Search API
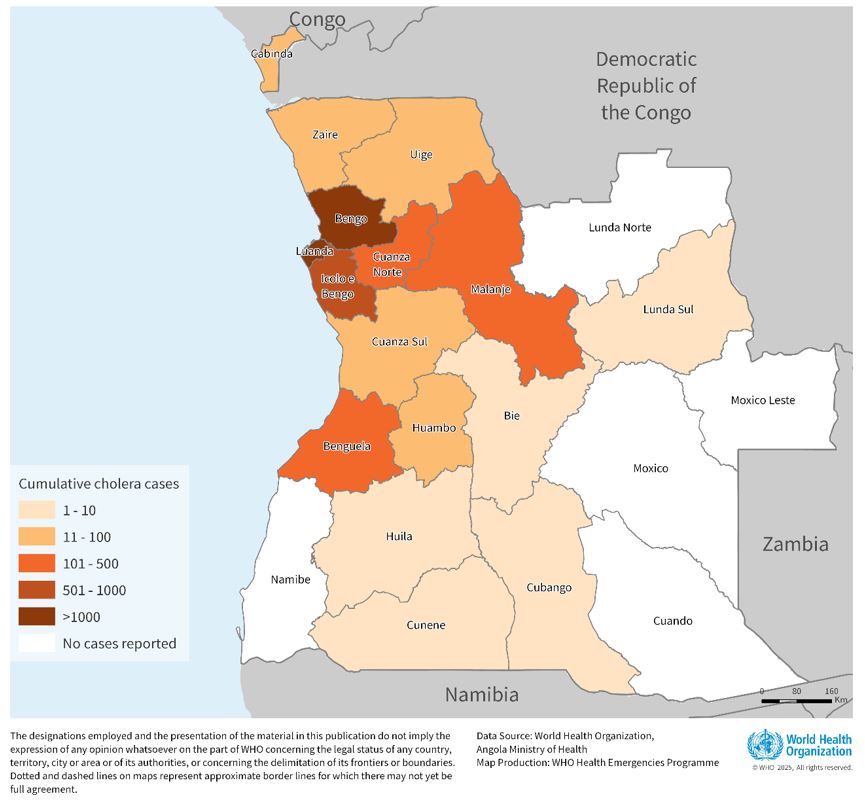
As the seventh cholera pandemic continues in three World Health Organization (WHO) regions in late March 2025, countries in Africa have been severely impacted by these acute diarrheal infections.
Since January 2025, the Republic of Angola has been experiencing a significant cholera outbreak. The disease can cause severe acute watery diarrhea, resulting in considerable morbidity and mortality.
As of March 23, 2025, a total of 8,543 cases and 329 deaths have been reported, resulting in a case fatality rate of 3.9% in this northwestern African country.
The outbreak has spread rapidly to 16 of Angola's 21 provinces, with the highest burden among those under 20.
Angola shares borders with the Democratic Republic of Congo and Zambia, both of which are currently experiencing cholera outbreaks.
As of March 29, 2025, the WHO's Disease Outbreak News wrote, 'Given the rapidly evolving nature of the outbreak, the ongoing rainy season, and cross-border movement with neighboring countries, the WHO assesses the risk of further transmission in Angola and surrounding areas as very high.'
Furthermore, due to the cholera outbreak, the WHO does not recommend travel or trade restrictions to and from Angola.
To reduce this outbreak, Angola's Ministry of Health, with support from others, carried out a five-day reactive vaccination campaign in January 2025. Over 900,000 people were vaccinated, and 700,000 additional doses of oral cholera vaccines arrived in the country in mid-March for a second reactive campaign.
While the U.S. CDC has not issued a Travel Health Advisory regarding Angola's outbreak, the agency writes, 'cholera vaccination may be considered for children and adults traveling to areas of active cholera transmission.'
In the United States, cholera vaccines are offered at travel clinics and pharmacies in 2025.
