Search API
Now in its third decade of serving travelers in Central Texas, Austin–Bergstrom International Airport welcomed over two million visitors last month, many of whom arrived from overseas.
Unfortunately, this year, eight visitors to Travis County, and Austin, Texas, contracted the Dengue virus while traveling abroad.
Last year, Travis County reported 18 travel-related cases of Dengue, the most in Texas.
According to the Texas Department of State Health Services' (DSHS) arbovirus weekly report #36, there have been 31 travel-related Dengue cases reported in Texas this year.
This news is relatively positive compared to 2024, when 143 imported Dengue cases and one related fatality occurred across 23 Texas counties.
Texas is not alone in reporting fewer Dengue cases in 2025.
Throughout the United States, 3,045 cases of mosquito-transmitted Dengue have been confirmed this year.
In 2024, 53 U.S. jurisdictions reported 9,391 Dengue cases.
Only a few states, such as Florida, reported locally acquired Dengue cases last year.
And in the Region of the Americas, as of epidemiological week 34, a total of 3,740,133 suspected cases of Dengue were reported in 2025. This data represents a 68% decrease compared to the same period in 2024.
To enhance disease detection, the U.S. Centers for Disease Control and Prevention (CDC) advised clinicians in July 2025 to consider Dengue in patients with fever who live in or have recently traveled to areas with a risk of Dengue.
