Cervical Cancer Risks Reduced by 41% With HPV Vaccine

The number of young women showing early signs of potential cervical cancer have been reduced by 41 percent since the introduction of a school vaccination program.
This research by the University of Aberdeen suggests the vaccine against Human Papilloma Virus (HPV) has seen a significant reduction in abnormal cervical screening tests.
Twenty years earlier than anticipated by researchers..
The study published in the International Journal of Obstetrics & Gynaecology analysed trends in the numbers of Scottish women referred from the cervical screening programme for a colposcopy examination.
Results of this study showed that the women who had been offered the HPV vaccine showed a significant reduction in not only colposcopy, but also medical interventions and treatment compared to those who had not been offered the vaccine.
The UK government introduced the school-based vaccination program in 2008 for girls to protect from HPV virus and specifically against HPV 16 and 18, which cause at least 70% of cervical cancers.
The UK government also offered a three year catch-up programme for girls up to 18 years of age.
The uptake of the HPV vaccine in Scotland is currently among the highest in the world, with around 90% of girls opting to receive it.
We're showing that the HPV vaccination is not only protecting against cancer, but also the immediate risks of the colposcopy and longer term, hopefully, the increased risk of pre-term labour,” said Professor Maggie Cruickshank, from the School of Medicine and Medical Science and Nutrition at the University of Aberdeen, and who led the study.
“This is great news for women as this means they can avoid the short term negative effects of colposcopy such as pain and bleeding, but also longer term, there are concerns that some women treated for pre-cancer changes can have an increased risk of preterm labor.”
Professor Mary Ann Lumsden, Senior Vice President of the Royal College of Obstetricians and Gynaecologists (RCOG), added: “Cervical cancer is the second most common cancer in women below the age of 35.”
“We welcome these extremely encouraging results which reveal a reduction in the number of young women being referred for a colposcopy with early signs of potential cervical cancer – this is most likely due to the HPV vaccination programme’s success. We encourage all girls aged 12 and 13 to take up the vaccine. “
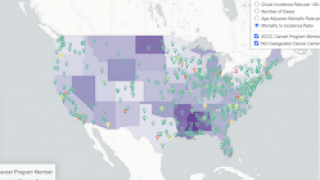
In the USA, HPV is a very common virus, with nearly 80 million people currently infected.
HPV infections are responsible for cancers of the cervix, vagina, penis, tongue, throat and anus, according to the Centers for Disease Control and Prevention (CDC).
The CDC reported 31,500 people are diagnosed with cancer related to HPV each year.
During 2016, the CDC’s Advisory Committee on Immunization Practices approved a two-dose schedule for adolescents under age 15 instead of the traditional three-dose schedule. Teens starting at age 15 or later still need three doses.
The Gardasil 9 vaccine immunizes against nine genotypes of HPV known to cause cervical cancer, as well as vulvar, vaginal and anal cancers and genital warts caused by HPV.
This vaccine is an advance over the four-valent HPV vaccine, Gardasil, which was approved by the FDA in 2006.
The CDC Vaccine Price List provides the private sector vaccine prices for general information. Most pharmacies offer vaccination services, including HPV.
Our Trust Standards: Medical Advisory Committee