Search API
With Lyme disease cases steadily declining in the United States, the only vaccine candidate conducting late-stage clinical research announced very encouraging news today.
On September 3, 2025, Valneva SE reported positive immunogenicity and safety data from the ongoing Phase 2 study of Lyme disease vaccine candidate, VLA15.
The strong anamnestic immune response and favorable safety profile following a third booster dose were consistent with those reported after receiving previous annual booster doses, further demonstrating compatibility with the anticipated benefits of a yearly vaccination before each Lyme season, wrote the company.
Juan Carlos Jaramillo, M.D., Chief Medical Officer of Valneva, commented in a press release, "These latest data further reinforce the potential benefits of booster doses across all evaluated age groups.... as the disease continues to expand geographically, it remains a pressing unmet medical need affecting communities across the Northern Hemisphere."
"Each set of positive results moves us closer to the possibility of making this vaccine available to both adults and children living in Lyme-endemic areas."
Lyme disease (Lyme borreliosis) is a bacterial disease transmitted to humans through the bite of infected ticks, initially detected in 1977 in Lyme, Connecticut, and now found in most northeastern states.
In the UK, ticks that carry Lyme disease are most active in the spring and summer. Approximately 4% of ticks in England and Wales are infected with Lyme disease.
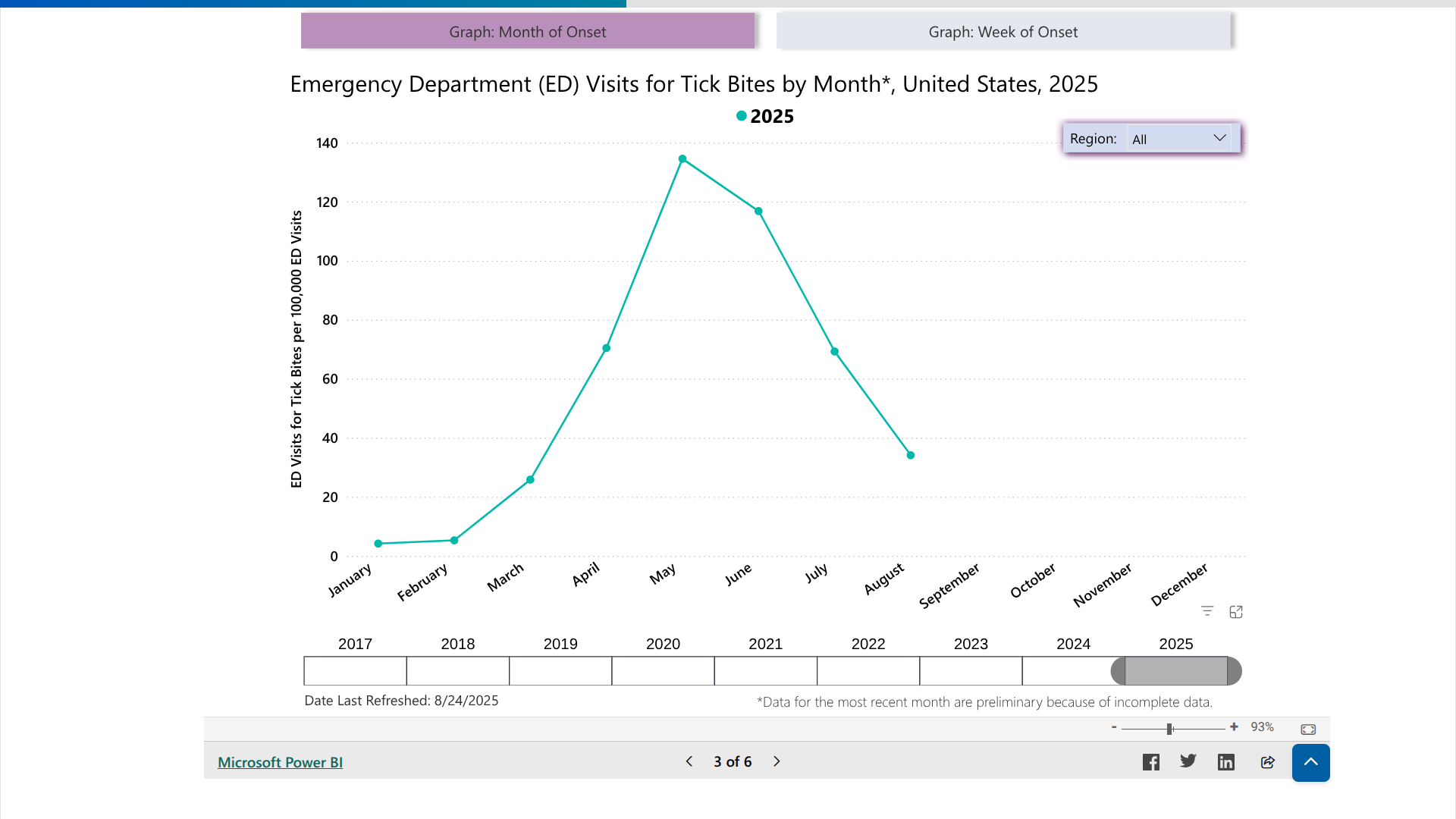
As of September 2025, the U.S. Centers for Disease Control and Prevention's Tick Bite Data Tracker displays case data and maps for the U.S.