Furthermore, to alert international travelers to this health risk, the CDC reissued a Global Travel Health Notice on August 21, 2025, regarding Dengue outbreaks in the Americas, Africa/Middle East, and Asia/Pacific regions, in countries such as India, Singapore, Thailand, the Philippines, Malaysia, and Myanmar.
From a disease prevention perspective, the CDC says mitigating mosquito bites is the best option, as access to Dengue vaccines in the USA is currently limited to children in Puerto Rico.

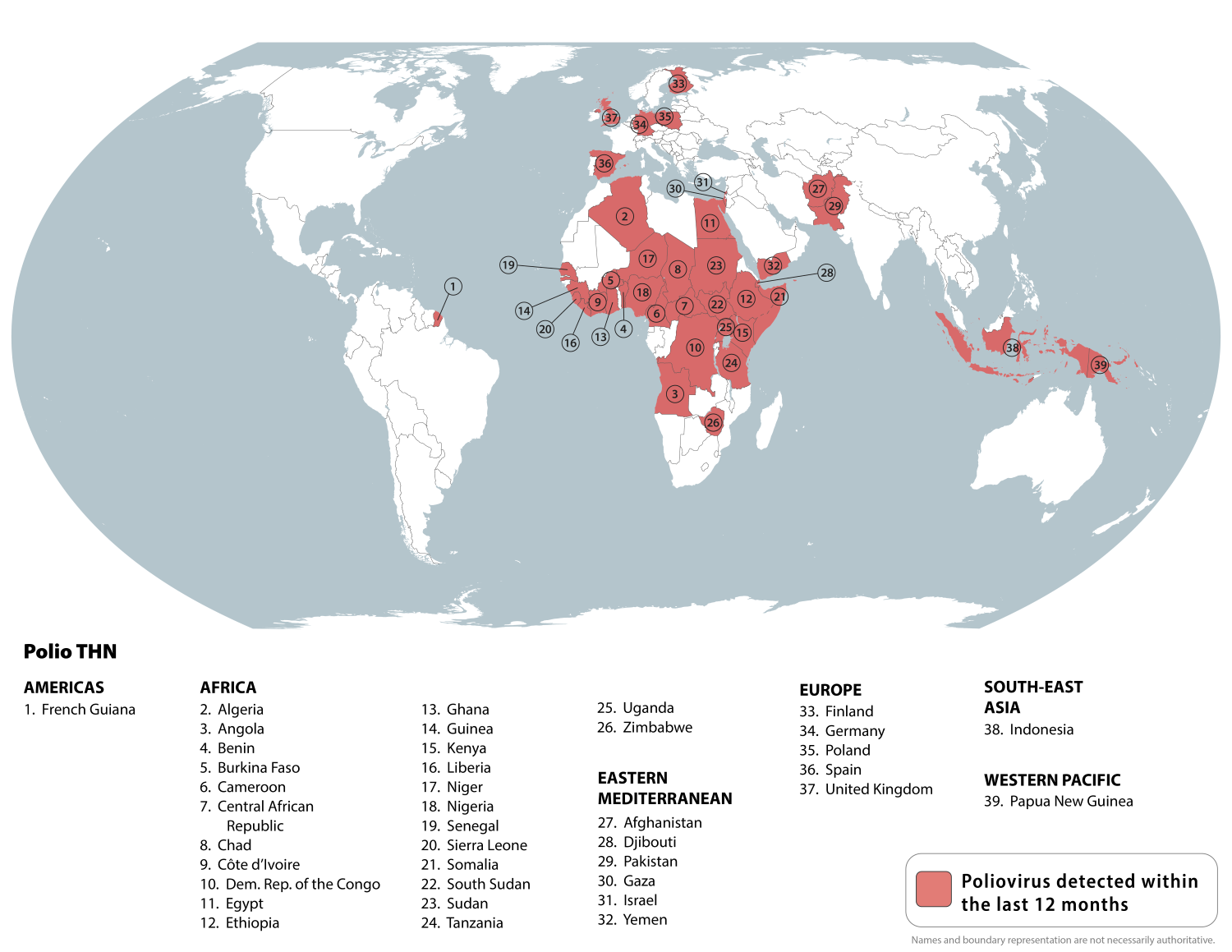
According to the latest weekly update from the Global Polio Eradication Initiative (GPEI), three countries have reported new cases of polio.
As of September 15, 2025, the GPEI confirmed that Chad, Nigeria, and Somalia reported vaccine-derived poliovirus types.
In the Federal Republic of Nigeria, four cVDPV2 cases were reported this week, two from Sokoto, and one each from Zamfara and Kaduna.
The total number of cases reported in Nigeria this year is 28. The number of cases from 2024 remains 98.
To alert international travelers of this serious health risk, the U.S. CDC published a Level 2 - Practice Enhanced Precautions, Travel Health Advisory in August 2025. In total, the CDC identified 39 countries where poliovirus has been identified.
The CDC advises that before traveling to any destination listed below, adults who previously completed the whole, routine polio vaccine (IPV) series may receive a single, lifetime booster dose of polio vaccine.
Polio vaccination services are offered at travel clinics and pharmacies in the USA.
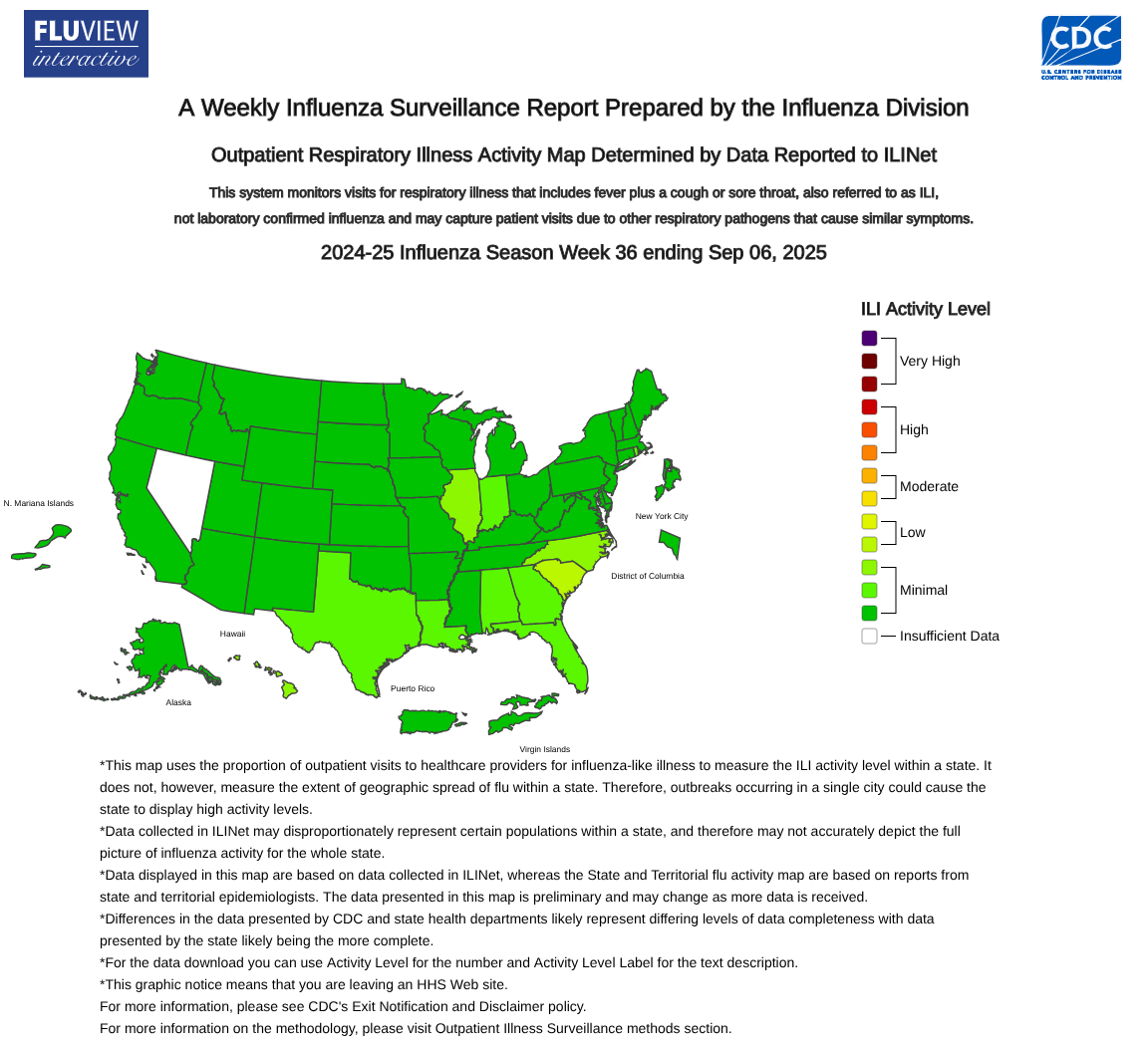
Since the summer of 2025 has ended, and most children have returned to school, parents are asking when the best time is to get the annual flu shot. Since it takes a few days for influenza vaccines to take effect, timing is a crucial factor.
To help guide answers, the U.S. Centers for Disease Control and Prevention (CDC) recently published the results of tests performed by clinical laboratories nationwide.
Nationally, during Week 36, the percentage of respiratory specimens testing positive for the influenza virus in clinical laboratories was 0.4%.
The CDC also confirmed that, based on NCHS mortality surveillance data available as of September 4, 2025, 0.06% of the deaths that occurred during the week ending Week 36 were attributed to influenza.
Unfortunately, a total of 280 influenza-associated pediatric deaths occurred during the 2024-2025 season.
This data is the highest number of pediatric deaths reported in any non-pandemic influenza season since the condition became reportable in 2004.
To reduce these pediatric deaths, the CDC and most state health departments recommend that eligible children receive the flu shot beginning in September each year.
Additionally, adults and children should be protected when traveling to a country reporting influenza outbreaks, such as Australia. Influenza vaccination is recommended for all Australians aged 6 months and older for the 2025-2026 flu season.
As of September 15, 2025, most pharmacies in the USA offer vaccine appointments to streamline the flu shot programs.