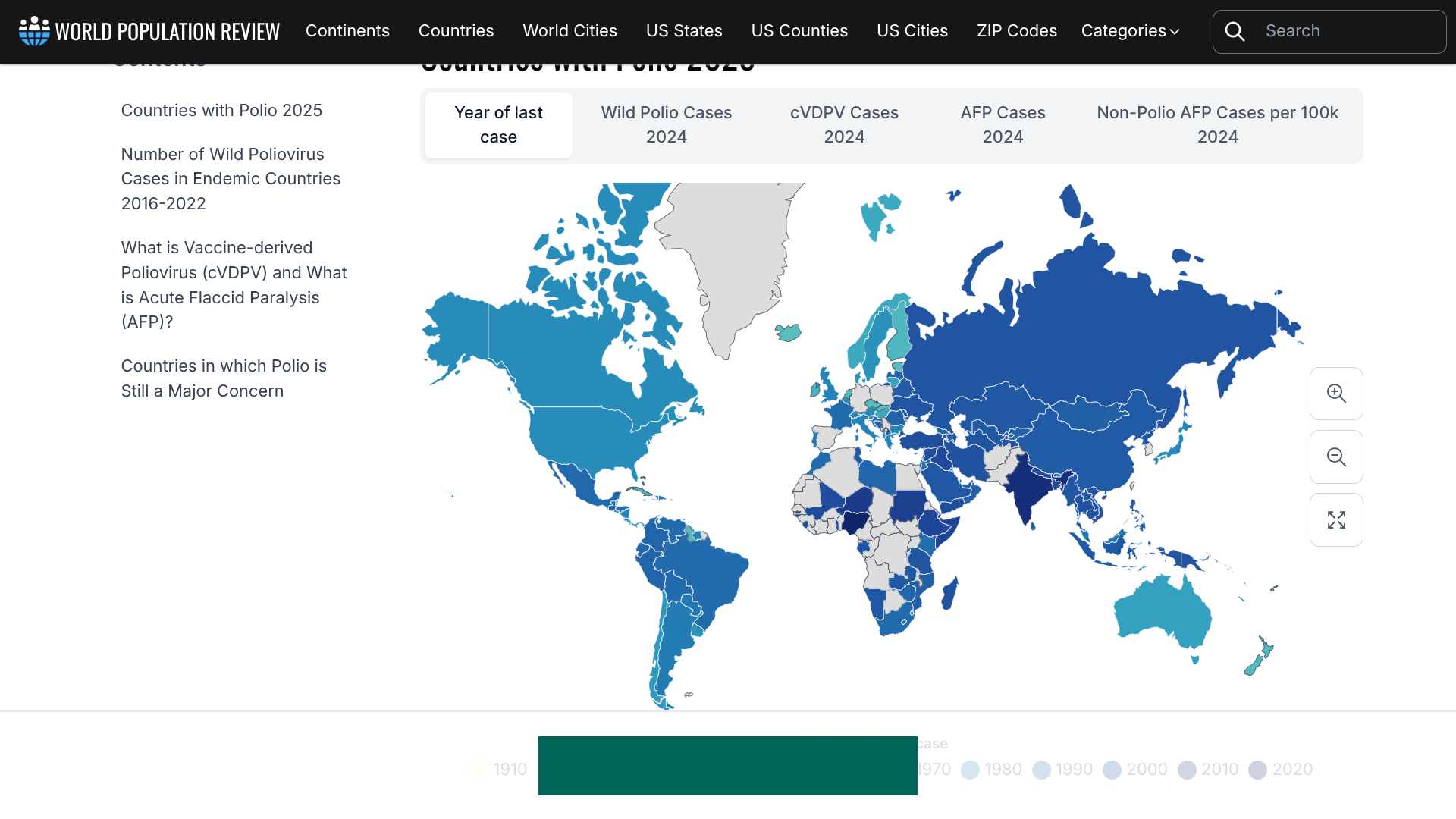
According to the Global Polio Eradication Initiative (GPEI), several countries reported new circulating vaccine-derived poliovirus type 2 (cVDPV2) cases.
Nigeria reported three cases as of March 26, 2025, with onset dates in January and February, bringing its total for 2025 to ten instances. Last year, 98 cVDPV2 cases were reported.
Angola recorded its first case of 2025.
Additionally, GPEI reported that wastewater surveillance in Israel detected a positive cVDPV2 sample collected in the Central province. Genetic analysis indicates that this virus is not related to recent environmental detections in Europe or Gaza, but is most closely linked to a strain that originated in Nigeria's Zamfara state.
Israel is conducting a thorough field investigation to strengthen disease surveillance (including for acute flaccid paralysis cases in health facilities) and identify any residual subnational immunity gaps in this densely populated area.
And in Pakistan, one of two countries in which polio is still endemic, 24 Wild Polio 1-positive environmental samples were recently collected.
