Search API
The British Medical Journal (BMJ) recently confirmed that 300,000 people have become eligible for a shingles vaccination.
BMJ says shingles is caused when the varicella zoster virus, which reactivates, often decades after initial infection.
NHS England has announced that from September 1, 2025, immunosuppressed adults aged 18 to 49 will be newly eligible to receive the vaccine, marketed as Shingrix®.
The vaccine is currently available to people aged 65 to 79 and severely immunosuppressed people aged over 50. This group includes people with conditions such as leukaemia or lymphoma, or those who are undergoing chemotherapy.
The rollout to all severely immunosuppressed adults follows advice from the Joint Committee on Vaccination and Immunisation, which found that the risk of hospitalisation from shingles or those resulting in post-herpetic neuralgia was similar in younger immunosuppressed age groups to those who were already eligible.
Dr Amanda Doyle, National Director for Primary Care and Community Services at NHS England, commented in a press release, "Shingles can be seriously debilitating for older people and those with a severely weakened immune system, so following the latest expert guidance, the NHS is now expanding the potentially lifesaving jab to all severely immunosuppressed adults."
"The vaccine is safe and effective and significantly reduces the chance of developing shingles and becoming seriously unwell, so I'd urge anyone newly eligible to come forward for their protection as soon as possible.
As of September 6, 2025, in the United States, this shingles vaccine is generally available at retail pharmacies.

A significant increase in hepatitis A virus (HAV) infections has been reported in Austria, Czechia, Hungary, and Slovakia in 2025.
The Czechia State Institute of Health recently reported its multi-month HAV outbreak had reached 1,348 cases, with 15 people having died from the liver disease this year.
The State Health Institute (SZÚ) reported on September 3, 2025, that the majority of HepA cases have been recorded in Prague (436), Central Bohemia (202), and the Moravian-Silesian Region (118).
According to the European Centre for Disease Prevention and Control (ECDC), the increase in HAV infections is primarily affecting adults experiencing homelessness, individuals who use or inject drugs, and those living in poor sanitary conditions who have limited access to healthcare.
Local cases have also been reported among members of the Roma communities in both Czechia and Slovakia.
According to media reports, Prague was the most visited destination in Czechia, attracting about 1.2 million visitors in 2024.
"This outbreak reminds us that hepatitis A can cause serious illness and death, especially among people with limited access to healthcare and basic hygiene," said Ole Heuer, Head of Unit for One Health Related Diseases at ECDC, in a media release.
"We need to strengthen outreach, provide access to vaccination in groups more likely to be exposed, and ensure basic sanitation, especially in response to the increase in cases. More than health measures, they are equity measures."
Hepatitis A is a vaccine-preventable acute infection of the liver caused by a small, non-enveloped hepatotropic virus classified in the genus Hepatovirus within the family Picornaviridae.
The U.S. CDC recommends vaccination for unvaccinated travelers one year old or older traveling to Czechia.
And unvaccinated travelers who are over 40 years old, are immunocompromised, or have chronic medical conditions planning to depart for a risk area in less than 2 weeks should receive the initial dose of vaccine and, at the same appointment, receive immune globulin.
As of September 6, 2025, HAV vaccines are generally available at health clinics and pharmacies in Europe and the United States.

The U.S. Centers for Disease Control and Prevention (CDC) today reissued its Level 2, Practice Enhanced Precautions, Travel Health Advisory for chikungunya outbreaks in countries/territories located in the Indian Ocean.
On September 5, 2025, the CDC confirmed outbreaks of chikungunya in Bangladesh, Kenya, Madagascar, Somalia, and Sri Lanka.
Other outbreaks have occurred in Africa, the Americas, Asia, Europe (specifically in France), the Caribbean, and the Indian and Pacific Oceans.
Chikungunya disease is caused by the chikungunya virus and is transmitted to humans through the bites of infected mosquitoes. Most people infected with the chikungunya virus develop symptoms, according to the CDC.
If you are pregnant, consider reconsidering travel to the affected areas, especially if you are nearing the delivery of your baby. Mothers infected around the time of delivery can pass the virus to their baby before or during delivery.
Newborns infected in this way or by a mosquito bite are at risk for severe illness, including poor long-term outcomes.
The CDC advises vaccination (VIMKUNYA) for most travelers visiting an area with a chikungunya outbreak in September 2025.
Across the USA, local experts do offer their advice on eligibility for mpox and other travel vaccines.