The Communicable Diseases Agency of the Republic of Singapore has reported a total of 21 chikungunya cases this year.
As of August 28, 2025, this number has already surpassed the total recorded for all of 2024, which was 15 cases.
The increase began in May 2025, primarily due to travelers returning from areas affected by the chikungunya outbreak in China's Guangdong Province and several French Territories in the western Indian Ocean.
In 2024, this sovereign island country and city-state in Southeast Asia welcomed approximately 16.5 million international tourists, representing a 20% increase from the previous year.
In early August, Professor Ooi Eng Eong from Duke-NUS Medical School explained to the media that although chikungunya is less deadly than dengue, it can be debilitating. Chronic joint discomfort can limit physical activity and impact overall quality of life.
Although the U.S. CDC has not issued a Travel Health Advisory for chikungunya related to Singapore, the UK's Travel Health Pro indicates that there is a risk of chikungunya in this country.
As of September 3, 2025, the UK recommends that international travelers take precautions to avoid mosquito bites, especially during daytime hours.
Additionally, vaccination may be considered for individuals aged 12 years and older who meet specific eligibility criteria.
In the United States, the FDA has approved a chikungunya vaccine, which is available at travel clinics and pharmacies.

Since the Zika virus was first detected in the Region of the Americas in May 2015, the Pan American Health Organization (PAHO) has published counts of cases reported by member countries.
However, given the high proportion of asymptomatic individuals infected with the Zika virus, the lack of specificity in clinical presentation among cases, and the complexity of laboratory diagnosis in the context of co-circulation of closely related viruses such as chikungunya and dengue, underreporting of Zika virus cases is probable, wrote the PAHO.
While Brazil has been the multi-year leader in reporting Zika cases, the Argentine Republic has been confronted with a measurable outbreak in 2025.
As of September 2, 2025, the PAHO reported 730 Zika cases for the year. This data compares with 564 cases for all of 2024.
Currently, the U.S. CDC has not issued a Travel Health Advisory regarding Zika in Argentina.
However, the United Kingdom Travel Health Pro states there is a risk of the Zika infection in this country. Specific affected areas within Argentina where mosquitoes are spreading the virus are not available.
Both the CDC and the UK confirm that pregnant women should discuss the suitability of travel and the potential risks that the Zika virus may present with their healthcare provider before traveling abroad.
From a prevention and treatment perspective, no Zika vaccine or medication is expected to be available in 2025.

According to the WHO's Multi-country External Situation Report #57, published on August 28, 2025, all clades of the monkeypox virus (MPXV) continue to circulate in several countries.
The WHO writes that 'when mpox outbreaks are not rapidly contained and human-to-human transmission is not interrupted, they continue to pose a risk of sustained community transmission.'
In July 2025, 47 countries reported a total of 3,924 confirmed cases, including 30 deaths (case fatality ratio 0.8%).
China, Germany, Türkiye, and the United Kingdom have reported additional cases of mpox due to clade Ib MPXV since the last situation report.
These new cases have been linked to international travel.
On August 20, 2025, the WHO Director-General extended the standing recommendations for mpox until August 2026 to further prevent or reduce the international spread of mpox, as well as its impact on health.
Both the WHO and the U.S. Centers for Disease Control and Prevention (CDC) recommend receiving your first mpox vaccine at least 6 weeks before travel. After completing your first and second vaccine doses, which are given 4 weeks apart, it takes about two more weeks to get the best protection against mpox.
The majority of U.S. cases of clade II mpox continue to be reported in people who are not vaccinated or have received only one dose.
Several cases have recently been tied back to an outbreak in Sierra Leone, Liberia, and other West African countries.
The CDC suggests that whether or not you've been vaccinated (JYNNEOS®, MVA-BN®, IMVAMUNE®), you continue to reduce your risk of getting mpox.