The total number of WPV1 cases in 2025 is six. Last year, Pakistan reported 24 WPV1 cases.
As of March 29, 2025, the U.S. CDC recommends international travelers speak with a travel vaccine expert before visiting any polio-risk area.
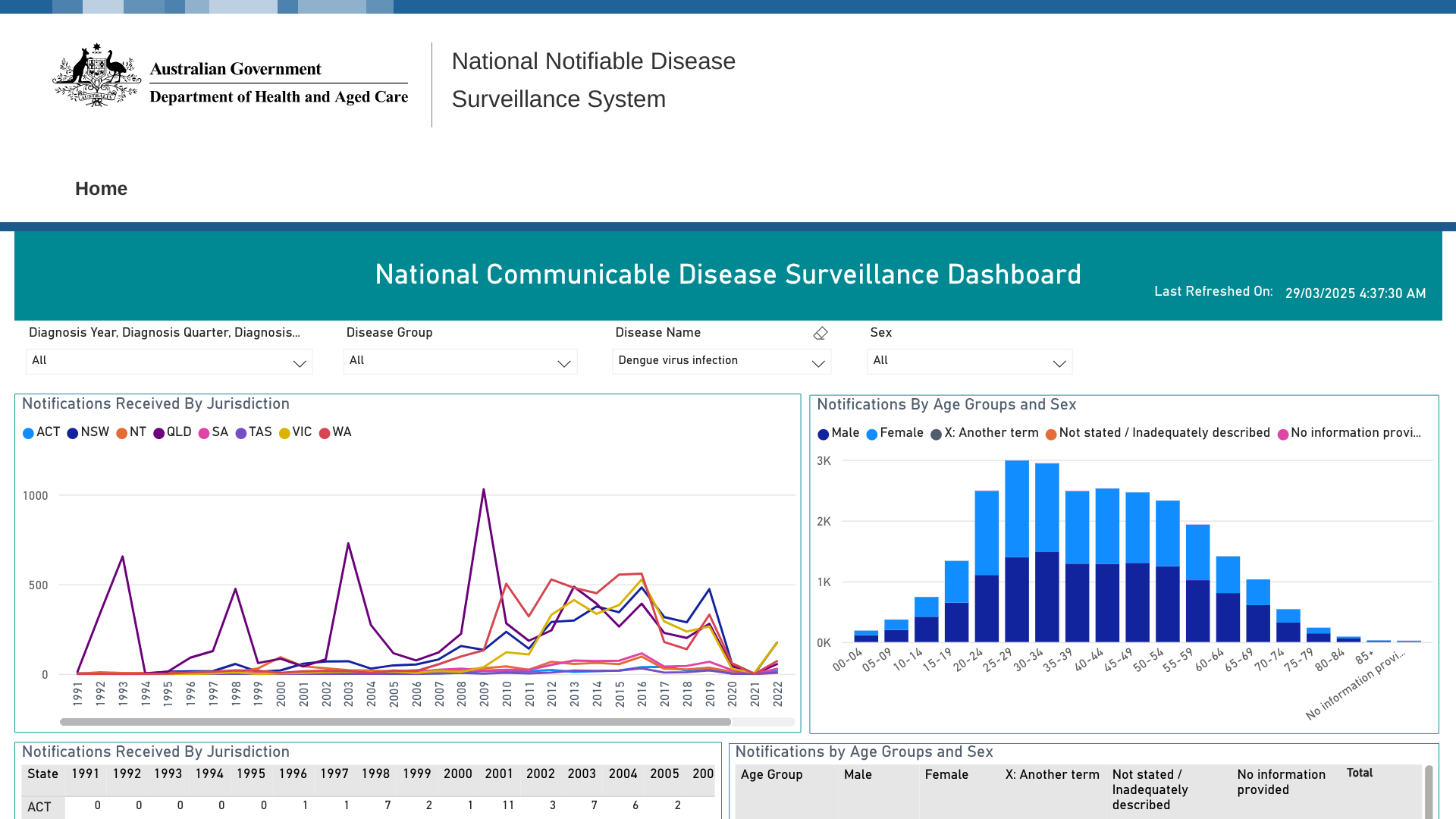
Historically, most mainland Australian states have reported cases of locally acquired dengue fever. In January 2025, 261 notifications of dengue cases throughout Australia were received.
