Search API
According to disappointing news released today, the world must wait for an approved vaccine that prevents invasive E. coli disease (IED).
Sanofi announced today that a scheduled review of the E.mbrace phase 3 clinical study conducted by an independent data monitoring committee (IDMC) determined that Sanofi and Johnson & Johnson's vaccine candidate for extraintestinal pathogenic E. coli was not sufficiently effective at preventing IED compared to placebo.
As a result of the IDMC's determination, the E.mbrace study is being discontinued.
The study, initiated in June 2021, enrolled older adults with a history of urinary tract infections (UTIs) in the past two years. It was conducted at over 250 sites across five continents. Janssen Research & Development, LLC, is the trial sponsor and responsible party and will continue appropriate safety follow-up for the currently enrolled participants.
Jean-François Toussaint, Sanofi's Global Head of Research and Development Vaccines, commented in a press release on February 13, 2025, "E. coli sepsis is a devastating disease, and no preventative measures are available to date."
In October 2023, Sanofi agreed with Janssen Pharmaceuticals, Inc. (Janssen), a Johnson & Johnson company, to develop and commercialize the vaccine candidate. As a result of the discontinuation, Sanofi has recorded an impairment charge before tax of $250 million in the Q4 2024 results.
UTIs are among the most common bacterial infections, many of which are caused by uropathogenic E. coli. Still, less common pathogens, such as Enterococcus faecalis and other enterococci, can cause infections by infecting an abnormal or catheterized urinary tract.
UTIs are more common in females because their urethras are shorter, making it easier for bacteria to enter the urinary tract. Moreover, younger people also suffer from UTIs.
As of 2025, the U.S. Centers for Disease Control and Prevention says most UTIs can be treated with antibiotics prescribed by a healthcare professional.
However, international travelers seeking access to a non-FDA-approved UTI vaccine (Uromune™, MV140) outside of the USA can submit an appointment request using this Vax-Before-Travel link.

Despite decades of clinical research, Herpes Simplex Virus (HSV) remains among the most prevalent infectious pathogens, impacting millions annually. While herpes vaccine candidates continue to progress in clinical trials, none have been approved.
However, an innovative HSV therapy may soon become available.
Theralase® Technologies Inc. announced today that the previous University of Manitoba research has been validated, proving that Ruvidar® is safe and effective in the inactivation of Herpes Simplex Virus, Type 1 (HSV-1), in an animal model.
In the latest Theralase® research, announced on February 10, 2025, Balb/C mice were infected with the human HSV-1 virus. On day 6 post-infection, 20 uL of a 1% Ruvidar® solution was applied topically over the area of well-developed lesions once daily for four days.
Four days of Ruvidar treatment resulted in complete healing of the HSV-1 cutaneous lesions.
In a press release, the Company stated that these 'results support the safety and efficacy of topically applied non-light activated Ruvidar® against cutaneous HSV-1 lesions in a mouse model.'
Kevin Coombs, B.A., M.A., Ph.D., professor of medical microbiology and infectious diseases at the Max Rady College of Medicine, University of Manitoba (retired), stated, "I am delighted that Theralase® researchers were able to successfully translate my team's cellular inactivation of HSV into a safe and effective therapy in an animal model."
"Their research may prove to be instrumental in developing a clinical program that will have real-world impacts on the lives of billions of people infected with this prolific disease."
Effective U.S. FDA-approved anti-herpetic drugs available in 2025 include acyclovir and later-generation derivatives (penciclovir, valacyclovir, famciclovir, and ganciclovir), which inhibit viral DNA synthesis.
Independent research by the University of Manitoba verifies that Ruvidar is more effective than acyclovir in inactivating HSV after infection.
According to the Company's press release, Ruvidar inhibited HSV-1 replication at significantly lower concentrations.
The effects of Ruvidar versus acyclovir on HSV-1 yields when added 24 hours post-infection (hpi). Vero cells were infected with HSV-1 at a Multiplicity of infection ~ 1.5, incubated for 24 hours, and then treated at 24 hpi with indicated drug concentrations for an additional 44 hours.
Virus yields were then determined, and reductions in virus yields were compared to non-treated controls.