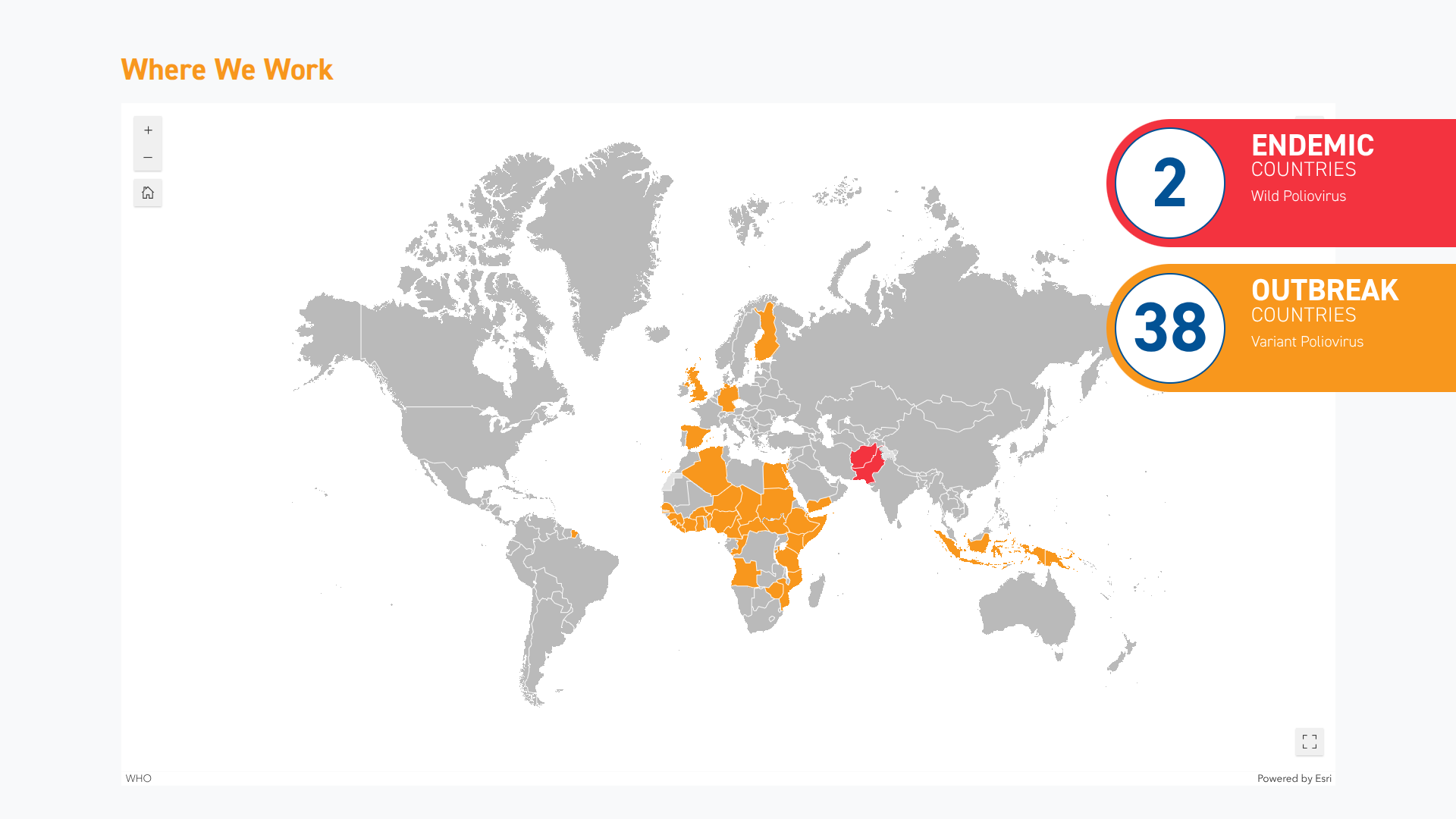
When the World Health Organization confirmed in June 2025 that the spread of the poliovirus remained a Public Health Emergency of International Concern, it identified several countries where visitors are at risk of contracting this severe disease.
As of August 27, 2025, new data from the Global Polio Eradication Initiative (GPEI) reveal an unexpected surge in polio cases in the Republic of Yemen, situated in southern Arabia.
According to the GPEI, 25 circulating vaccine-derived poliovirus type 2 (CVDPV2) cases were reported this week. This updated data brings the number of cases in Yemen for 2024 to 187 and 29 for 2025.
