Protective Genes Enable Tuberculosis Airborne Transmission
For over 100 years, a vaccine has been deployed 4 billion times to prevent tuberculosis (TB) outbreaks. Unfortunately, versions of the Bacille Calmette-Guérin (BCG) vaccine have only been about 50% protective at reducing severe disease.
To understand this shortcoming and why TB treatments often fail, researchers recently identified genes that the tuberculous bacteria rely on to survive and spread. These genes could help stop the spread of the world's leading infectious disease killer.
They present an introductory study in a series of efforts of increasing technical difficulty to identify the transmission survival genome of Mtb. The identified genes were previously considered unimportant since they appear not to play a role in disease progression when a person is infected.
Instead, the new study suggests that these genes are essential for successful transmission from person to person.
Until this study, very little was known about how tuberculous bacteria survived temperature changes, oxygen levels, humidity, and other environmental factors from one person's lungs to another's.
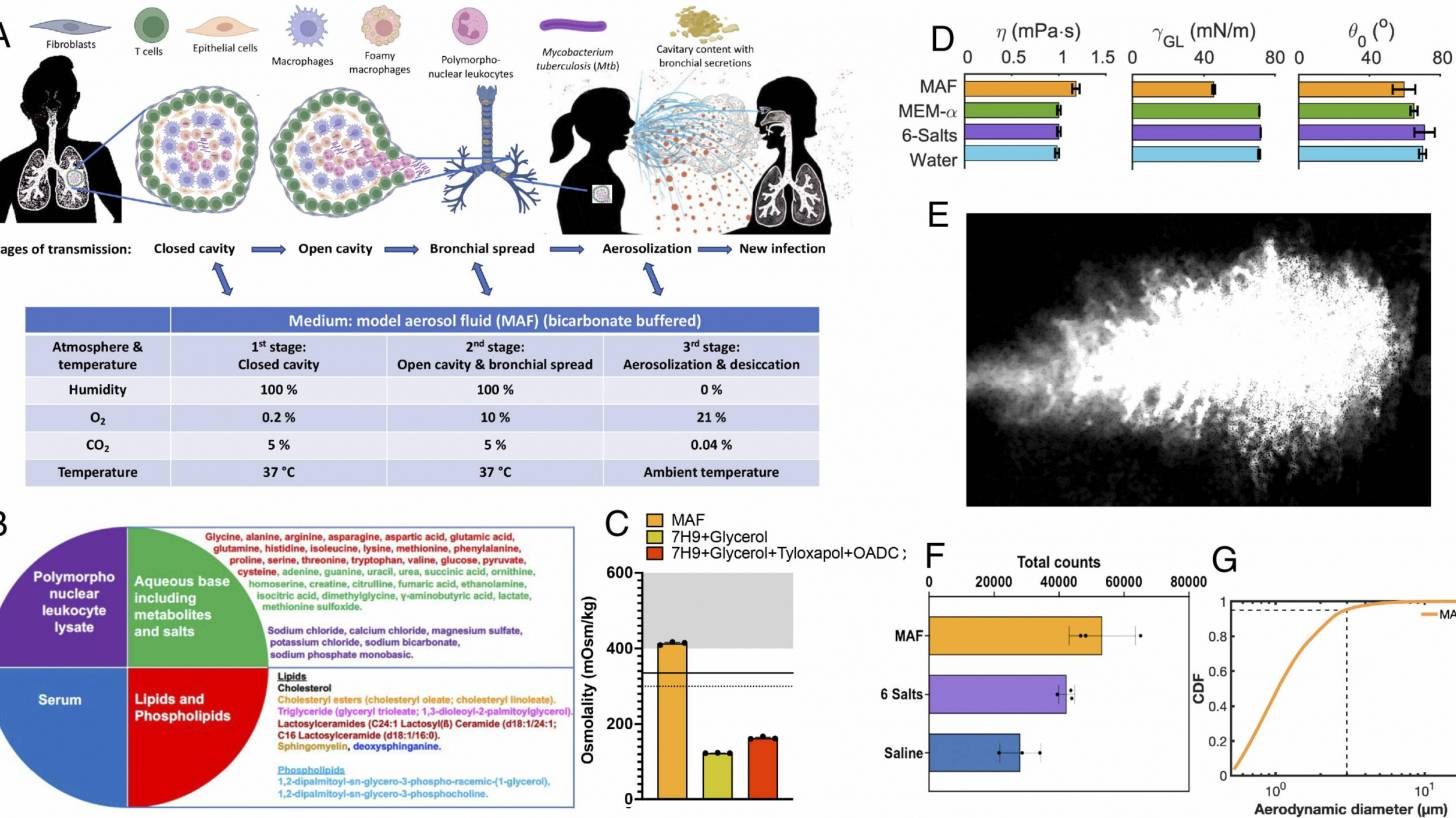
On March 7, 2025, PNAS published a Reach Article by researchers at Weill Cornell Medicine and the Massachusetts Institute of Technology. The article stated that Mycobacterium tuberculosis (Mtb) travels from the lungs of one person through the air to the lungs of another and survives multiple stresses en route, including changes in temperature and concentrations of oxygen, carbon dioxide, hydrogen ions, salts, and organic solutes.