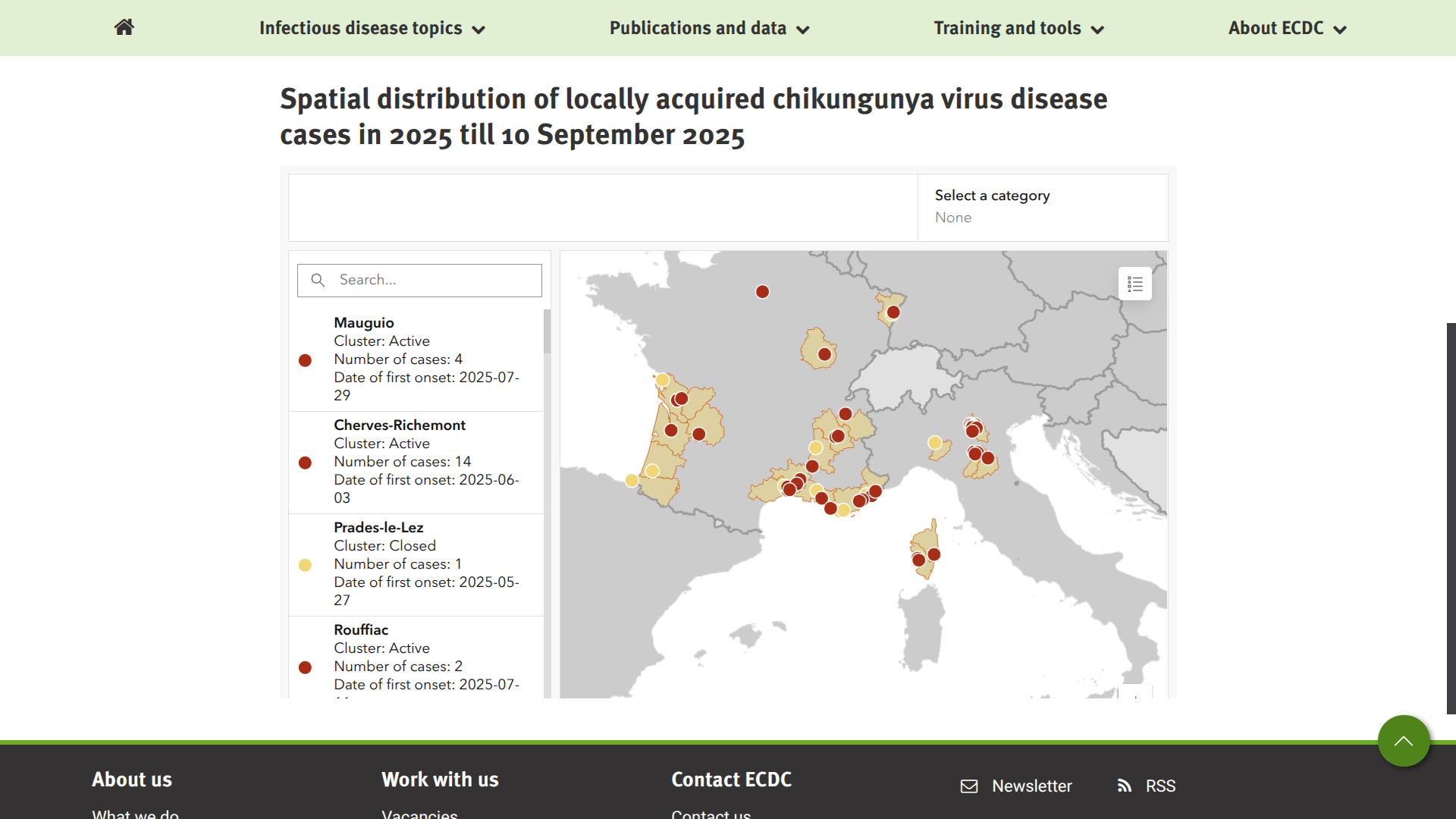
Since the beginning of 2025, two European countries have reported an unusual number of locally transmitted cases of chikungunya virus disease.
The European Centre for Disease Prevention and Control (ECDC) states that the environmental conditions in the areas of the Europe where Ae. albopictus or Ae. Aedes aegypti mosquitoes are established and currently favourable for chikungunya outbreaks.