French Polynesia, located in the southwest Pacific Ocean, has been a dream vacation destination for decades.
However, these islands are also home to dengue fever, which is transmitted by the bite of infected mosquitoes.
According to Bulletin de surveillance sanitaire de Polynésie française n°34, published on September 2, 2025, there were 22 new dengue cases (19 confirmed last week.
And the blue alert for DENV-1 remains in effect.
Since November 2023, a total of 2,577 cases have been recorded.
To alert international travelers of this health risk, the U.S. CDC's Travel Health Advisory issued on August 21, 2025, included French Polynesia.
The CDC identified the island groups of the Society Islands (Tahiti, Moorea, and Bora Bora), the Marquesas Islands (Hiva Oa and Ua Huka), and the Austral Islands (Tubuai and Rurutu).
The CDC reported that these countries are experiencing higher-than-usual numbers of cases and have identified a higher-than-expected number of dengue cases among U.S. travelers returning from those countries.
While a second-generation dengue vaccine is available in various countries, it is not offered in the USA.
Fortunately, several dengue vaccine candidates are conducting late-stage research focused on preventing all four virus types from infecting people.
Mumbai, the capital city of the Indian state of Maharashtra, with a population of over 12 million residents, recently reported a significant increase in vector-borne diseases in 2025.
As of September 2025, the Brihanmumbai Municipal Corporation's (BMC) health report reveals a surge in cases of chikungunya, dengue, and malaria, which are impacting Mumbai's residents, formerly known as Bombay.
Daijiworld Media reported BMC data shows Mumbai has confirmed 5,706 malaria cases, a 42% rise compared to 2024.
Chikungunya cases increased from 210 in 2024 to 485 this year.
Dengue cases increased from approximately 1,979 to 2,319 in 2025.
To contain the spread, the BMC has restarted its 'Zero Mosquito Breeding' initiative to reduce the number of virus-carrying vectors.
BMC officials said cases are expected to decline once monsoon activity eases.
To alert international visitors, both the U.S. CDC and the UK government have issued travel vaccine advice for those planning trips to Maharashtra in 2025. Mumbai attracts almost 6 million tourists annually.
The CDC recommends that chikungunya vaccination may be considered for individuals traveling to or residing in this location for an extended period (e.g., 6 months or more).

The World Health Organization (WHO) recently confirmed that the global cholera situation continues to deteriorate in 2025.
Cholera is resurging in several countries, with some that had not reported substantial case numbers in years.
Since January and through August 17, 2025, the WHO has reported a total of 4,738 cholera/Acute Watery Diarrhoea-related fatalities from 31 countries, with six of the 31 countries reporting case fatality rates (CFR) above 1%.
For example, suspected cholera cases have been reported from two provinces of the Republic of Chad. Among these, Chokoyane is the most affected area, accounting for 541 cases and 25 deaths, with a district-specific CFR of 4.6%.
While Cholera is an acute diarrheal infection caused by consuming food or water contaminated with the bacterium Vibrio cholerae, primarily associated with poor sanitation and limited access to safe water, it can be prevented with vaccination.
As of September 5, 2025, the U.S. CDC's Travel Health Advisories for these countries advise cholera vaccination before departing abroad. Most cholera cases diagnosed in the U.S. are related to international travel.
In the U.S., Vaxchora® (CVD 103-HgR) is the only U.S. FDA-approved vaccine available at travel clinics and pharmacies.

