Search API
The Centers for Disease Control and Prevention (CDC) has detected an increase in extensively drug-resistant Shigella infections in the United States over the past few years.
As of January 11, 2025, the U.S. CDC confirmed 296 Shigellosis cases have already been reported in 2025, led by New York (53) and Florida (42).
Last year, the CDC confirmed 20,621 Shigella cases nationwide, led by California (4,365) and New York (2,990).
In Northern Nevada, the Public Health (NNPH) agency identified a Shigellosis outbreak in Reno / Washoe County after a reported influx of new cases and hospitalizations. About 14 cases and nine hospitalizations were reported, although the number of cases is expected to be much higher.
However, there is a low risk of transmission to the general public in 2025.
Shigellosis is an intestinal infection that causes diarrhea, fever, and stomach pain. Shigellosis can be spread by coming into contact with the poop of an infected person, eating or drinking contaminated food or water, or through sexual contact.
According to the CDC, Shigellosis can be challenging to treat, and prevention is critical to reducing the spread of the infection.
As of January 18, 2025, the U.S. FDA has not approved a preventive vaccine. However, a tetravalent bioconjugate vaccine candidate has progressed into phase 2 clinical research.

Despite spending $4 billion annually, the number of malaria cases and deaths has not significantly changed over the past decade, especially in Africa. Last year, the WHO's African Region reported the broadest malaria outbreak burden.
Based on today's U.S. Centers for Disease Control and Prevention (CDC) Travel Health Advisory, health agencies are not optimistic about seeing any improvement in this trend by 2025.
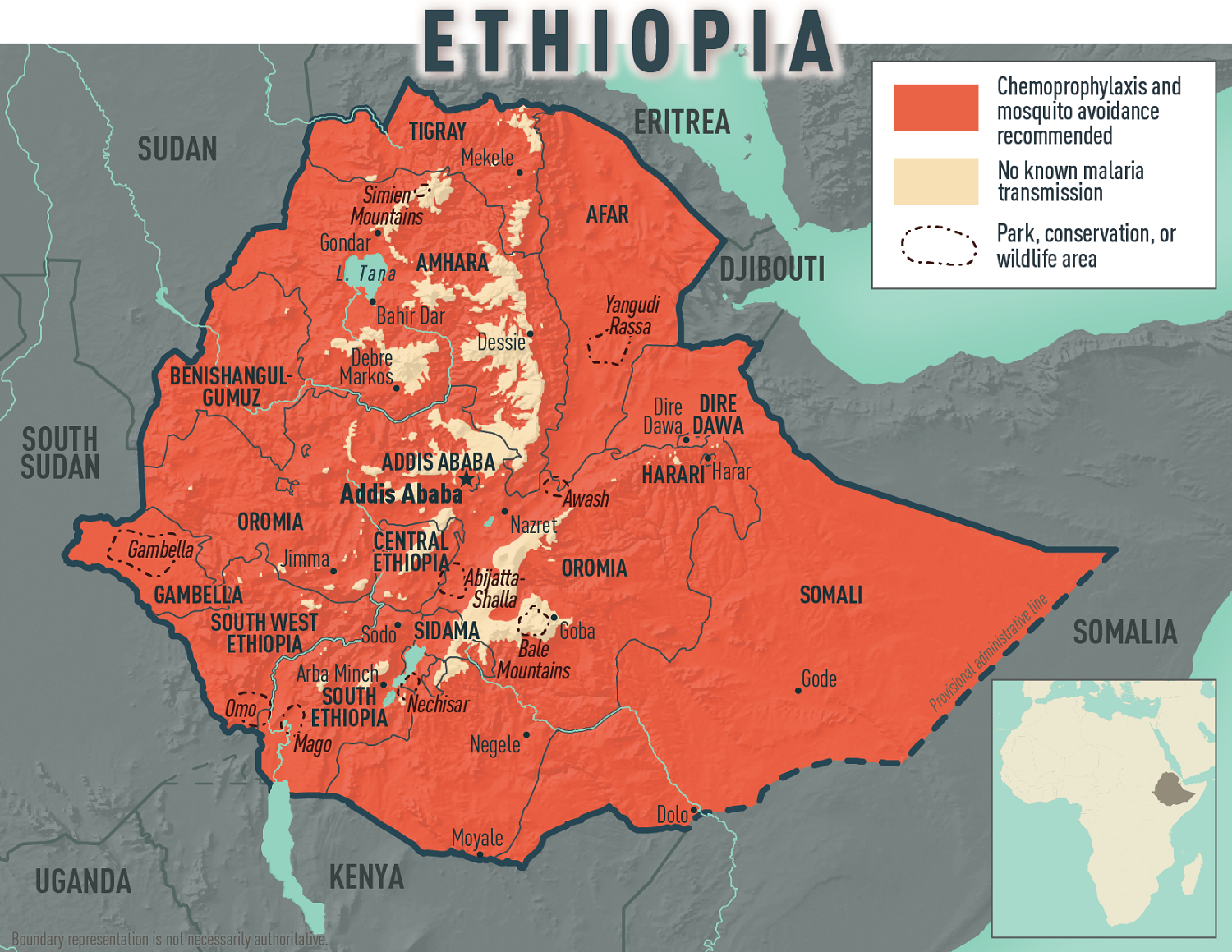
Today, the CDC confirmed an ongoing malaria outbreak in the Federal Democratic Republic of Ethiopia, affecting all 14 country regions. More than 8.4 million malaria cases were reported, the highest number of cases ever reported within a year.
To bolster Ethiopia’s fight against malaria, the United States Government, through the U.S. Agency for International Development, donated 175 computer terminals to the Ethiopian Public Health Institute on January 15, 2025.
Additional U.S. support includes over $27.5 million of antiretroviral supplies, early infant diagnostics, quality assessment panels, lab equipment, and more.
Malaria is a disease caused by a parasite that spreads to humans through the bite of infected mosquitoes, commonly found in Africa.