As of mid-September 2025, France reported 82 new locally acquired cases of chikungunya, compared to 74 new cases the previous week, while Italy reported 60 new locally acquired cases (compared to 44 new cases the previous week.
In total, France's southern and western coasts have reported about 383 cases, and Italy's northern area has reported 167 local cases this year.
Both countries have also reported cases related to travel.
While the U.S. CDC recently highlighted chikungunya outbreaks in Bangladesh, Kenya, Madagascar, Somalia, and Sri Lanka, the Level 2 Travel Health Advisory did not list France or Italy.
Since the long-term health risks from a chikungunya infection remain unknown, the CDC recommends vaccination for travelers visiting an area with an outbreak.
When departing from the United States in September 2025, travel clinics and pharmacies offer U.S. FDA-approved vaccination services.
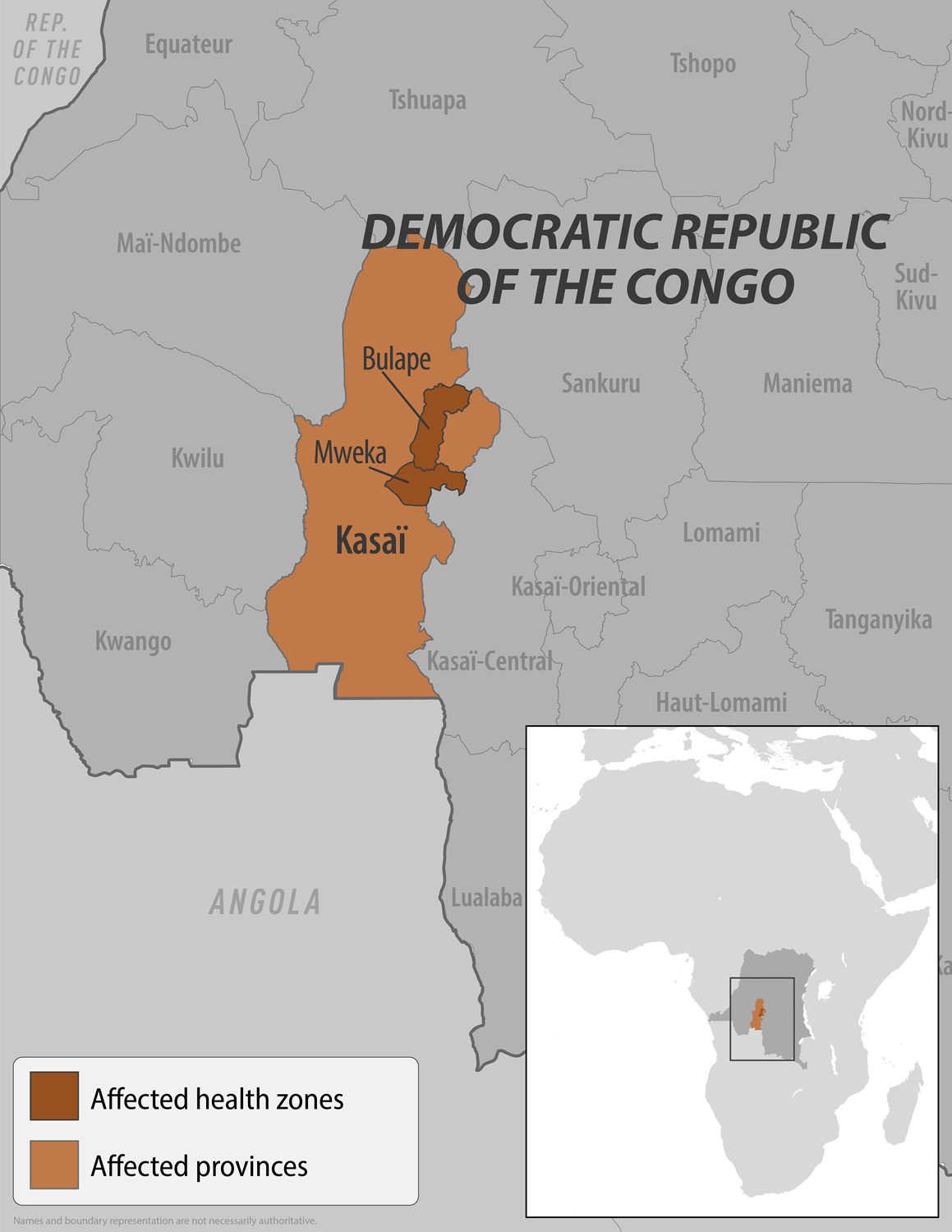
Vaccination of frontline health workers and contacts of people infected with Ebola virus disease has begun in Bulape health zone in the Democratic Republic of the Congo (DRC) 's Kasai Province, where an outbreak of the disease was declared.