'The recent increase in reported cases and environmental sample isolates from 2024 and 2025 is not particularly linked to an increase in poliovirus transmission, but rather to retrospective testing,' wrote the GPEI.
CVDPV2 is a strain of poliovirus that can emerge in under-vaccinated populations when the oral polio vaccine (OPV) strains genetically revert to a form that can cause paralysis.
To address the shortcomings of this vaccine, the nOPV2 vaccine has been deployed over 1 billion times in various countries.
In the United States, the inactivated polio vaccine (IPV) was developed in 1955 and has been offered since 2000. IPVs produce antibodies in the blood that target all three types of poliovirus, thereby preventing the virus from spreading.
As of September 2, 2025, the U.S. CDC recommends IPV booster doses for specific travelers visiting areas where poliovirus has been detected, such as Israel and Germany.
IPVs are currently offered at travel clinics and pharmacies in the U.S.
The Dominican Republic Ministry of Health recently announced that the Caribbean island country had reduced dengue fever cases by over 85%.
As of Epidemiological Week 33, the total for 2025 is now 174 dengue cases, a significant improvement from last year's outbreak..
During 2024, 1,110 dengue cases were recorded in the same period.
The Health Ministry stated the decrease is attributed to the effectiveness of the national relaunch of the "Let's Beat Dengue" campaign, which carries the slogan "Eliminate, Clean, and Cover."
As part of the campaign, educational workshops, community operations to eliminate breeding sites, targeted fumigations, junk removal, distribution of informational materials, and larvicide distribution were implemented.
Dominican Republic's Minister of Health, Víctor Atallah, highlighted in a media release posted at the end of August 2025, that these prevention initiatives have positioned the country as a leader in disease control in the Region of the Americas, where dengue virus-transmitting mosquitoes have caused significant harm over the past few years.
“We have demonstrated that prevention works. The country today shows encouraging figures that reflect the dedication of our personnel and the commitment to protecting the health of the Dominican people."
"Now we will redouble our efforts to sustain and expand this success, and continue winning the battle against dengue," stated Atallah.
In addition to dengue, this vacationer's favorite destination continues to battle two other mosquito-borne diseases, chikungunya and malaria.
As of September 2, 2025, the U.S. CDC recommends chikungunya vaccination for at-risk travelers visiting areas with outbreaks; however, vaccines for dengue and malaria are not available in the USA.

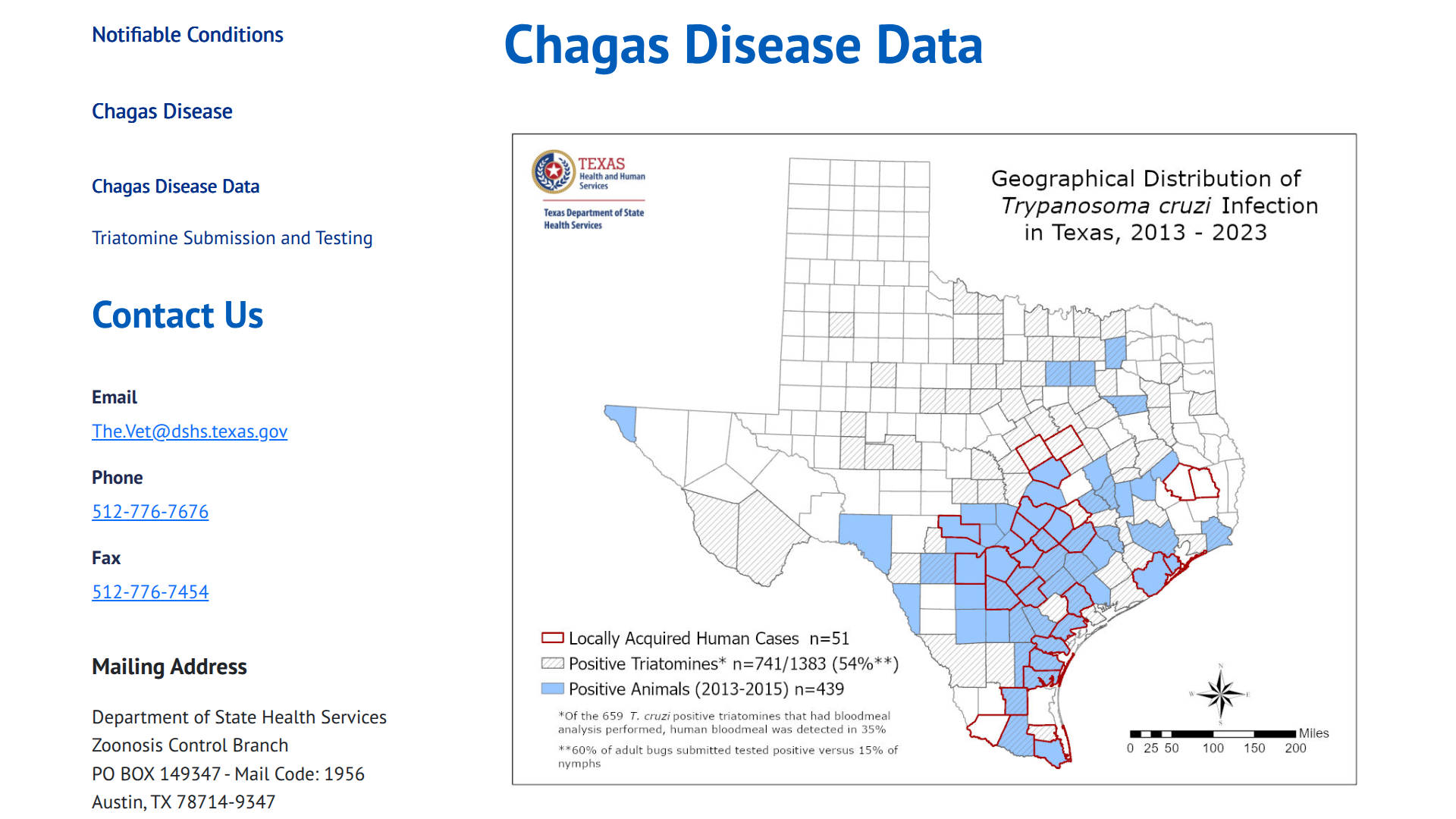
Chagas disease, also known as American trypanosomiasis, is found in twenty-one countries in the Americas, including the United States, where it has become endemic.