If you plan to travel to Ethiopia in 2025, the CDC recommends speaking with a travel health expert about which antimalarial drug is best for you. And seek medical care immediately if you develop fever, chills, sweats, headache, vomiting, or body aches during or after travel to Ethiopia.
In 2024, numerous international travelers brought malaria back with them.
As of the week ending November 23, 2024, the CDC confirmed 1,772 malaria cases, mostly among international travelers arriving in New York City (232), Texas, Miami, Florida, and Los Angeles, California.
While malaria vaccines are available in Africa, they are not FDA-approved in the U.S. and remain unavailable in the U.S.
Furthermore, innovative vaccine candidates, such as the RH5.1/Matrix-M malaria vaccine, are proceeding in late-stage clinical trials. Developed at the University of Oxford, this vaccine targets blood-stage malaria, unlike previously approved vaccines that target the pre-erythrocyte stage.
While Chikungunya and Dengue virus outbreaks reached records in the Region of the Americas in 2024, a little-known virus with similar symptoms has been spreading, causing complications in diagnosis.
Oropouche virus, primarily transmitted through bites from infected midges, has expanded its range over the past year, reaching Central America and the Caribbean.
Research published in The Lancet Infectious Diseases in December 2024 estimates that up to 5 million people in the Americas are at risk of exposure to the virus.
To confuse a diagnosis, Oropouche infections can appear clinically similar to Chikungunya, Dengue, Malaria, and Zika. A reverse transcriptase–polymerase chain reaction test is only administered after a negative dengue result.
Still, once confirmed, no treatment or preventive vaccine for Oropouche is available as of January 2025.
To alert international travelers to this health risk, the U.S. CDC updated its Level 1 - Practice Usual Precautions, Travel Advisory on December 18, 2024. The CDC lists nine countries that have reported Oropouche cases.
And in Brazil, the CDC issued a Level 2 Advisory for Espírito Santo.
In Florida, about 103 international travelers have been diagnosed with this infection.
Symptoms of Oropouche infection include headache, fever, muscle aches, stiff joints, nausea, vomiting, chills, or sensitivity to light. Severe cases may result in neuroinvasive diseases such as meningitis.
Furthermore, the CDC says the Oropouche virus has been found in semen and may spread through sex.