Roger DuMoulin-White, B.Sc., P.Eng, Pro.Dir., President and Chief Executive Officer, Theralase, stated, "Based on the success of Theralase®'s latest research, Theralase® plans to develop a vaccine and therapeutic for the prevention and treatment of HSV, with clinical development to commence thereafter."
This announcement was based on an animal model study, indicating the product is not commercially available.

Since the clade II mpox outbreak began about three years ago, the U.S. Centers for Disease Control and Prevention (CDC) has issued Travel Health Advisories based on the type of virus.
Historically, clade I have been associated with a higher percentage of people with mpox developing severe illness or dying, compared to clade II.
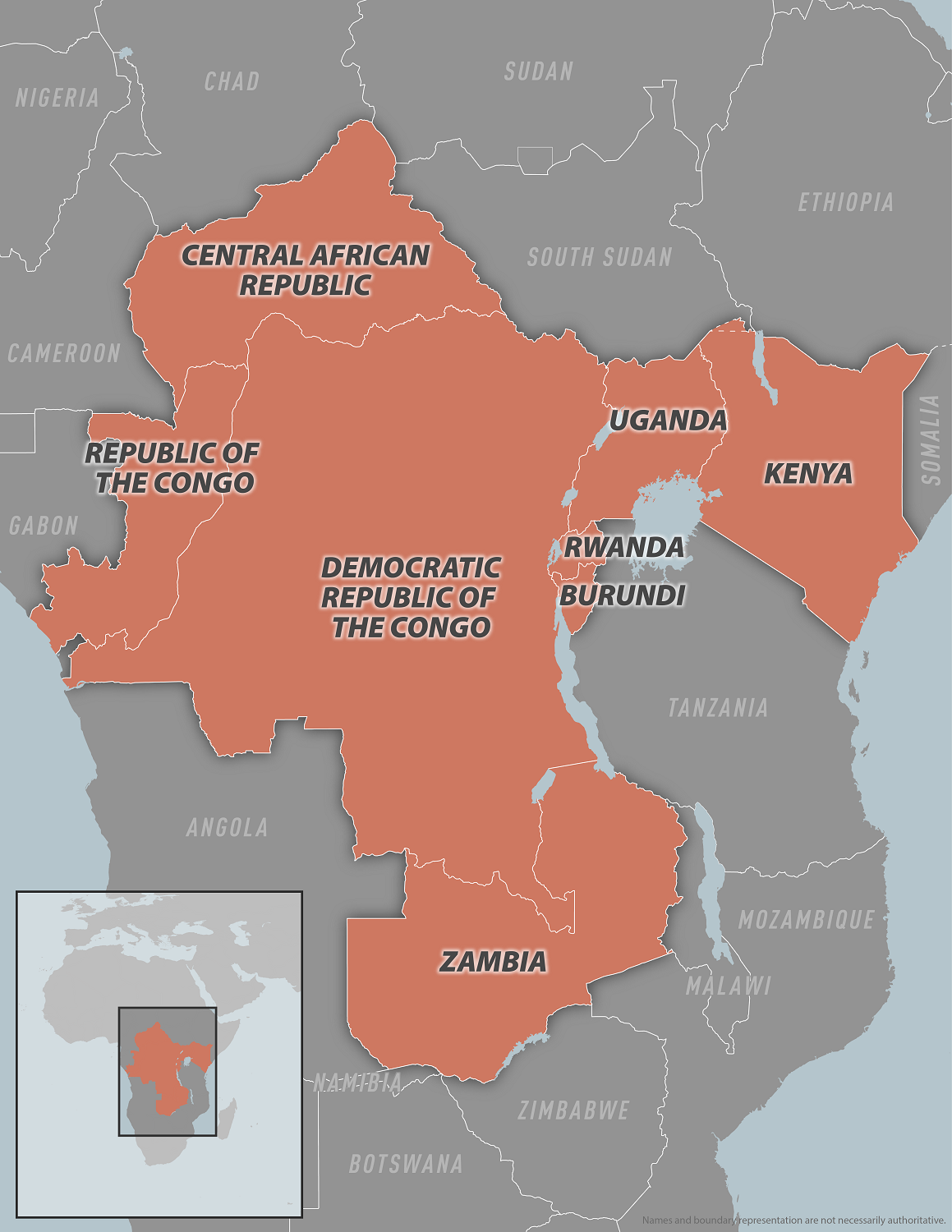
On February 10, 2025, the CDC reissued a Level 2 Practice Enhanced Precautions advisory regarding the clade I mpox outbreaks in eight Central and Eastern African countries.
