Malaria Health Alert Issued by the U.S. CDC
The Centers for Disease Control and Prevention (CDC) today announced Health Alert Network (HAN) Health Update (CDCHAN-00496) was issued to share new information about locally acquired malaria cases identified in the United States in 2023.
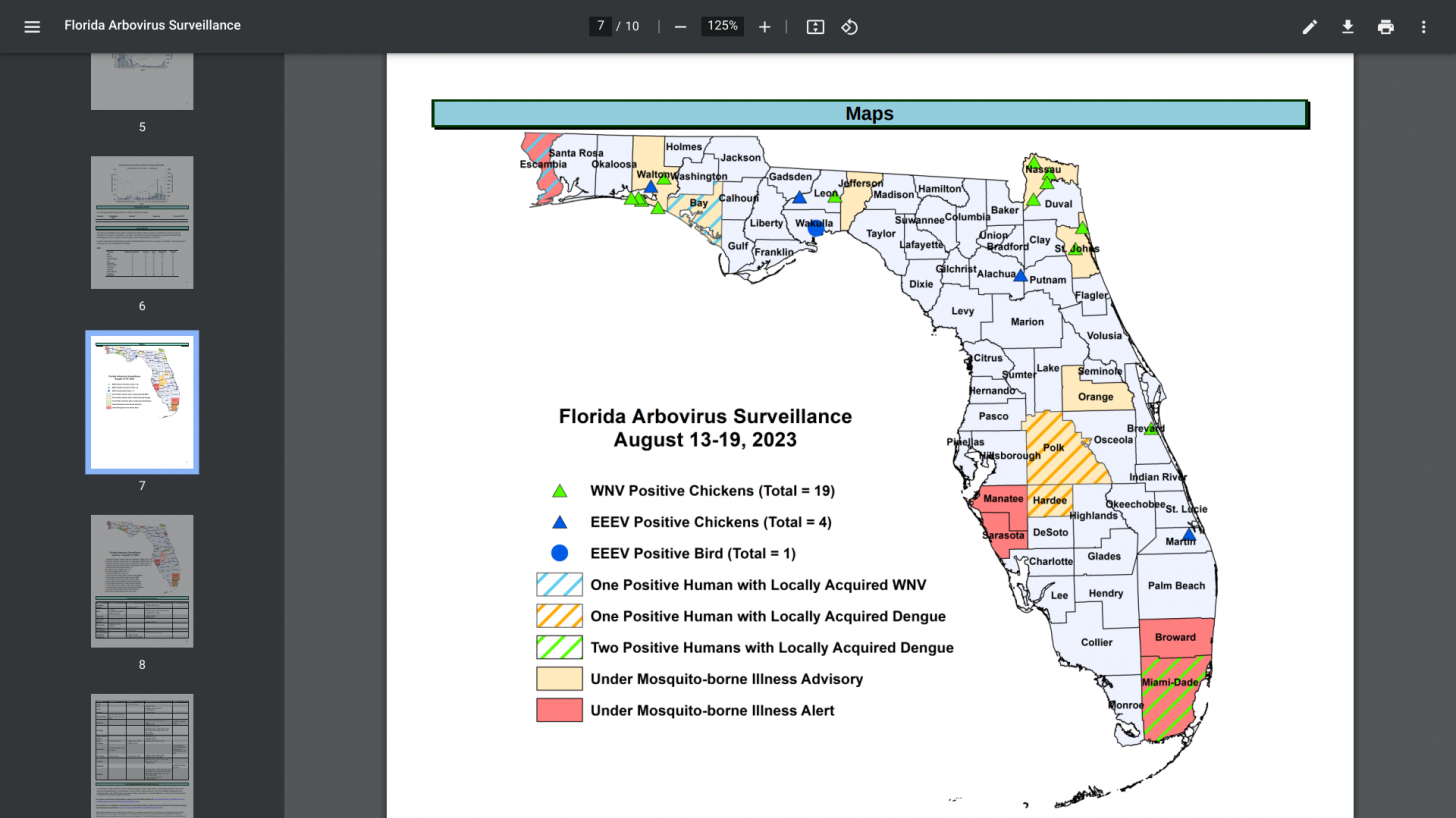
On August 18, 2023, a single case of locally acquired malaria was reported in Maryland in the National Capital Region.
