Search API
The Department of Mayotte, an overseas department of France, recently announced that, due to the first indigenous (local) case of chikungunya on the island, health authorities are activating level 2A of the ORSEC (emergency) plan.
This decision will increase surveillance of the epidemiological situation and measures to prevent more active viral (virus) circulation by mosquitoes in the territory.
As of April 7, 2025, Mayotte has reported four chikungunya cases this year.
As a reminder, about 900 miles away, Reunion Island has been facing a chikungunya epidemic, with 13,594 cases, including two related fatalities, since August 2024.
Mayotte's Regional Health Agency says all travelers to and from Reunion Island should protect themselves from mosquito bites.
Mayotte is located between Africa's east coast and Madagascar, one of France's 18 regions.
To protect people on Reunion, the local government has started vaccinating 40,000 residents with a U.S. FDA-approved vaccine.
Valneva SE's IXCHIQ® Chikungunya vaccine is commercially available in the U.S. and recommended for travelers to endemic areas in 2025.

Two powerful earthquakes recently struck the central part of the Republic of the Union of Myanmar's Sagaing Region near Mandalay. The full scale of damage, deaths, and injuries has not yet been ascertained.
The World Health Organization's (WHO) Public Health Situation Analysis, released on April 3, 2025, says preliminary assessments indicate high casualties and trauma-related injuries, with an urgent need for emergency care.
On April 2, 2025, the State Administration Council (SAC) reported that 3,003 people had died and 4,515 had been injured in the earthquake.
In the earthquake-affected areas, with limited access to safe water and worsening sanitation and hygiene conditions, the WHO says the risks for Acute Waterborne (AWD) - cholera outbreaks are assessed as very high.
Since July 2024, AWD and cholera cases have surged in at least nine states, including Ayeyarwady, Bago, and Mandalay.
Mandalay, which faced a cholera outbreak in October 2024, remains at high risk for further outbreaks due to infrastructure damage and overcrowded shelters, significantly increasing the likelihood of cholera and other waterborne disease outbreaks.
From June 22, 2024, to March 23, 2025, 12,195 AWD cases (not all confirmed as cholera) were reported, along with three deaths.
A vaccination campaign using oral cholera vaccine (OCV) has been conducted in Yangon, Mon, and Mandalay, providing 2.4 million doses.
As of April 7, 2025, the U.S. CDC says, 'OCV vaccination may be considered for children and adults traveling to areas of active cholera transmission.'
In the United States, OCVs such as DUKORAL® are available at travel clinics and pharmacies.
The WHO wrote, 'These deteriorating conditions, combined with overcrowded temporary shelters and reduced sanitation services, significantly increase the risk of cholera and other waterborne disease outbreaks in the affected areas.'