So far this year, the disease has significantly impacted Australia's northeast coast.
Queensland Health declared a Dengue outbreak centered in Townsville City LGA on February 19, 2025, and as of March 25, 2025, 11 cases (9 confirmed, two probable) had been reported.
Townsville Public Health Unit director Dr Steven Donohue said in a recent press release that they have started a full-scale dengue outbreak response.
Teams from Townsville HHS and Townsville City Council are talking to residents in nearby homes in North Ward to warn them of the dengue outbreak, inspect their properties, and carry out any mosquito-mitigation activities," Dr Donohue said.
"It is important for residents to take dengue precautions."
"Therefore, it's imperative to tip out anything holding water around your house. They'll breed in junk, tyres, and pot plant bases. Tip those out. Have a dry yard as much as possible.
"Make sure to spray dark, damp hiding places inside your house. Use surface spray or long-acting insecticide – under the sink, in the bathroom, or the laundry, all of those hiding places. That's a great way to get rid of these mosquitoes."
Dr. Donohue added that it is vital for anyone feeling unwell to see a doctor.
As of March 29, 2025, dengue vaccines are authorized in Australia and most Asia / Pacific countries.
According to recent data from Japan's public health institute, the number of infectious gastroenteritis cases caused by norovirus and other pathogens in Japan has reached the highest level in ten years.
As of mid-March 2025, there were 34,609 norovirus cases reported by the National Institute of Infectious Diseases.
According to Japan's Ministry of Health, Labor and Welfare, most reported cases of infectious gastroenteritis are viral, primarily affecting infants and school-age children.
Like "infectious diarrhea" in Western terminology, norovirus is classified as a causative pathogen and a foodborne infection.
Historically, norovirus cases in Japan are detected in early winter, peak in December due to viruses like RSV, have a smaller peak in spring associated with rotavirus, and continue into early summer.
Bacterial infections, such as Vibrio parahaemolyticus, are more common in summer.
In summary, the Ministry says these infections can be categorized as sporadic or epidemic diseases in the region or as part of foodborne infectious diseases.
The U.S. CDC says norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis and stomach inflammation among people of all ages in the U.S.
Norovirus causes 58% of foodborne illnesses acquired, resulting in about 900 deaths, mostly among adults aged 65 and older, each year.
Furthermore, the CDC has reported 12 norovirus outbreaks on cruise ships. In 2024, 18 norovirus outbreaks were confirmed on U.S.-based cruises.
As of March 28, 2025, the U.S. government has not approved a norovirus vaccine for commercial use.

Even with a vaccination requirement to visit most Yellow fever endemic countries, the Pan American Health Organization (PAHO) has issued a new Epidemiologic Alert regarding increased human cases in 2025.
As of March 26, 2025, the PAHO wrote that health officials have confirmed 131 Yellow fever (YF) cases in four countries, 53 of them fatal, indicating a 40.4% case-fatality rate.
Brazil has 81 confirmed cases, 31 of which have been fatal.
The other YF cases have been reported in the Plurinational State of Bolivia, Colombia, and Peru.
In 2025, YF cases have also been detected in the state of São Paulo in Brazil and the department of Tolima in Colombia, regions outside the Amazon region.
The PAHO/WHO wrote 'It is essential that countries achieve vaccination coverage of at least 95% in populations in at-risk areas, in a homogeneous manner, and that health authorities ensure that they have a strategic reserve inventory that allows them to maintain routine vaccination and, at the same time, respond effectively to possible outbreaks.'
When departing to South America from the United States in March 2025, YF vaccination services are offered at most travel clinics and pharmacies. Once immunized, a certificate that is essential to enter certain countries will be generated.