Throughout the record-setting dengue virus outbreak in the Region of the Americas, the Republic of Nicaragua reported 92,022 cases in 2024.
According to a study published on January 10, 2025, all four virus serotypes impacted Nicaragua's dengue outbreak. Based on 19 years of data from the Pediatric Dengue Cohort and Pediatric Dengue Hospital-based Studies in Managua, the relationship between serotype and immune status and dengue severity became very clear.
Of the 2,644 cases with serotype results by RT-PCR, 559 corresponded to DENV1, 1,002 to DENV2, 760 to DENV3, and 323 to DENV4.
Severe disease was more prevalent among secondary DENV2 and DENV4 cases, while similar disease severity was observed in both primary and secondary DENV1 and DENV3 cases.
These researchers wrote, 'These findings demonstrate differences in dengue severity by serotype and immune status and emphasize the critical need for a dengue vaccine with balanced effectiveness against all four serotypes, as existing vaccines show variable efficacy by serotype and serostatus.'
Nicaragua's southern neighbor, the Republic of Colombia, reported similar dengue virus types in 2024.
In the United States, dengue virus serotype 3 was most often identified among travel-associated and locally acquired dengue cases in Florida in 2022-2023.
As of January 11, 2025, the leading dengue vaccine available in the Americas does not meet this requirement. However, vaccine candidates currently conducting research may need this clinical need.
There are no dengue vaccines currently offered in the United States.
Overall, more than 12 million dengue cases were reported in the Americas last year, about 300% more than in 2023.