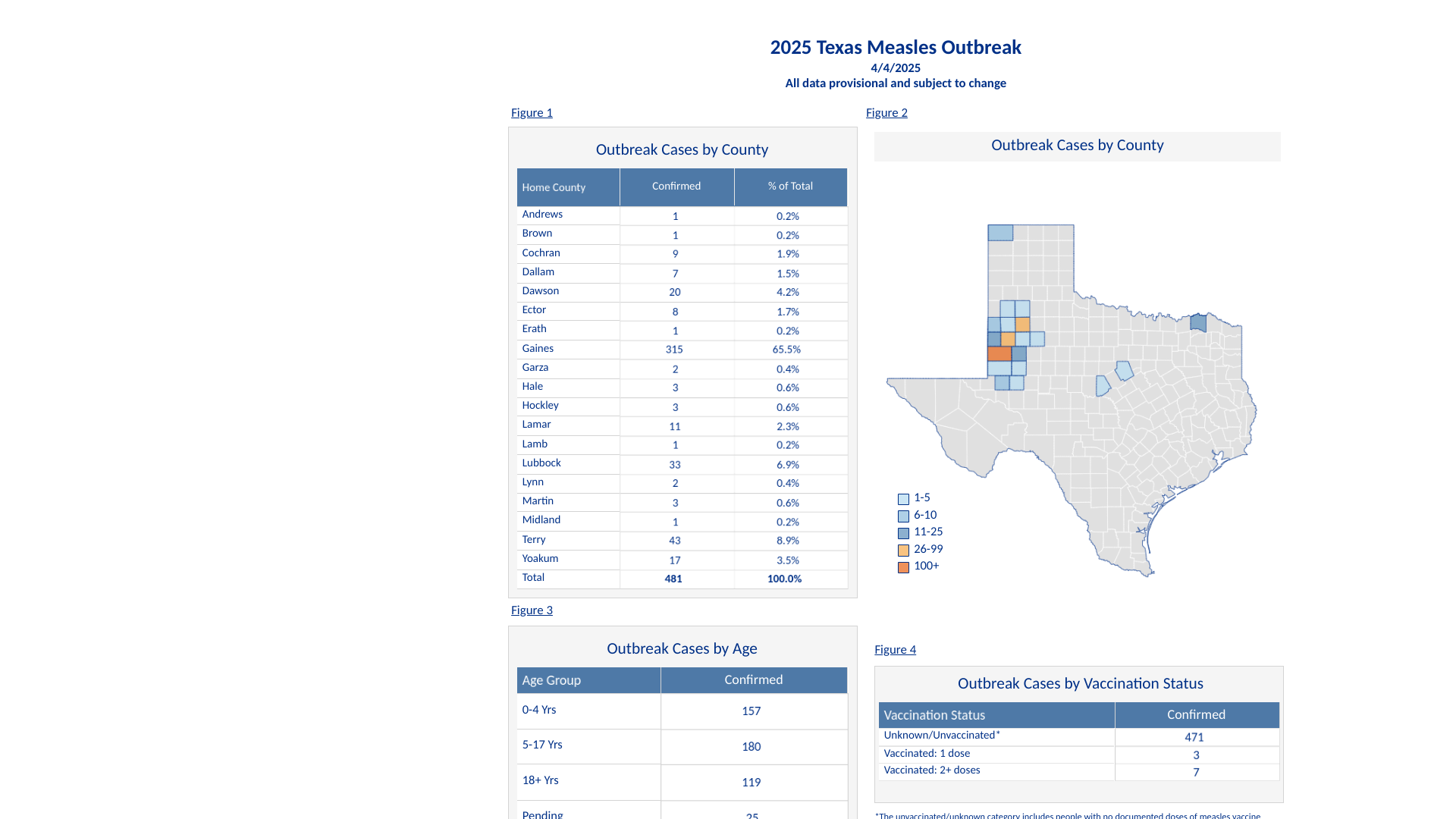
During the measles outbreak of 2025, a second measles-related fatality was confirmed by the Texas Department of State Health Services (DSHS).
This school-aged child was hospitalized in Lubbock, Texas, was not vaccinated, had no reported underlying conditions, and passed away last week.
According to the child’s doctors, the condition was described as measles pulmonary failure.
As of April 7, 2025, 489 measles cases have been confirmed in Texas's South Plains and Panhandle regions this year.
DSHS’s interactive dashboard and additional information about the outbreak can be found on the News & Alerts page.
Globally, the U.S. CDC and the World Health Organization (WHO) have issued various measles outbreak advisories in 2025. The WHO says the 'source of this measles outbreak is unknown.'
The WHO and the CDC disclosed that genotype D8 and B3 sequences have been detected in 2025.
According to a new report from the World Health Organization (WHO), Dengue is a mosquito-borne viral infection that has caused significant increases in severe flu-like illness across the globe.
For example, the WHO's Western Pacific Region continues to face a high burden of Dengue-like Illnesses in the Republic of Fiji, an island country in the South Pacific Ocean.
Dengue Situation Update #720, published on April 3, 2025, shows that Fiji has reported over 800 cases of Dengue each of the last two weeks. This data indicates a significant increase above the five-year median of 300 monthly cases in the early part of most years.
This year's Dengue outbreak may upset vacationers planning to visit this unique destination in 2025. Fiji visitors reached a new high of over 900,000 in 2024, an increase of 5.7% compared to last year.
To forewarn international visitors in 2025, the U.S. CDC includes Fiji in its reissued Global Dengue Travel Health Advisory, which says people should avoid being bitten by a virus-carrying mosquito.
Since the WHO's Strategic Advisory Group of Experts on Immunization shared recommendations for use of the QDENGA® vaccine in October 2023, about 40 countries have authorized its use. However, the United States has yet to authorize this second-generation Dengue vaccine.