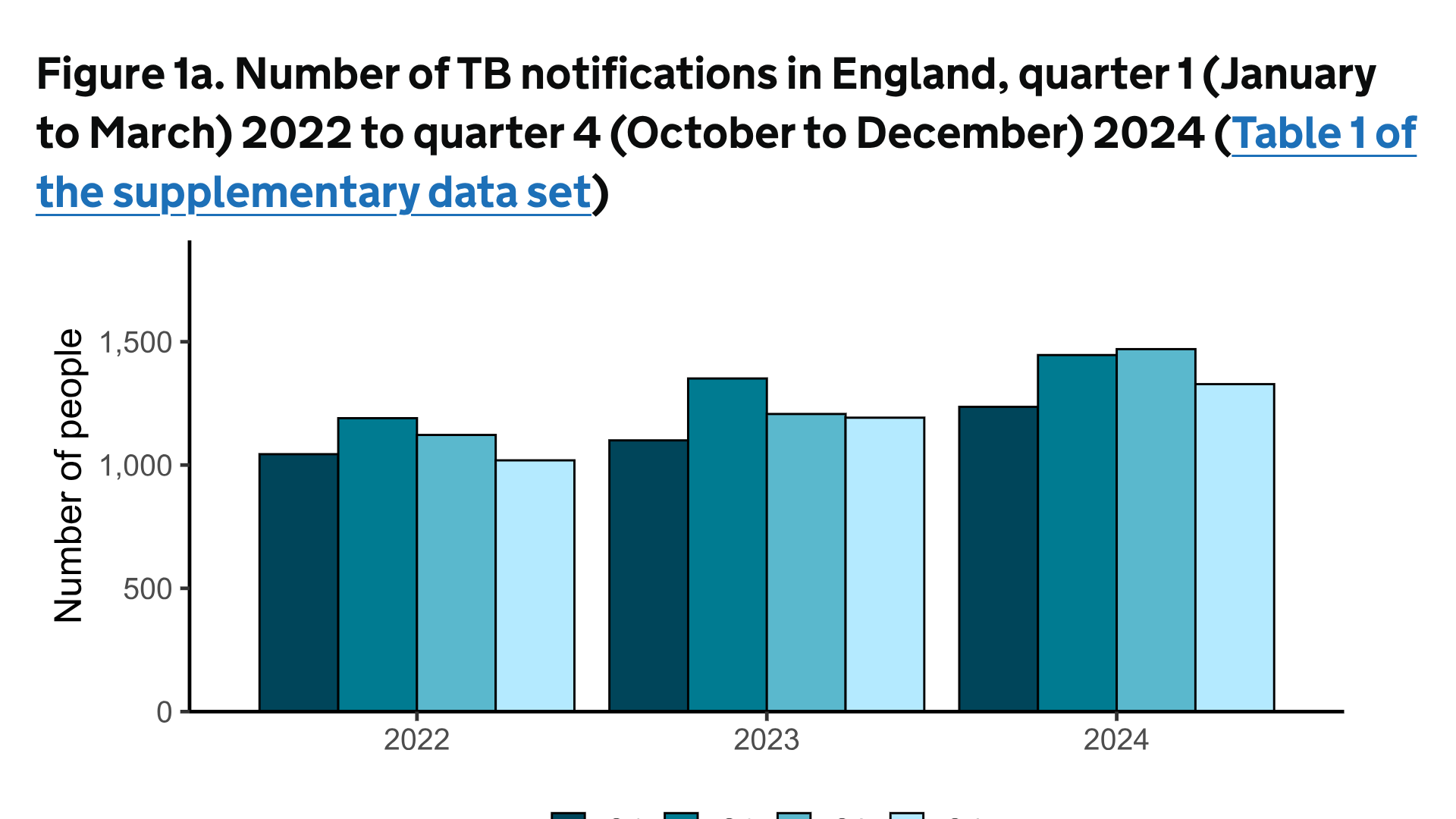
Tuberculosis (TB) is the leading cause of death from a single infectious agent worldwide, including in England.
The UK Health Security Agency (UKHSA) report announced on March 24, 2025, reveals that TB remains a significant public health concern in England.
Data indicates that reported TB notifications increased by 13% in 2024, from 4,850 to 5,480 people, compared with 2023.
The most significant geographic increases were in London and the West Midlands
The UKHSA writes, ' If this rate of increase persists, the UK risks losing its WHO low incidence status of 10 cases per 100,000 population.'
According to the UKHSA, there is a strong association between the increase in TB incidence and the rise in migration, with about 81% of all notifications in 2023 coming from people born outside the UK. Work is underway to identify the optimal and most cost-effective control and prevention strategies to tackle this increase.
One tactic to reduce TB cases in children listed by the UKHSA is to optimize the use of Bacillus Calmette–Guérin (BCG) vaccines provision through commissioning and specification to include vaccinating infants at four weeks of age. While about 50% effective, BCG vaccination is an inexpensive defence against treating TB cases.
The global average cost for BCG vaccination is about $5.00. According to USAID, treating a tuberculosis case in the U.S. costs about $20,000, and a drug-resistant tuberculosis case can cost over $150,000.