This case was caused by the Plasmodium falciparum (P. falciparum) species and is unrelated to the cases in Florida and Texas described in the HAN Health Advisory 494 issued on June 26, 2023.
As an update to that report, Florida has identified seven cases, and Texas has identified one case of locally acquired P. vivax malaria.
However, there have been no reports of local transmission of malaria in Florida or Texas since mid-July 2023.
The CDC stated on August 28, 2023, that the risk to the U.S. public for locally acquired mosquito-transmitted malaria remains very low.
However, Anopheles mosquito vectors, found throughout many regions of the U.S., can transmit malaria if they feed on a malaria-infected person.
Before 2023, locally acquired mosquito-borne malaria had not occurred in the U.S. since 2003, when eight cases of locally acquired P. vivax malaria were identified in Palm Beach County, FL.
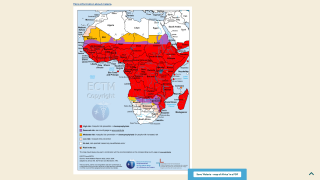
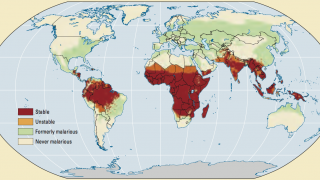
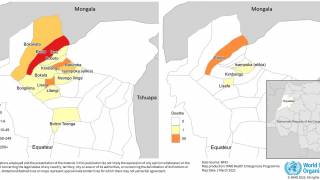
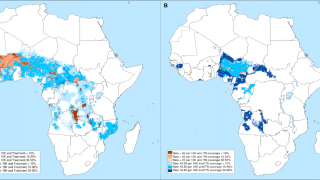
Over 240 million malaria cases worldwide occur yearly (95% in Africa). Almost all malaria cases in the United States are imported and occur in people traveling from countries with malaria transmission.
The CDC's Malaria Program 2023 states that almost half of the world's population is at risk of malaria in 84 countries.
If not quickly diagnosed, P. falciparum malaria can rapidly cause severe illness and even death. Therefore, rapid diagnosis and treatment is imperative.
Clinical manifestations of malaria are non-specific and may include fever, chills, headache, myalgias, and fatigue. Nausea, vomiting, and diarrhea may also occur. Symptoms begin ten days to 4 weeks after infection for most people, although a person may feel ill as early as seven days or as late as one year after infection.
Malaria is a medical emergency and should be treated accordingly.
According to the CDC, patients suspected of having malaria should be urgently evaluated in a facility that can provide rapid diagnosis and treatment as soon as possible, within 24 hours of the patient's presentation.
The most effective way to prevent malaria in the U.S. is for travelers to malaria-endemic areas to take appropriate steps to avoid acquiring malaria while traveling—including taking medications to prevent malaria—and ensuring early diagnosis and treatment of imported malaria cases and preventing mosquito bites.
Artemether-lumefantrine (Coartem®) is the CDC's preferred option, if readily available, for the initial treatment of uncomplicated P. falciparum or unknown species of malaria acquired in areas of chloroquine resistance.
Atovaquone-proguanil (Malarone®) is another recommended option. P. vivax infections acquired from regions other than Papua New Guinea or Indonesia should initially be treated with chloroquine (or hydroxychloroquine).
IV artesunate is the first-line drug for treating severe malaria in the U.S. Artesunate for Injection, manufactured by Amivas, is approved by the FDA for treating severe malaria and is commercially available.
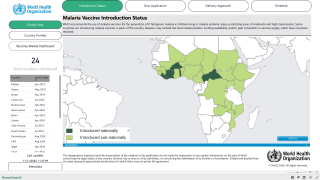
While malaria vaccines are available in Africa, they are not available in the U.S. in 2023.
Our Trust Standards: Medical Advisory Committee