When visiting areas in central Asia, travelers may become ill with fevers and headaches, occasionally leading to acute encephalitis. According to local health ministries, the cause could be Nipah virus (NiV).
It is estimated that about 40% of people with NiV may die.
According to the UK Travel Health Pro on April 4, 2025, most human infections result from direct contact with animals, particularly pigs and bats, in a few Asian countries, such as Bangladesh, India, Malaysia, the Philippines, and Singapore.
For example, Bangladesh has already reported three cases of NiV in people this year.
In the Indian state of Kerala, the Health Department has started awareness activities ahead of the bat breeding season in five districts considered to be hotspots for the zoonotic infection: Kozhikode, Malappuram, Kannur, Wayanad, and Ernakulam.
In 2023, Kerala experienced multiple Nipah outbreaks. Three of these outbreaks were contained to the Kozhikode district.
However, the causes of these NiV outbreaks remain unclear.
While these outbreaks are concerning, the UK says the 'risk of NiV infection for tourists to endemic countries is currently very low, if the following precautions are taken.'
Unfortunately, NiV preventive vaccines are unavailable in 2025.
The World Health Organization says Nipah vaccine candidates include live-attenuated and replication-defective recombinant vaccine platforms based on poxviruses, VSV, adenovirus, measles, rabies, and virus-like particles and subunit vaccines.
As of April 6, 2025, neither the U.S. Food and Drug Administration nor the European Medicines Agency has authorized a vaccine or treatment for Nipah, but clinical trials are ongoing.

While the U.S. CDC reports a continued decrease in influenza cases during the tail end of the 2024-2025 flu season, several cities are treating patients impacted by this respiratory disease.
According to the Wlagreens Flu Index®, the first week to show an increase in flu activity was the week ending on January 18, 2025.
Currently, the top ten cities treating people for the flu are:
- Harlingen-Weslaco-Brownsville-McAllen, Texas.
- New Orleans, La.
- Baton Rouge, La.
- Lafayette, La.
- El Paso, Texas (Las Cruces, N.M.)
- Chicago, Ill.
- Washington, D.C. (Hagerstown, Md.)
- Houston, Texas.
- Knoxville, Tenn.
- Honolulu, Hawaii.
For 11 years, the Walgreens Flu Index has provided an early and accurate view of disease trends. The Index offers detailed insights into flu activity across different markets.
This Index is based on retail prescription data for antiviral medications used to treat influenza at Walgreens locations nationwide. It is designed not to indicate the overall levels or severity of flu activity, but rather to highlight which populations are experiencing the highest incidence of influenza.
As of April 6, 2025, the CDC recommends flu shots for people at risk for this severe disease, especially for children. Unfortunately, there have been 168 influenza-associated deaths this flu season.
Flu shots remain available at most pharmacies throughout the United States.

