Search API
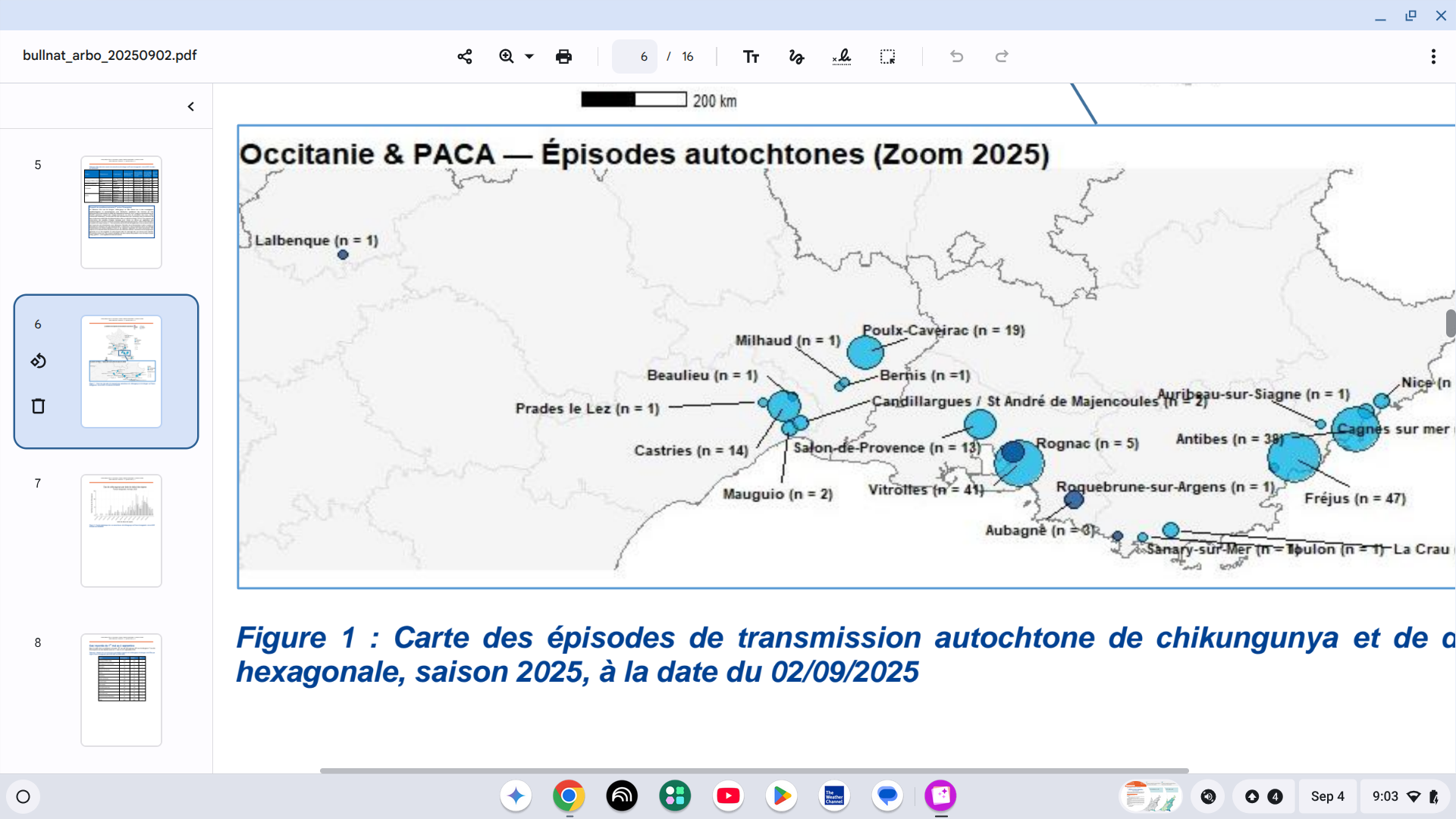
Chikungunya virus disease patients have been reported in 14 countries/territories in Europe this year. Several of these countries are positioned along the Mediterranean Sea.