The CDC wrote, 'There is an ongoing person-to-person transmission of mpox in Burundi, Central African Republic, Democratic Republic of the Congo, Kenya, the Republic of the Congo, Rwanda, Uganda, and Zambia.'
In the United States, the New Hampshire Department of Health and Human Services reported the third clade 1b case in the past four months. This mpox patient recently traveled to Eastern Africa.
During these mpox outbreaks, person-to-person transmission has occurred through various means, including sexual contact, day-to-day household contact, and within the healthcare setting. Transmission has also occurred from contact with certain live or dead wild animals.
Mpox is a disease caused by infection with the Monkeypox virus. Symptoms often include fever, rash, headache, muscle aches, and swollen lymph nodes, although fever is not always present.
The CDC says If you are sick and could have mpox, follow isolation and infection control measures at home and during travel.
Mpox vaccination is recommended by the CDC for certain people visiting at-risk areas.
In the U.S. and many countries, mpox vaccines (JYNNEOS®, MVA-BN®) are commercially available in 2025.
France is one of the most popular tourist destinations, reaching about 100 million guests annually. Its overseas department, La Réunion, welcomes about 500,000 vacationers to its beautiful mountains and beaches.
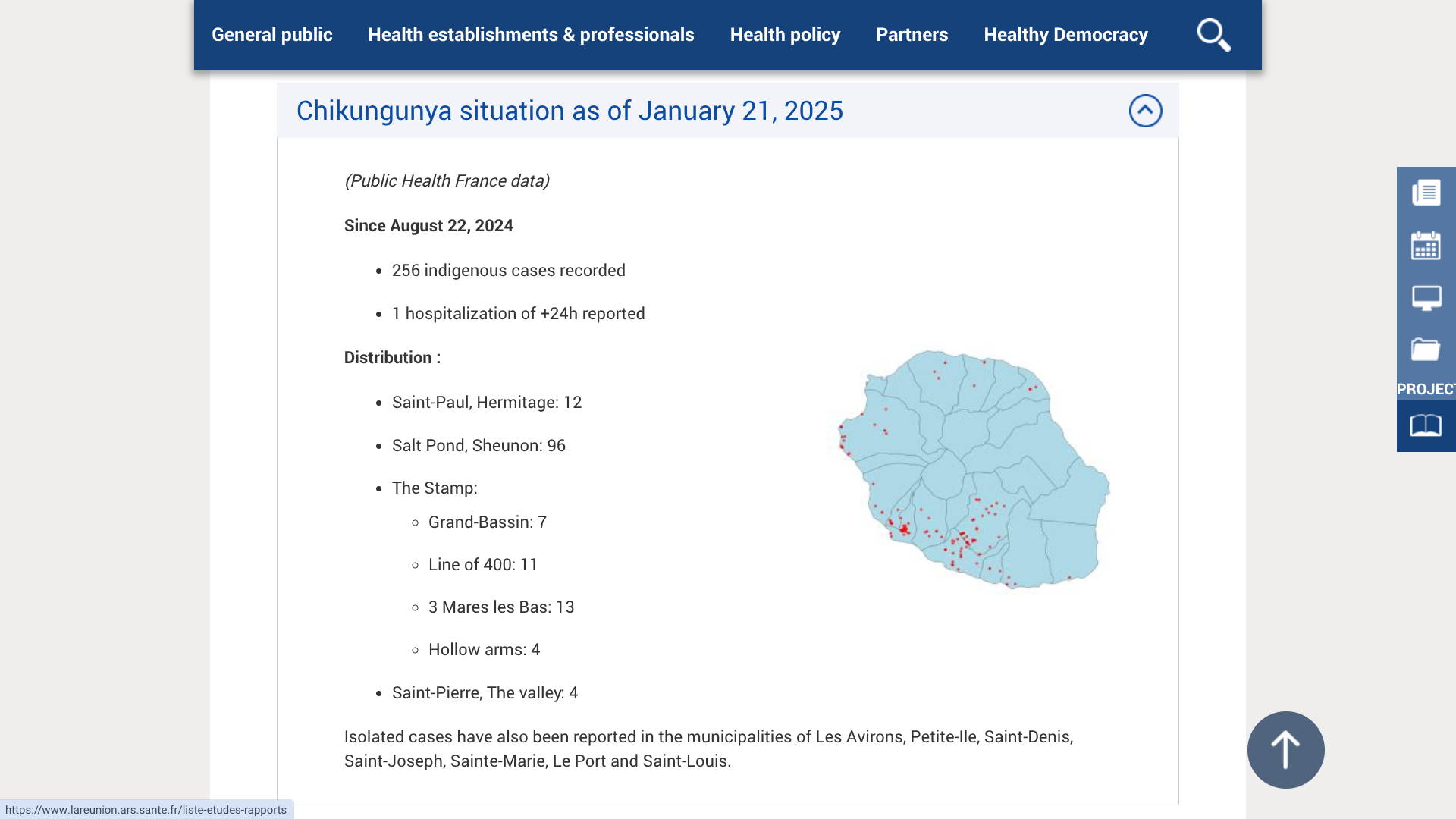
However, due to the increase in the number of Chikungunya virus cases and its continued infections, and on the proposal of the Director General of the ARS Gérard COTELLON, Patrice LATRON, France's Prefect of La Réunion, has triggered level 3 of the ORSEC "arboviruses" system, which corresponds to a low-intensity epidemic.
As of February 11, 2025, and since August 23, 2024, ARS Reunion has confirmed 783 indigenous cases, including 671 since the start of 2025.
The municipalities of Étang-Salé and Le Tampon still have the highest number of Chikungunya cases.
'As soon as a case of Chikungunya is reported, the ARS intervenes in the affected area, without waiting for confirmation of the case by the medical biology laboratory, to reduce the risk of spreading the virus.'
The last major Chikungunya outbreak in La Réunion was from 2005 to 2006.
The ongoing outbreak in La Réunion is caused by Ae. albopictus, the primary vector, due to the adaptation of the ECSA CHIKV genotype.
