EU Countries Reporting Increased Hep A Cases

The European Centers for Disease and Control (ECDC) reported large increases in hepatitis A cases during the first half of 2017. And, that these hepatitis A (HAV) outbreaks across Europe most likely have not reached their peak.
EU countries reporting hepatitis A outbreak-related cases are Austria, Belgium, Denmark, Finland, France, Germany, Ireland, Italy, the Netherlands, Norway, Portugal, Slovenia, Spain, Sweden and the United Kingdom.
In Spain, as example, hepatitis A cases reported in 2017 are almost eight times higher than the average number of cases reported during the same period between the years 2012 and 2016.
The ECDC stresses the importance of hepatitis A vaccination as a main option to avoid new infections. These new cases are mainly affecting men who have sex with men.
Additionally, several EU countries are experiencing hepatitis A vaccine shortages. Austria, Italy, Portugal and Spain are facing immediate vaccine shortages.
Which means, according to the ECDC, countries should allocate their limited supply of vaccines to higher risk of infection groups.
"As suggested in our latest rapid risk assessment, further transmission may be prevented by vaccination of men who have sex with men and post-exposure prophylaxis among contacts of those infected", said ECDC Acting Director Andrea Ammon. “But, limited vaccine availability in some countries may however have an impact on the implementation of such control measures."
Hepatitis means inflammation of the liver. This condition is most often caused by a virus.
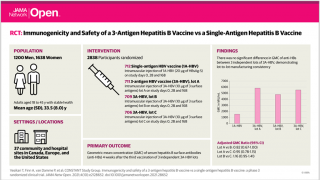
In the United States, the most common causes of viral hepatitis are hepatitis A virus (HAV), hepatitis B virus (HBV), and hepatitis C virus (HCV). HBV and HCV are common among people who are at risk for, or living with, HIV.
You can get some forms of viral hepatitis the same way you get HIV—through unprotected sexual contact and injection drug use.
Hepatitis B virus and HIV are blood-borne viruses transmitted primarily through sexual contact and injection drug use. Because of these shared modes of transmission, a high proportion of adults at risk for HIV infection are also at risk for HBV infection.
There's no vaccine to prevent HIV infection and no cure for AIDS.
But it's possible to protect yourself and others from both hepatitis and HIV infections.
That means avoiding any behavior that allows HIV-infected fluids, such as blood, semen, vaginal secretions and breast milk, into your body.
Our Trust Standards: Medical Advisory Committee