HPV Screening Produced Better Results Than Pap Smear

Many countries are considering switching from classic Pap Tests to human papillomavirus (HPV) tests for cervical cancer screening.
In Australia, a large clinical trial showed the human papillomavirus test was significantly better at detecting potential precancerous cells than the traditional pap smear.
These research results, published in the journal PLOS Medicine, were released before the transition to Australia’s new national cervical cancer screening program which eliminates scheduling a pap smear every two years.
“We found that the HPV test was substantially more effective at picking up high-grade abnormalities compared to the pap test,” said Prof Karen Canfell, director of research at Cancer Council New South Wales, Australia.
These researchers report a significantly higher detection rate for CIN2+ in HPV-screened women (about 1.0% for HPV-screened women versus 0.1% for cytology-screened women).
"These findings provide initial confirmation of an improved performance of primary HPV screening compared to cytology screening in settings with HPV-vaccinated populations," said Dr. Canfell.
Previous research suggested the new HPV screening program would lower cervical cancer incidence and mortality by at least 20%. But, until this study, this assumption had not been tested on women who had already received the HPV vaccination.
This study was a randomised trial of 5-yearly HPV screening versus 2.5-yearly cytology screening in women aged 25–64 years presenting for routine screening in Victoria, Australia.
HPV testing with partial genotyping of the virus for the highest risk types HPV16 and 18, and cytology (for participants with other high-risk HPV genotypes), or HPV testing with partial genotyping and dual-stained cytology.
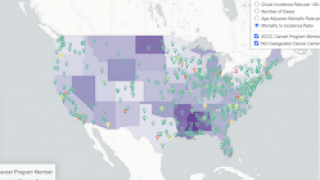
In the USA, the U.S. Preventive Services Task Force (USPSTF) recently reported evidence that screening with cervical cytology or testing for high-risk HPV types (“hrHPV testing”) can detect high-grade precancerous cervical lesions and cervical cancer.
The USPSTF is recommending that primary care clinicians screen for cervical cancer in women 21 to 29 years of age, every three years with cervical cytology, more commonly known as the Pap test.
For women 30 to 65 years of age, the USPSTF recommends either screening with cervical cytology alone every three years or screening with hrHPV testing alone every five years.
In addition, co-testing "increases the number of follow-up tests" by as much as twofold and does not lead to increased detection of CIN3+ (CIN3 and all invasive cancers), so "the USPSTF did not include co-testing in this recommendation statement."
These draft USPSTF recommendations were published on the USPSTF Web site, where comments may be submitted. Public comment on this recommendation statement will be accepted until October 9, 2017.
The Gardasil 9 vaccine immunizes against nine genotypes of HPV known to cause cervical cancer, as well as vulvar, vaginal and anal cancers and genital warts caused by HPV.
This vaccine is an advance over the four-valent HPV vaccine, Gardasil, which was approved by the FDA in 2006.
The CDC Vaccine Price List provides the private sector vaccine prices for general information.
Most pharmacies offer vaccination services, including HPV. Vaccine discounts can be found here.
Research funding: Compass is an investigator-initiated trial which is conducted and funded by the Victorian Cytology Service (VCS) Ltd., a government-funded health promotion charity. The VCS Ltd. have received equipment and a funding contribution for the Compass trial from Roche Molecular Systems and Roche Tissue Diagnostics, AZ USA. KC/MS are also investigators on Compass in New Zealand, ('Compass NZ') (ACTRN12614000714684) which is conducted and funded by Diagnostic Medlab, now Auckland District Health Board. DML received an equipment and a funding contribution for the Compass trial from Roche Molecular Systems. MC, PC, JB, DG, SH, JDB, DH, JT, CDW are also investigators for Compass Australia. KC receives salary support (Career Development Fellowship) from the National Health and Medical Research Council Australia and non-commercial funding from this agency and a number of other sources including the Department of Health Australia and Cancer Council NSW, Australia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interests: KC is Co-PI of an investigator-initiated trial of cytology and primary HPV screening in Australia ('Compass'), which is conducted and funded by the VCS Ltd, a government-funded health promotion charity. The VCS have received equipment and a funding contribution for the Compass trial from Roche Molecular Systems and Roche Tissue Diagnostics, AZ USA. However neither I nor my institution on my behalf (Cancer Council NSW) receives direct funding from industry for this trial or any other project. MS (Co-PI), JB, DG, SH, report that their institution, VCS Ltd, received equipment and funding from Roche Molecular Systems and Roche Tissue Diagnostics, AZ USA, during the conduct of the study. JDB, MC and CJJ (project coordinator, project statistician and senior research assistant) are on the Compass study team. Compass is conducted and funded by VCS Ltd, a government-funded health promotion charity. The VCS have received equipment and a funding contribution for the Compass trial from Roche Molecular Systems and Roche Tissue Diagnostics, AZ USA. However, neither JDB, MC and CJ nor their institution- CCNSW, receive direct funding from industry for this trial or any other project. PEC reports personal fees and non-financial support from Roche Molecular Systems, outside the submitted work. VG has no COIs to disclose. JT and CDW report that VCS Ltd has provided The Department of Oncology & Dysplasia at The Royal Women's Hospital (RWH) monetary support to perform verification colposcopies. JT and CDW were paid to perform colposcopies on Compass participants at the standard public sessional rate, as specified by the RWH and the Victorian Senior Doctors EBA.
Our Trust Standards: Medical Advisory Committee
- Cervical screening with primary HPV testing or cytology in a population of women in which those aged 33 years or younger had pre
- Trial ID ACTRN12613001207707
- Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled tri
- Long term duration of protective effect for HPV negative women: follow-up of primary HPV screening randomised controlled trial
- HPV for cervical cancer screening (HPV FOCAL): Complete Round 1 results of a randomized trial comparing HPV-based primary screen
- Pap Test or hrHPV Test, Choose One, Not Both