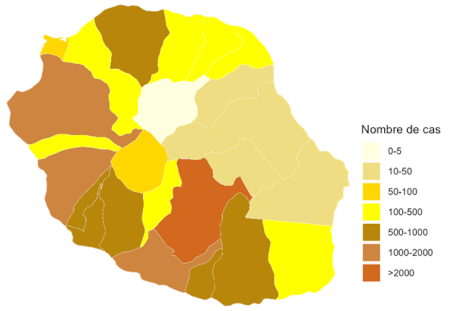
The French Republic's overseas department and region of Réunion today reported a serious spike in Chikungunya cases. Over the last week, 4,156 new cases were reported.
This data indicates a 16% increase in Chikungunya cases compared to the previous week.
Furthermore, emergency department activity increased from 78 admissions the previous week to 128 during March 10-16, 2025.
During early March, Réunion health authorities announced two virus-related deaths.
Since this Chikungunya outbreak began in August 2024, 13,594 cases, 15 serious cases (eight adults and seven newborns) have been reported, setting an unfortunate record for a French department or region.
Réunion's southern and western municipalities are the most affected. Le Tampon remains the most affected municipality.
However, this mosquito-transmitted virus has increased sharply in Possession, Saint Andrew, Saint Paul, and Saint Suzanne.
As part of the Mascarene Islands, Réunion is a vacation destination for many travelers. It is located east of Africa, Madagascar, and southwest of Mauritius.
France has issued a Level 4 emergency for Réunion to alert visitors of this health emergency, and the U.S. CDC issued a Level 2 Advisory regarding La Réunion's Chikungunya outbreak.
To reduce the impact of this outbreak, Valneva SE and the Agence Régionale de Santé La Réunion recently announced an agreement to deliver at least 40,000 IXCHIQ® vaccine doses starting in early April 2025. The French government funded this purchase.
In the U.S. and various countries, Chikungunya vaccines are approved and available at travel clinics and pharmacies. They are recommended for international travelers visiting endemic countries such as La Réunion.
As sexually transmitted diseases continue to spread in 2025, a new vaccine candidate may reduce the number of chlamydia cases in the United States. Current programs to prevent infection rates from rising have proven insufficient, highlighting the urgent public health need for a vaccine.
Sanofi announced today that the U.S. Food and Drug Administration has granted a fast-track designation to Sanofi's mRNA vaccine candidate for preventing chlamydia infection.
The chlamydia vaccine candidate has been designed to protect against primary genital tract infection and reinfection by the bacterium Chlamydia trachomatis.
In 2020, there were 129 million worldwide cases of chlamydia among adults and adolescents, with the highest rates of infection among younger people.
Jean-François Toussaint, Global Head of Vaccines R&D, stated in a press release on March 26, 2025, "Millions of people currently live with undiagnosed chlamydia, including asymptomatic infection that can also cause severe long-term health effects if left untreated."
"Antibiotics to treat chlamydia have not been successful in controlling rising infection rates. With our program, we aim to make chlamydia a preventable disease through vaccination."
Following a promising preclinical program, Sanofi is planning a phase 1/2 randomized clinical study to evaluate the immunogenicity and safety of the chlamydia vaccine candidate in adults aged 18 to 29.
This clinical study is due to start in the coming days.
Chlamydia, caused by the bacterium Chlamydia trachomatis, is a common bacterial infection of the reproductive tract with consequences for developing infertility and pregnancy complications.
Although chlamydia can be treated with antibiotics when diagnosed, over 80% of chlamydia cases are asymptomatic, meaning there is a significant risk that infections go unrecognized, leading to untreated cases and unintentional transmission.
A study published by the Annals of Family Medicine on March 24, 2025, indicates that many women are not receiving guideline-adherent treatment in primary care settings. For example, the time to treat chlamydia was longer for patients aged 50-59 years (time ratio relative to those aged 20-29 years = 1.61; 95% CI, 1.12-2.30).
The development of this vaccine candidate is part of the Translational Science Hub, a partnership with the Queensland Government, Griffith University, and the University of Queensland that connects world-class researchers in Queensland, Australia, with Sanofi scientists in France and the U.S.
As of late March 2025, the FDA, the United Kingdom, and the European Medicines Agency have not approved a vaccine to prevent chlamydia infections.