In mainland France, the Health Agency reported on September 4, 2025, that an unprecedented situation has developed, with the number of locally acquired cases exceeding previously unseen levels.
As of early September 2025, 34 episodes of chikungunya had been reported, totaling 301 cases.
Mosquitos have transmitted the virus to people in the Provence-Alpes-Côte d'Azur, Corsica, Occitanie, Auvergne-Rhône-Alpes regions, already affected in previous years, and for the first time this year in Grand Est, Nouvelle-Aquitaine, and Bourgogne-Franche-Comté.
Additionally, 957 international travelers have been diagnosed with chikungunya while in France.
When planning a trip to France this fall, health agencies in the United Kingdom and the United States recommend speaking with a travel vaccine expert regarding chikungunya vaccination options.
In the U.S., travel clinics and pharmacies offer a U.S. FDA-approved chikungunya vaccine.
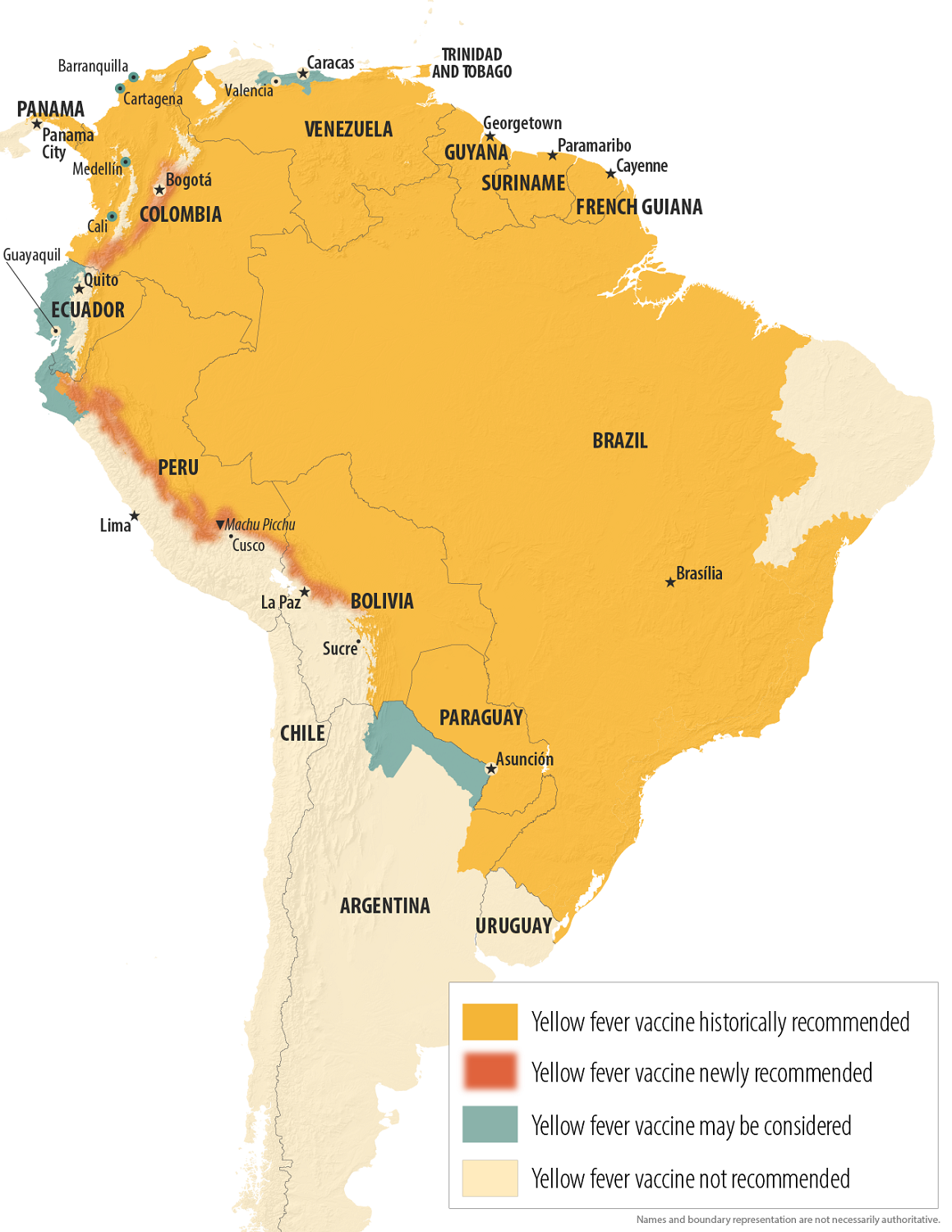
The U.S. Centers for Disease Control and Prevention (CDC) today announced an update to its Level 2 Travel Health Advisory for the Republic of Colombia, due to a yellow fever outbreak.