While the U.S. CDC has yet to highlight La Reunion's Chikungunya outbreak as a travel risk, it says international travelers should arrange an appointment with a travel vaccine specialist at least four to six weeks before departing for France. An appointment with a travel expert provides an opportunity to assess which vaccines are appropriate for your trip abroad in 2025.
When departing for France or La Reunion from the United States, Valneva SE's IXCHIQ® chikungunya vaccine is commercially offered by various travel clinics and pharmacies. And in 2025, this innovative vaccine can be found throughout Europe.
The World Health Organization (WHO) recently confirmed the yellow fever (YF) virus has become endemic in tropical areas of the Region of the Americas, such as the Republic of Colombia.
While yellow fever is a vaccine-preventable disease, with ample supplies available in Colombia, significant outbreaks have been reported over the past 13 months.
The WHO reported on February 4, 2025, that between the start of 2024 and EW 4 of 2025, a total of 31 confirmed cases of YF have been reported, including 15 fatal cases.
Recent YF outbreaks have been detected in the department of Tolima in the municipalities of Cunday, Prado, and Purificación.
With over 6 million tourists visiting Colombia last year, most landing at the El Dorado International Airport, the WHO and U.S. CDC have offered updated vaccine recommendations.
Travelers ≥1 year old arriving from Angola, Brazil, the Democratic Republic of the Congo, or Uganda; this includes certain airport transits or layovers in any of these countries, must be vaccinated.
YF vaccination is generally not recommended for travel limited to Barranquilla, Cali, Cartagena, or Medellín cities, areas in Colombia above 7,550 ft. in elevation (where infected mosquitoes are not found), the archipelago departments of San Andrés and Providencia, or the city of Bogotá.
When departing from the United States in 2025, the YF-VAX® vaccine is commercially offered at travel clinics and pharmacies.
From a safety perspective, the U.S. Department of State issued a high-level travel advisory for Colombia in January 2025, stating that visitors should exercise increased caution due to civil unrest and that some areas are at increased risk.