The Pan American Health Organization (PAHO) is urging countries in the Americas to strengthen immunization activities as measles cases continue to rise in the region.
So far in 2025, over 10,000 confirmed measles cases have been reported across ten countries, representing a 34-fold increase compared to the same period in 2024.
On December 15, 2025, the PAHO stated in a press release that these measles outbreaks are linked primarily to low vaccination coverage, with 71% of cases occurring in unvaccinated individuals.
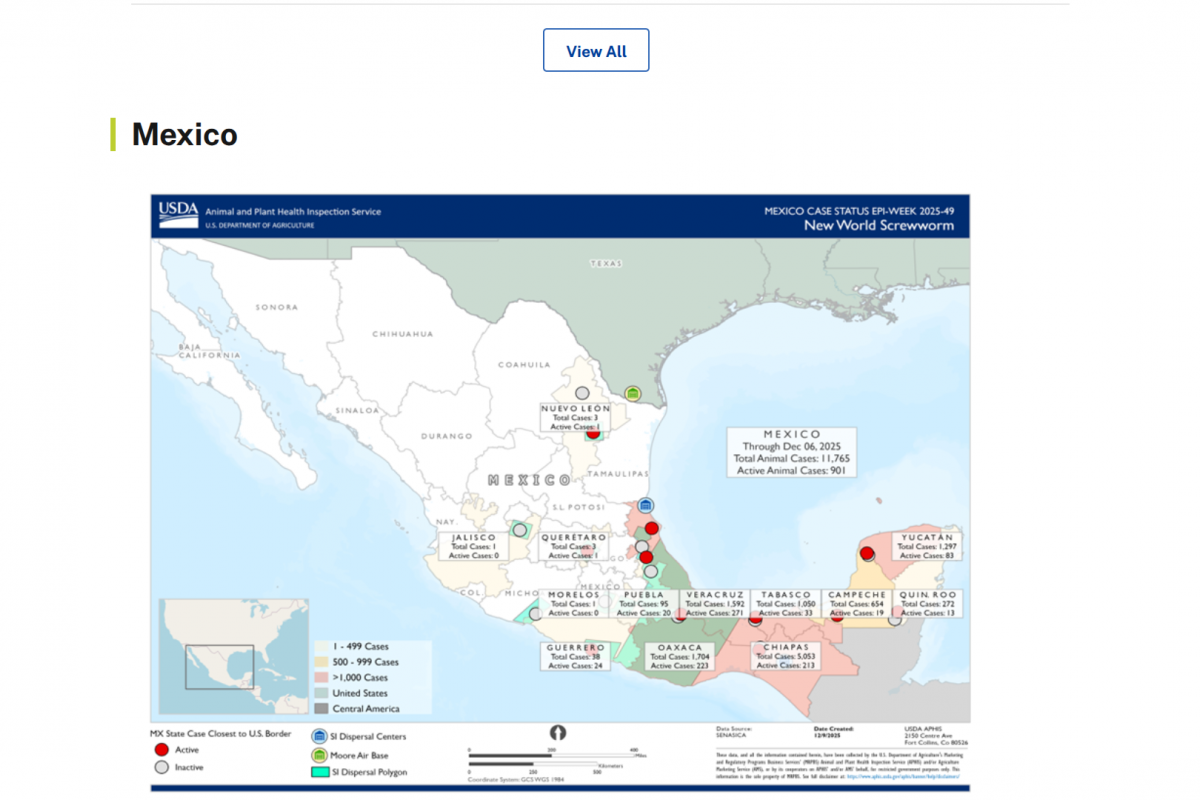
Countries with the highest case numbers include Canada (4,548), Mexico (3,911), and the United States (1,356). Other countries reporting confirmed cases are Bolivia, Argentina, Belize, Brazil, Paraguay, Peru, and Costa Rica.
Mexico leads measles-related fatalities with 14 this year.
"Measles is preventable with two doses of a vaccine, which is proven to be very safe and effective. To stop these outbreaks, countries must urgently strengthen routine immunization and conduct targeted vaccination campaigns in high-risk communities," said Dr. Daniel Salas, Executive Manager of the Special Program for Comprehensive Immunization at PAHO, in a press release.
As of mid-December, Canada lost its measles elimination status after three decades, and Mexico is also at risk of losing its measles-free status in the months ahead.
To alert international travelers to their health risk, the U.S. CDC published a Level 1 Travel Health Notice stating that all international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine.
MMR vaccination services are generally offered throughout the United States at travel clinics and pharmacies.