In the U.S., blood-sucking insects occur naturally in the southern half of the country and, as of September 2025, have been identified in 32 states.
The state of Texas has undertaken extensive efforts to document human Chagas disease cases that were made reportable in 2013. The first known autochthonous case of human Chagas disease in the U.S. occurred in an infant in Corpus Christi, Texas, in 1955, in a home infested with triatomines.
According to the U.S. CDC's Emerging Infectious Diseases (Volume 31, Number 9—September 2025), in this Perspective, researchers review a body of evidence establishing the robust presence of T. cruzi parasites in the U.S., not only among insect vectors, wildlife, and domestic animals but also among humans without travel histories who are assumed to be locally infected.
After feeding, these bugs pass the parasite in their feces. If the feces enter a person's body through a cut or near the eyes or mouth, it can cause infection.
These researchers wrote, 'Updating Chagas disease endemicity status as hypoendemic is a crucial step toward a more effective management model, one that addresses the unique challenges and complexities of this country regarding vector-borne diseases.'
'Such a shift will help reform curriculum in professional schools to enable the next generation of practitioners to be competent in recognizing the low but present risk for locally acquired T. cruzi infections and better serve those who acquire the parasite elsewhere and require diagnosis in the U.S.'
A Viewpoint published by The Lancet in May 2025 wrote that, despite many studies, there is still no vaccine for Chagas Disease.
To make matters worse for those infected, the only two drugs available have proved efficacy only when administered during the acute phase of the disease.
The U.S. government has recently issued travel alerts regarding visits to the Plurinational State of Bolivia in 2025.
As of August 31, 2025, the U.S. CDC included Bolivia in two recent Travel Health Advisories: one for measles outbreaks and another for yellow fever.
Additionally, Bolivia is reporting an unusual number of mosquito-transmitted chikungunya fever cases in 2025.
The Pan American Health Organization's latest data indicate that Bolivia trails just Brazil in the number of chikungunya cases (5,159) and deaths (4) in the Americas in 2025.
Oropouche virus and Zika diseases are also emerging risks in Bolivia.
If you plan to visit Bolivia, the CDC has confirmed that U.S. FDA-approved travel vaccines are available for these diseases at various retailers in the USA.
From a safety perspective, the U.S. Department fo State's travel advisory for Bolivia says visitors should exercise increased caution in Bolivia due to civil unrest. Some areas have an increased risk.
For example, the State Department advises against visiting the Chapare region due to crime.
If you do visit this area, the local embassy recommends enrolling in the Smart Traveler Enrollment Program to receive digital alerts and make it easier to locate you in an emergency.