This research presents a genetically tractable transmission model to begin identifying the transmission survival genome of Mtb.
They devised a fluid that mimics TB lesions, found that it protects Mtb from transmission-related stresses, associated this with the structure of the droplets as they dry and their ability to retain water, and used it to query the potential contribution of each of Mtb's genes to Mtb's survival in models of three sequential stages of transmission.
In summary, these studies of MAF as a model for TB lesional fluid are consistent with evidence that Mtb induces the host to provide it with a medium that confers tolerance to some antibiotics. They also reveal that such a fluid can promote the formation of aerosols in a size range consistent with substantial time in the air and access to pulmonary alveoli in new hosts while partially protecting Mtb from death in rapidly shifting environmental conditions before and during its airborne journey.
To the extent that our study of sessile droplets is relevant to aerosol transit, Mtb may depend not only on the host fluid in which it is carried but also on hundreds of its genes.
"The idea of waiting to identify someone with tuberculosis, then treating and curing them, is a inefficient way to stop the pandemic," Carl Nathan, chair of the Department of Microbiology and Immunology and R.A. Rees Pritchett Professor of Microbiology at Weill Cornell Medicine, said in a MIT News article on March 10, 2025.
"Most people who exhale tuberculosis bacteria do not yet have a diagnosis. So, we have to interrupt its transmission. And how do you do that if you don't know anything about the process itself? We have some ideas now."
"Now we have a sense, through these genes, of the tools tuberculosis uses to protect itself."
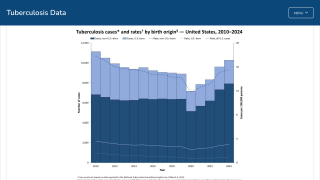
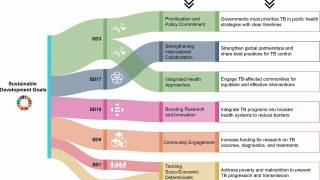
The World Health Organization says most people who developed TB live in the Regions of Southeast Asia, Africa, Europe, and the Western Pacific. Countries such as India (26%), Indonesia (10%), China (6.8%), the Philippines (6.8%), and Pakistan (6.3%) together accounted for 56% of the global TB burden.
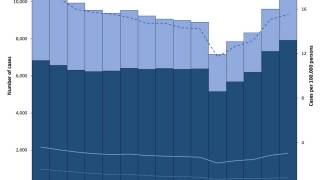
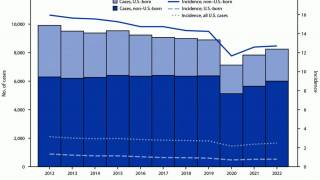
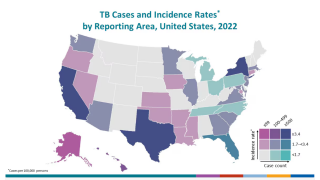
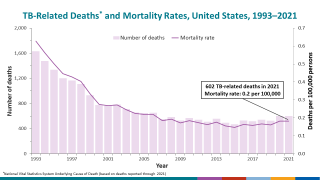
In the United States, TB cases have been increasing for three years, led by California and Texas.
Most of these countries offer various BCG vaccines to children. However, access to the BCG vaccine remains restricted in most states.
Hopefully, with several late-stage clinical trials nearing completion, access to innovative TB vaccines will increase.
Our Trust Standards: Medical Advisory Committee