On September 3, 2025, the CDC reported an increase in cases in new areas in the South American country.
In a Facebook post, the Health Ministry reported that between 2024 and 2025, 132 yellow fever (YF) cases were registered, resulting in 57 deaths, in the following Colombian departments: Tolima, Huila, Cauca, Nariño, Putumayo, Caldas, Meta, Vaupés, Guaviare, and Caquetá.
The CDC recommends that travelers to these newly affected areas get vaccinated at least 10 days before traveling abroad, as yellow fever is a severe viral disease.
Last year, the Colombian government declared a nationwide health emergency to alert residents and visitors to the situation.
Colombia welcomed over 6.5 million international visitors.
Recently, the U.S. Embassy in Bogota issued an alert stating visitors should reconsider travel to the Valle del Cauca Department due to civil unrest.
As of September 2025, YF is a vaccine-preventable disease, and proof of vaccination is required to enter various countries, including Colombia.
A booster dose may be given to eligible travelers or those who received their last dose of the YF vaccine at least 10 years prior and will be in a higher-risk setting, according to the CDC.
"With yellow fever cases rising in Colombia, the CDC has expanded the list of areas where vaccination is now recommended. We're seeing a similar trend in parts of Peru and Bolivia, too," commented Jeri Beales, MSN, RN, BS.
This isn't a mosquito-borne virus to take lightly—yellow fever can be deadly, with fatality rates as high as 60% in severe cases."
"If you're planning a trip to Colombia, consult with a travel health provider about getting vaccinated. It's highly effective and usually offers lifelong protection. Still, it's only available at certified clinics, so schedule ahead—ideally a few weeks before you leave to give the vaccine time to create a robust immune response so you're fully protected before arriving," added Beales, vaccination leader at Destination Health, located in the greater Boston, MA, area.
In the United States, the YF-VAX vaccine is commercailly offered at travel vaccination retailers.
Note - vaccine expert insight added on September 6, 2025.