In the U.S., 53 jurisdictions reported 9,255 dengue cases as of December 31, 2024. The unfortunate leaders in local dengue transmission were Arizona, California, Florida, New Jersey, New York, and Puerto Rico.

In the Region of the Americas, 2024 has been marked as the worst year ever for dengue virus infections, 12.8 million, and related fatalities, 7,855.
From a country perspective, the United States has experienced a significant impact, with dengue cases increasing by approximately 43%. According to the U.S. CDC, 8,863 dengue cases were reported as of mid-December 2024, compared to 6,164 cases in 2023.
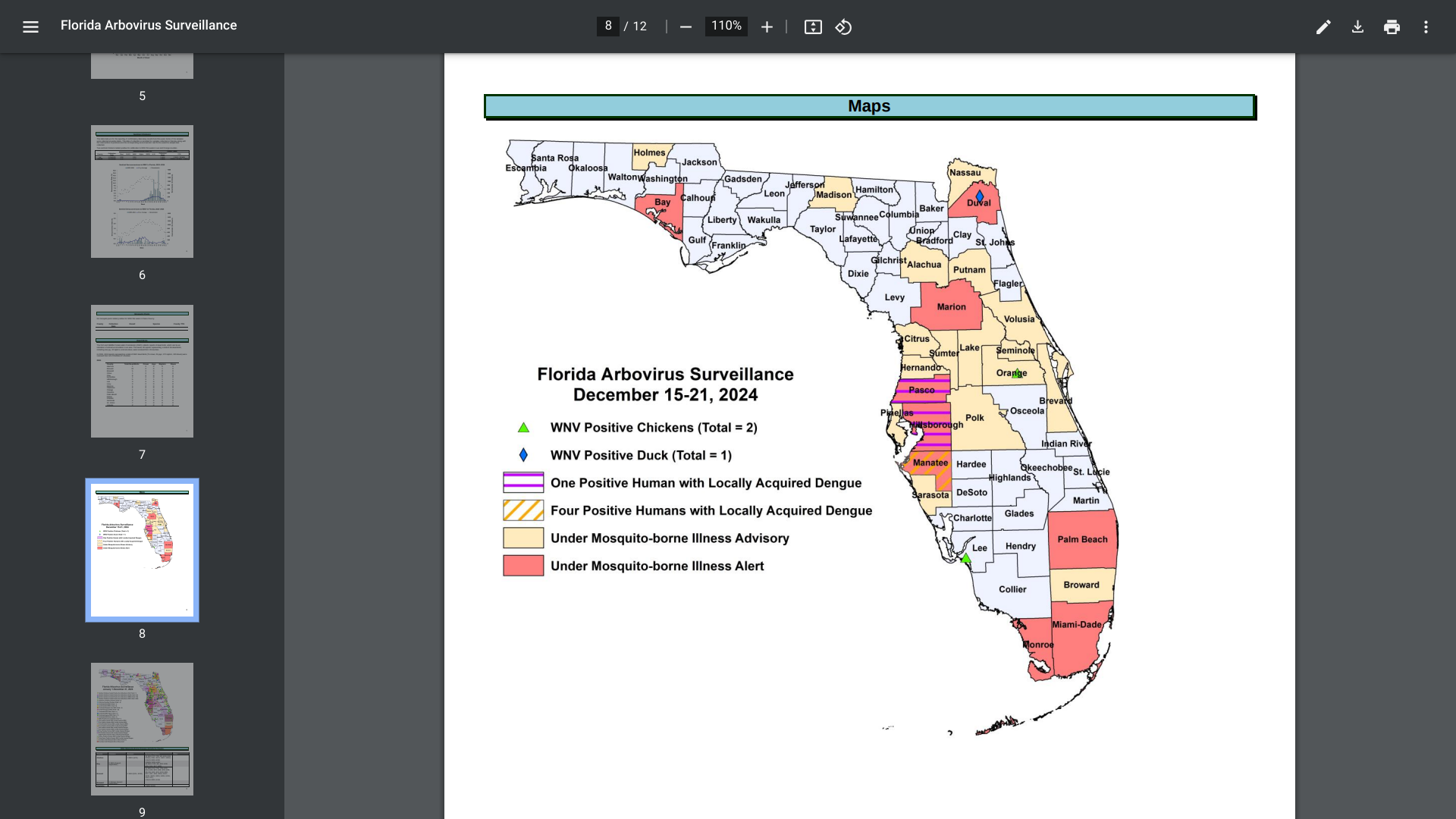
Within the U.S., the Florida Department of Health recently reported some unsettling news.
As of late December 2024, 911 travel-associated dengue cases had been reported, mainly by visitors to Brazil (61), Cuba (506), and Puerto Rico (41). Additionally, 85 locally acquired dengue cases were reported from ten counties, led by Miami-Dade (47).
In 2023, 609 travel-associated dengue cases were reported, and 186 humans contracted dengue while in Florida.
With international travel expected to increase in 2025, this CDC data suggests that more international visitors may unintentionally introduce one of the four dengue viruses in Florida next year.
Furthermore, since mosquitoes transmit dengue, locally acquired infections will likely increase next year.
From a disease prevention perspective, there is hope that access to dengue vaccines may improve in 2025 as approved vaccines increase production and vaccine candidates seek approvals.
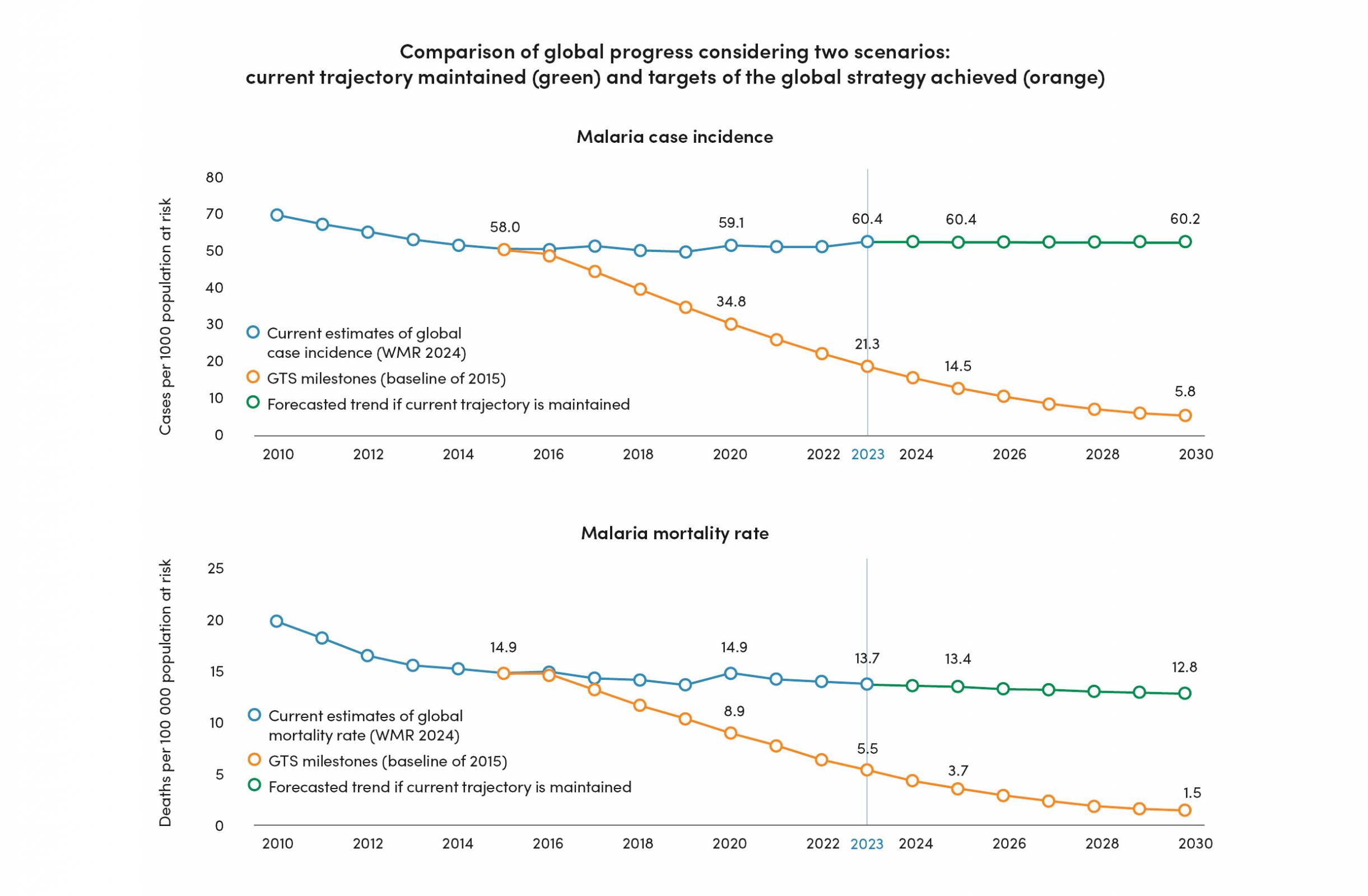