The World Health Organization (WHO) stated on September 14, 2025, that an initial 400 doses of the Ervebo® Ebola vaccine, prepositioned in the capital, Kinshasa, have been delivered to Bulape, one of the current hotspots of the DRC's 16th Zaire Ebolavirus outbreak.
Additional Ervebo doses will be delivered to the affected localities in the coming days.
In addition, treatment courses of the Ebanga™ monoclonal antibody therapy (Mab114) drug have also been sent to treatment centres in Bulape for clinical care.
In the outbreak area, WHO has so far deployed 48 experts in disease surveillance, clinical care, infection prevention and control, logistics, and community engagement.
In countries neighboring the DRC, the WHO is working with national authorities to bolster operational readiness, enabling the rapid detection of Ebola cases and the prompt initiation of measures to curb further spread of the lethal virus.
As of September 15, 2025, the WHO assesses the overall public health risk posed by the ongoing outbreak as high at the national level, moderate at the regional level, and low at the global level.
To alert international travelers, the U.S. CDC issued a Level 1 - Practice Usual Precautions, Travel Health Advisory regarding this Ebola outbreak.
The CDC wrote on September 8, 2025: "While not commercially available, there is an FDA-approved vaccine for the prevention of the Zaire Ebola virus." It is presently available to select individuals in specific occupations (e.g., outbreak responders).
For more information on vaccines, please consult with your healthcare provider to discuss eligibility and access to the Ebola vaccine.
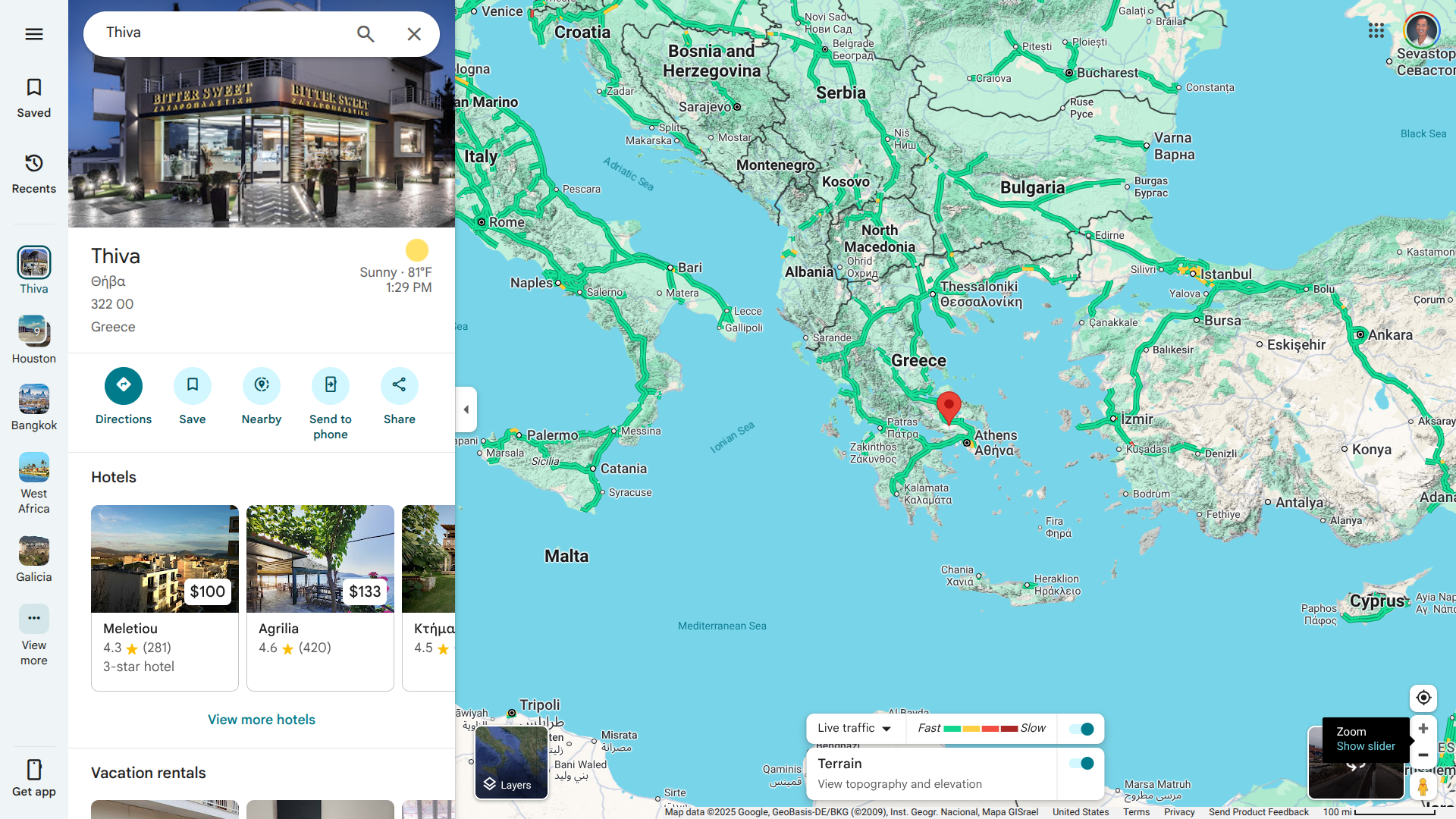
Malaria was eliminated from Greece in 1974. Since then, several (20-110) imported cases are reported annually to the National Public Health Organization (NPHO), referring to patients infected abroad in countries such as those in Africa and India.