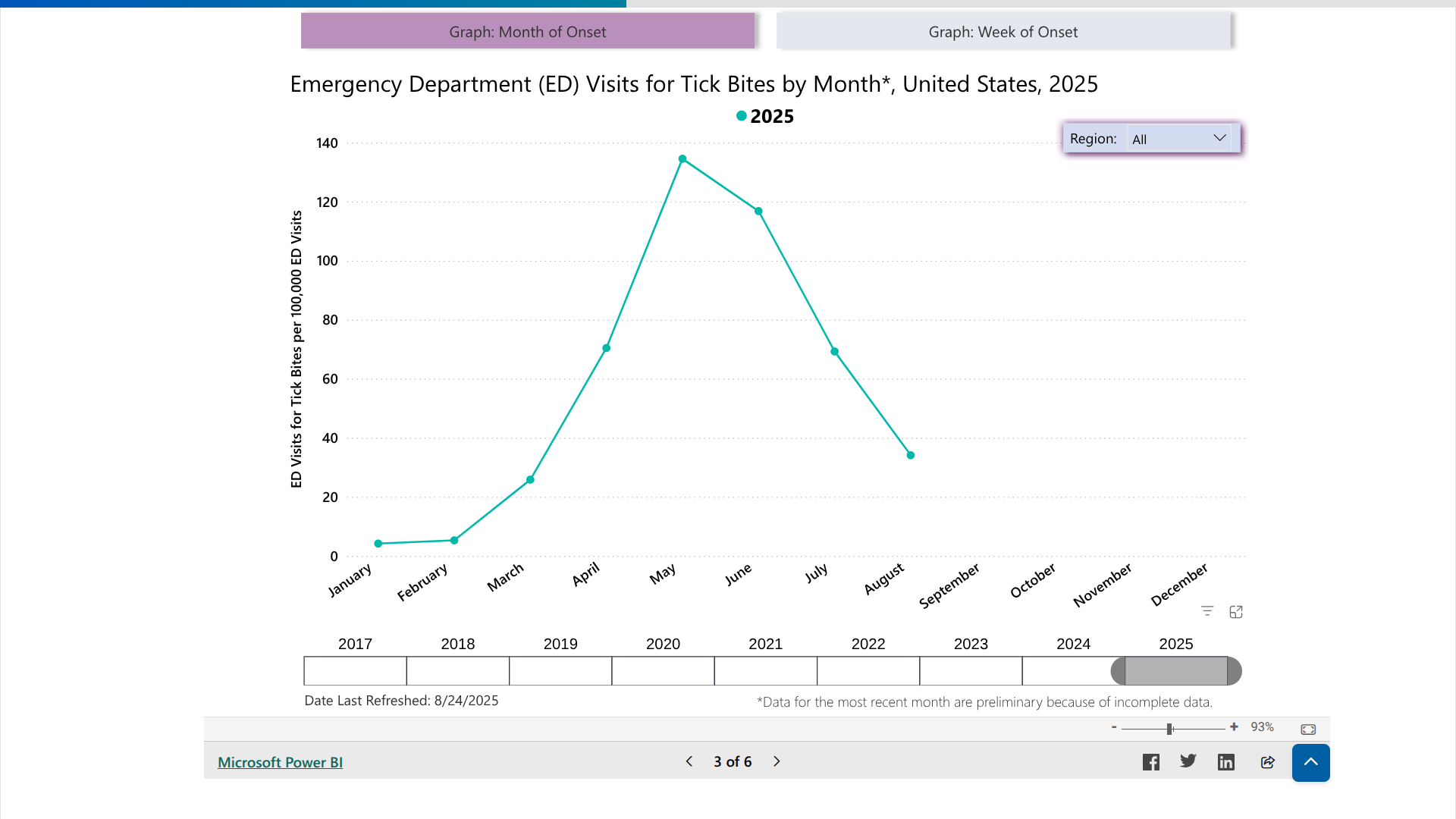
With Lyme disease cases steadily declining in the United States, the only vaccine candidate conducting late-stage clinical research announced very encouraging news today.
On September 3, 2025, Valneva SE reported positive immunogenicity and safety data from the ongoing Phase 2 study of Lyme disease vaccine candidate, VLA15.
The strong anamnestic immune response and favorable safety profile following a third booster dose were consistent with those reported after receiving previous annual booster doses, further demonstrating compatibility with the anticipated benefits of a yearly vaccination before each Lyme season, wrote the company.
Juan Carlos Jaramillo, M.D., Chief Medical Officer of Valneva, commented in a press release, "These latest data further reinforce the potential benefits of booster doses across all evaluated age groups.... as the disease continues to expand geographically, it remains a pressing unmet medical need affecting communities across the Northern Hemisphere."
"Each set of positive results moves us closer to the possibility of making this vaccine available to both adults and children living in Lyme-endemic areas."
Lyme disease (Lyme borreliosis) is a bacterial disease transmitted to humans through the bite of infected ticks, initially detected in 1977 in Lyme, Connecticut, and now found in most northeastern states.
In the UK, ticks that carry Lyme disease are most active in the spring and summer. Approximately 4% of ticks in England and Wales are infected with Lyme disease.