Nigeria’s Ministry of Health announced today that it has received over 1,000,000 doses of the pentavalent meningococcal conjugate vaccine (Men5CV) to combat the meningococcus C and W outbreak in northern Nigeria.
This initial shipment will launch a crucial response campaign targeting individuals aged 1 to 29, the most affected demographic. The campaign will begin in Kebbi and Sokoto States and expand to Yobe State as more vaccine doses arrive.
As of April 4, 2025, this meningococcal outbreak has claimed more than 70 lives and affected over 800 individuals across 23 states.
In Africa's 'meningitis belt', seasonal outbreaks are common during the dry season, peaking between March and April due to low humidity and high dust levels.
According to the U.S. CDC, disease rates during epidemics can reach 1% of the local population.
Dr. Muhammad Ali Pate, Nigeria’s Coordinating Minister of Health and Social Welfare, stated in a press release, “The arrival of the Men5CV vaccines is a significant milestone in our fight against the meningitis outbreak."
Gavi, the Vaccine Alliance, funds the global stockpiles of vaccines against cholera, Ebola, meningitis, and yellow fever, accessible to all countries worldwide.
When visiting Nigeria in 2025, the CDC recommends routine and travel vaccines to prevent polio, measles, yellow fever, and diphtheria infections.

In Réunion Island, a French department located in the Indian Ocean, an unexpected chikungunya outbreak has overwhelmed the local population.
Since August 2024, about 20,242 chikungunya cases and two related fatalities have been confirmed across the island.
As of April 2, 2025, 14 newborns have been hospitalized following infection with the chikungunya virus. The disease can have serious, even fatal, consequences for newborns and infants.
Due to the acceleration in the number of cases and the spread of outbreaks to almost the entire territory in 2025, the first phase of the free chikungunya vaccination campaign is scheduled to begin on Monday, April 7, 2025. It will be carried out based on a medical prescription by a healthcare provider.
Accoring to ARS Réunion's media statement today, per the recommendations of the High Authority for Health and by decision of the health authorities, this first phase of the IXCHIQ® vaccination campaign primarily targets people aged 65 and over with comorbidities or chronic illnesses and who have not already contracted chikungunya.
The first 40,000 doses of Valneva's single-dose IXCHIQ® vaccine will not be available for pregnant women. Furthermore, this live attenuated vaccine is contraindicated in immunocompromised individuals.
Since 2023, IXCHIQ® has been approved by the U.S. FDA to treat chikungunya virus infections in adults at increased risk of exposure to the mosquito-transmitted disease. This indication now includes adolescents.
In March 2025, the U.S. CDC issued a Level 2 - Practice Enhanced Precautions Travel Health Advisory regarding Réunion's situation. The CDC wrote, ' Vaccination against chikungunya is recommended for people traveling to a destination with a current chikungunya outbreak.'
As of April 4, 2025, IXCHIQ is commercially offered at travel clinics and pharmacies in various countries, including the United States.

The Republic of Trinidad and Tobago Ministry of Health recently announced it is investigating a cluster of Malaria cases in South Trinidad, indicating a potential upsurge in 2025.
As of April 2, 2025, five malaria cases have been confirmed this year.
These five cases are in a well-defined geographic area, and the following field work has been conducted by the Insect Vector Control Division, after the identification of the first case on March 27, 2025:
The Ministry says Trinidad and Tobago, located east of Venezuela, is not endemic for malaria, and as such, most confirmed cases are imported and/or introduced.
Last year, over 200,000 people visited Trinidad and Tobago from a country in North America.
Over the period 2015 to 2024, there were 153 confirmed cases, which is an average of 15 cases per year.
Countries in the Region of the Americas, such as Trinidad and Tobago, reported over 500,000 malaria cases in 2023, a 5% increase from 2022.
In the United States, the Centers for Disease Control and Prevention (CDC) says millions of residents travel to countries where virus-carrying mosquitoes transmit malaria.
As of week #11 ending March 15, 2025, the CDC confirmed 209 malaria cases in the U.S. this year, with Florida reporting eight travel-related malaria cases.
During 2024, the CDC confirmed 436 measles cases in the U.S.
While two malaria vaccines are available in 2025, neither is offered in the U.S.

