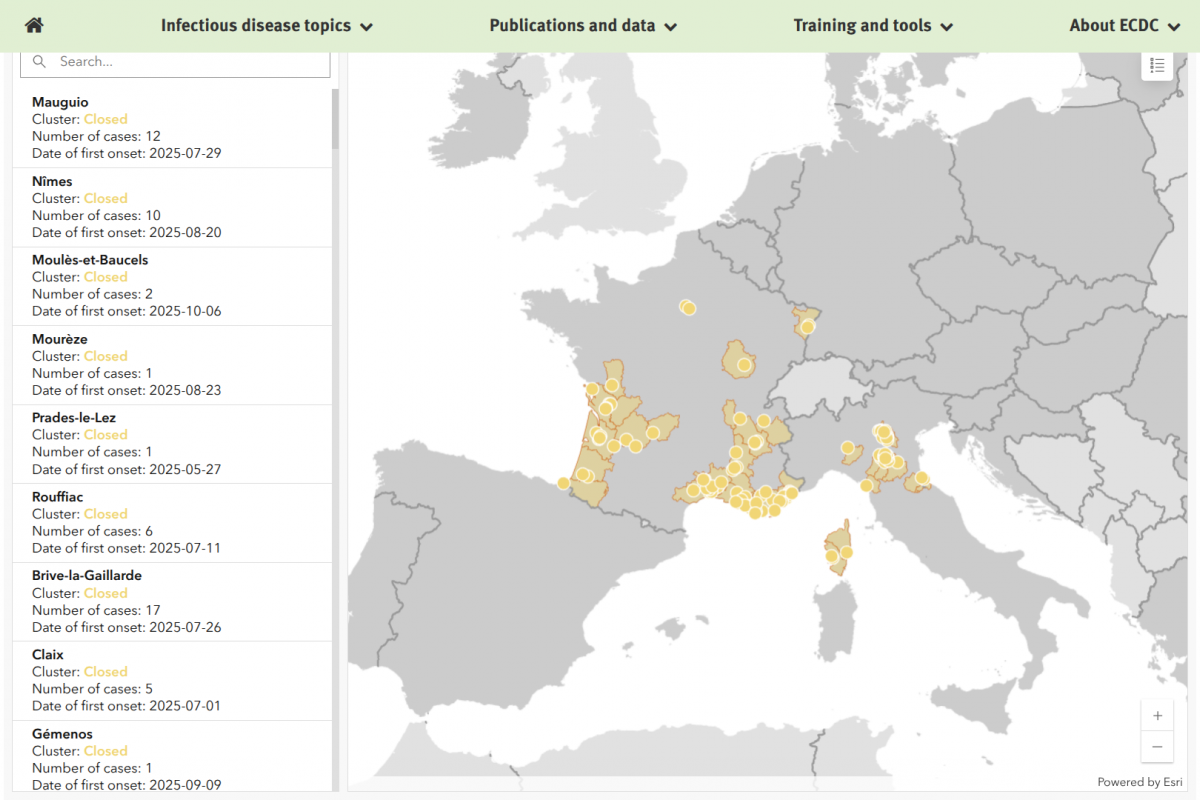
According to the European Centre for Disease Prevention and Control (ECDC) seasonal surveillance report as of December 31, 2025, a total of 788 cases were reported in France and 384 cases in Italy, all locally acquired.
As of January 8, 2026, no new cases have been reported, and all clusters in both countries are now closed. The ECDC has concluded that until weather conditions change, there is minimal risk until the warmer spring or summer months.
As of early 2026, two chikungunya vaccines have been authorized for use in the European Union: IXCHIQ, a live-attenuated single-dose vaccine approved in June 2024, and VIMKUNYA, a non-live virus-like particle vaccine approved in February 2025. Both vaccines protect against the virus, with VIMKUNYA serving as an alternative for those who may not be suitable candidates for live vaccines.
Vaccine availability varies by member state, and vaccination is generally recommended for travelers to endemic areas in France and Italy.
The ECDC says these vaccines represent a crucial tool in preventing future outbreaks amid the expanding presence of mosquito vectors in Europe.
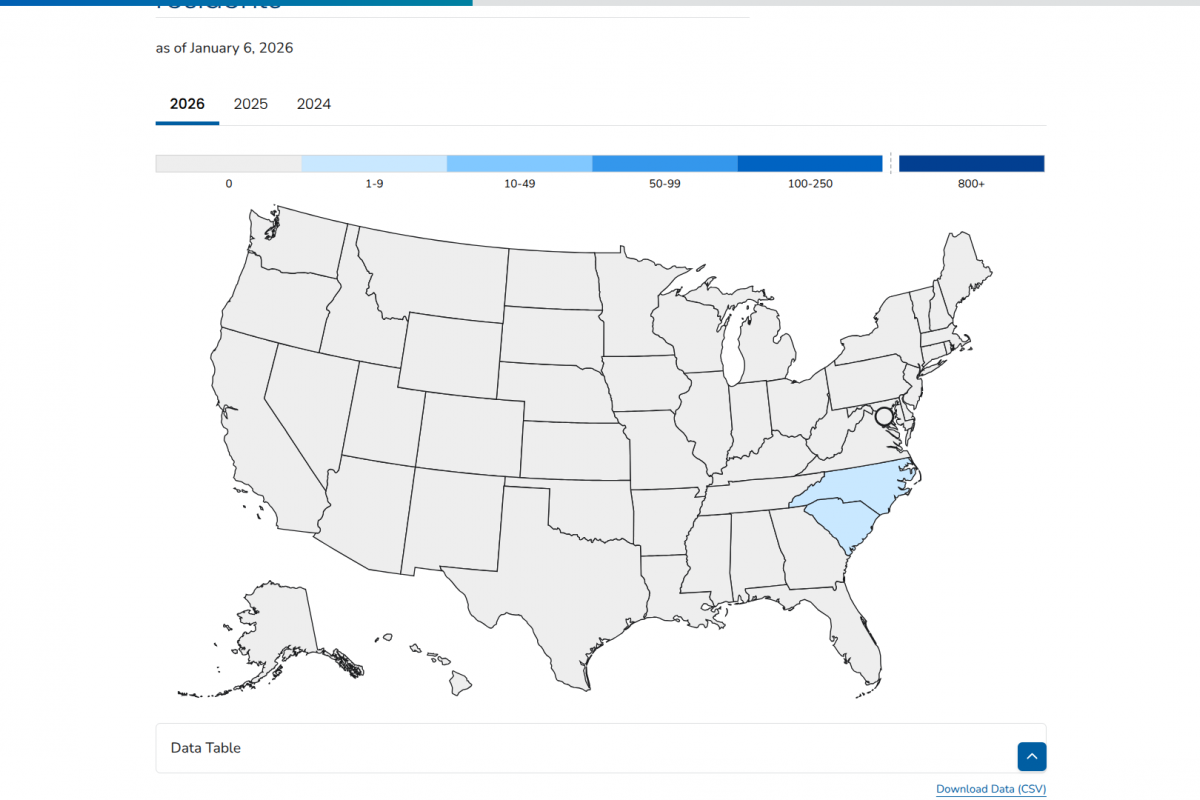
In the United States, chikungunya vaccines are commercailly offered at travel clinics such as Passport Health.