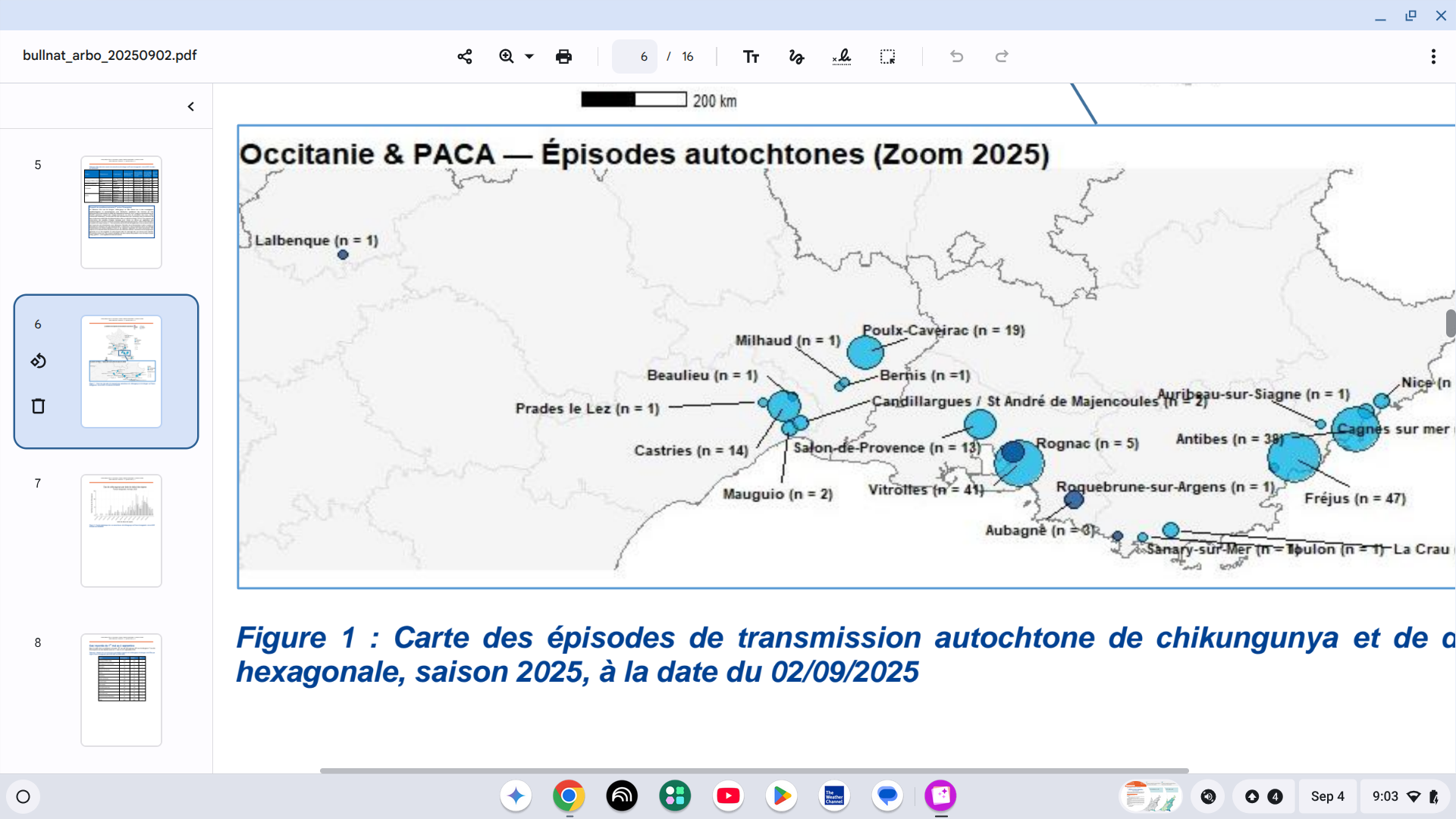
Chikungunya virus disease patients have been reported in 14 countries/territories in Europe this year. Several of these countries are positioned along the Mediterranean Sea.
In mainland France, the Health Agency reported on September 4, 2025, that an unprecedented situation has developed, with the number of locally acquired cases exceeding previously unseen levels.
As of early September 2025, 34 episodes of chikungunya had been reported, totaling 301 cases.
Mosquitos have transmitted the virus to people in the Provence-Alpes-Côte d'Azur, Corsica, Occitanie, Auvergne-Rhône-Alpes regions, already affected in previous years, and for the first time this year in Grand Est, Nouvelle-Aquitaine, and Bourgogne-Franche-Comté.
Additionally, 957 international travelers have been diagnosed with chikungunya while in France.
When planning a trip to France this fall, health agencies in the United Kingdom and the United States recommend speaking with a travel vaccine expert regarding chikungunya vaccination options.
In the U.S., travel clinics and pharmacies offer a U.S. FDA-approved chikungunya vaccine.