As 2024 draws to a close, the World Health Organization (WHO) published an in-depth update on malaria burden and trends at global, regional, and country levels. As of December 19, 2024, the WHO reported malaria outbreaks remain a formidable public health challenge.
In 2023 alone, there were an estimated 597,000 malaria-related fatalities and 263 million new cases, an increase of 11 million cases over 2022.
The WHO wrote, 'Given current trends, progress towards critical targets of the WHO global malaria strategy is off track.'
As the WHO Director-General stated: "No one should die of malaria.... An expanded package of lifesaving tools now offers better protection against the disease, but stepped-up investments and action in high-burden African countries are needed to curb the threat."
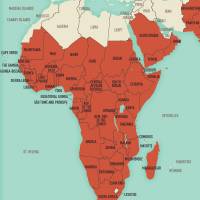
The WHO African Region continues to be most impacted, accounting for an estimated 94% of global cases, led by Nigeria and the Democratic Republic of the Congo.
When visiting these countries, the WHO recommends international travelers speak with a travel vaccine expert one month before departure. In November 2024, the WHO published a revised version of the consolidated Guidelines for malaria with an updated vaccine recommendation.
While malaria vaccines are available in Africa, they are unavailable in the USA in 2024.
In the U.S., most malaria cases are travel-related.
The U.S. Centers for Disease Control and Prevention reported that as of the week ending November 23, 2024 (#47), 1,772 malaria cases had been confirmed in 2024, mostly among international travelers arriving in New York City (232), Texas, Miami, Florida, and Los Angeles, California. In 2023, there were 2,013 travel-related malaria cases in the U.S.