As of early September 2025, there is evidence of probable local transmission/introduction (first-generation transmission) in two P. falciparum malaria cases who arrived in Greece in October 2024 from a malaria-endemic country.
According to the NPHP, the probable place of exposure is a rural village in the Municipality of Thiva, Regional Unit of Voiota.
As of September 14, 2025, no additional malaria cases were detected in the village.
Currently, the U.S. CDC and the UK do not recommend malaria vaccination before Greece.
While there are two WHO-approved malaria vaccines in use in 17 countries, neither are available in the USA. These malaria vaccines were added to the WHO's list of prequalified vaccines in 2024.
According to recent data published by the Japan Institute for Health Security (JIHS), Japan reported the most significant number of pertussis cases to date in 2025.
As of August 30, 2025, there have been a total of 72,448 pertussis cases reported in Japan this year.
Cases have been detected in all 47 Japanese prefectures, with Tokyo (5,846), Niigata (3,496), and Saitama (3,857) reporting the highest totals.
To help reduce these cases, the first round of pertussis routine immunization is administered three times for young children in Japan.
Furthermore, the JIHS recommends pre-arrival pertussis vaccination for individuals at risk, such as pregnant women and infants.
Unfortunately, the United States is confronting similar data.
Preliminary data show that more than six times as many cases were reported in 2024 compared to 2023.
However, the U.S. CDC reports that cases of pertussis have been trending downward since a peak in November 2024.
When planning a visit to Japan in 2025, the CDC advises travelers to be up to date with routine and travel vaccinations. This recommendation includes the Diphtheria-Tetanus-Pertussis vaccine.