As of September 2025, the U.S. Centers for Disease Control and Prevention's Tick Bite Data Tracker displays case data and maps for the U.S.
The Communicable Diseases Agency of the Republic of Singapore has reported a total of 21 chikungunya cases this year.
As of August 28, 2025, this number has already surpassed the total recorded for all of 2024, which was 15 cases.
The increase began in May 2025, primarily due to travelers returning from areas affected by the chikungunya outbreak in China's Guangdong Province and several French Territories in the western Indian Ocean.
In 2024, this sovereign island country and city-state in Southeast Asia welcomed approximately 16.5 million international tourists, representing a 20% increase from the previous year.
In early August, Professor Ooi Eng Eong from Duke-NUS Medical School explained to the media that although chikungunya is less deadly than dengue, it can be debilitating. Chronic joint discomfort can limit physical activity and impact overall quality of life.
Although the U.S. CDC has not issued a Travel Health Advisory for chikungunya related to Singapore, the UK's Travel Health Pro indicates that there is a risk of chikungunya in this country.
As of September 3, 2025, the UK recommends that international travelers take precautions to avoid mosquito bites, especially during daytime hours.
Additionally, vaccination may be considered for individuals aged 12 years and older who meet specific eligibility criteria.
In the United States, the FDA has approved a chikungunya vaccine, which is available at travel clinics and pharmacies.

Since the Zika virus was first detected in the Region of the Americas in May 2015, the Pan American Health Organization (PAHO) has published counts of cases reported by member countries.
However, given the high proportion of asymptomatic individuals infected with the Zika virus, the lack of specificity in clinical presentation among cases, and the complexity of laboratory diagnosis in the context of co-circulation of closely related viruses such as chikungunya and dengue, underreporting of Zika virus cases is probable, wrote the PAHO.
While Brazil has been the multi-year leader in reporting Zika cases, the Argentine Republic has been confronted with a measurable outbreak in 2025.
As of September 2, 2025, the PAHO reported 730 Zika cases for the year. This data compares with 564 cases for all of 2024.
Currently, the U.S. CDC has not issued a Travel Health Advisory regarding Zika in Argentina.
However, the United Kingdom Travel Health Pro states there is a risk of the Zika infection in this country. Specific affected areas within Argentina where mosquitoes are spreading the virus are not available.
Both the CDC and the UK confirm that pregnant women should discuss the suitability of travel and the potential risks that the Zika virus may present with their healthcare provider before traveling abroad.
From a prevention and treatment perspective, no Zika vaccine or medication is expected to be available in 2025.

According to the WHO's Multi-country External Situation Report #57, published on August 28, 2025, all clades of the monkeypox virus (MPXV) continue to circulate in several countries.
The WHO writes that 'when mpox outbreaks are not rapidly contained and human-to-human transmission is not interrupted, they continue to pose a risk of sustained community transmission.'
In July 2025, 47 countries reported a total of 3,924 confirmed cases, including 30 deaths (case fatality ratio 0.8%).
China, Germany, Türkiye, and the United Kingdom have reported additional cases of mpox due to clade Ib MPXV since the last situation report.
These new cases have been linked to international travel.
On August 20, 2025, the WHO Director-General extended the standing recommendations for mpox until August 2026 to further prevent or reduce the international spread of mpox, as well as its impact on health.
Both the WHO and the U.S. Centers for Disease Control and Prevention (CDC) recommend receiving your first mpox vaccine at least 6 weeks before travel. After completing your first and second vaccine doses, which are given 4 weeks apart, it takes about two more weeks to get the best protection against mpox.
The majority of U.S. cases of clade II mpox continue to be reported in people who are not vaccinated or have received only one dose.
Several cases have recently been tied back to an outbreak in Sierra Leone, Liberia, and other West African countries.
The CDC suggests that whether or not you've been vaccinated (JYNNEOS®, MVA-BN®, IMVAMUNE®), you continue to reduce your risk of getting mpox.

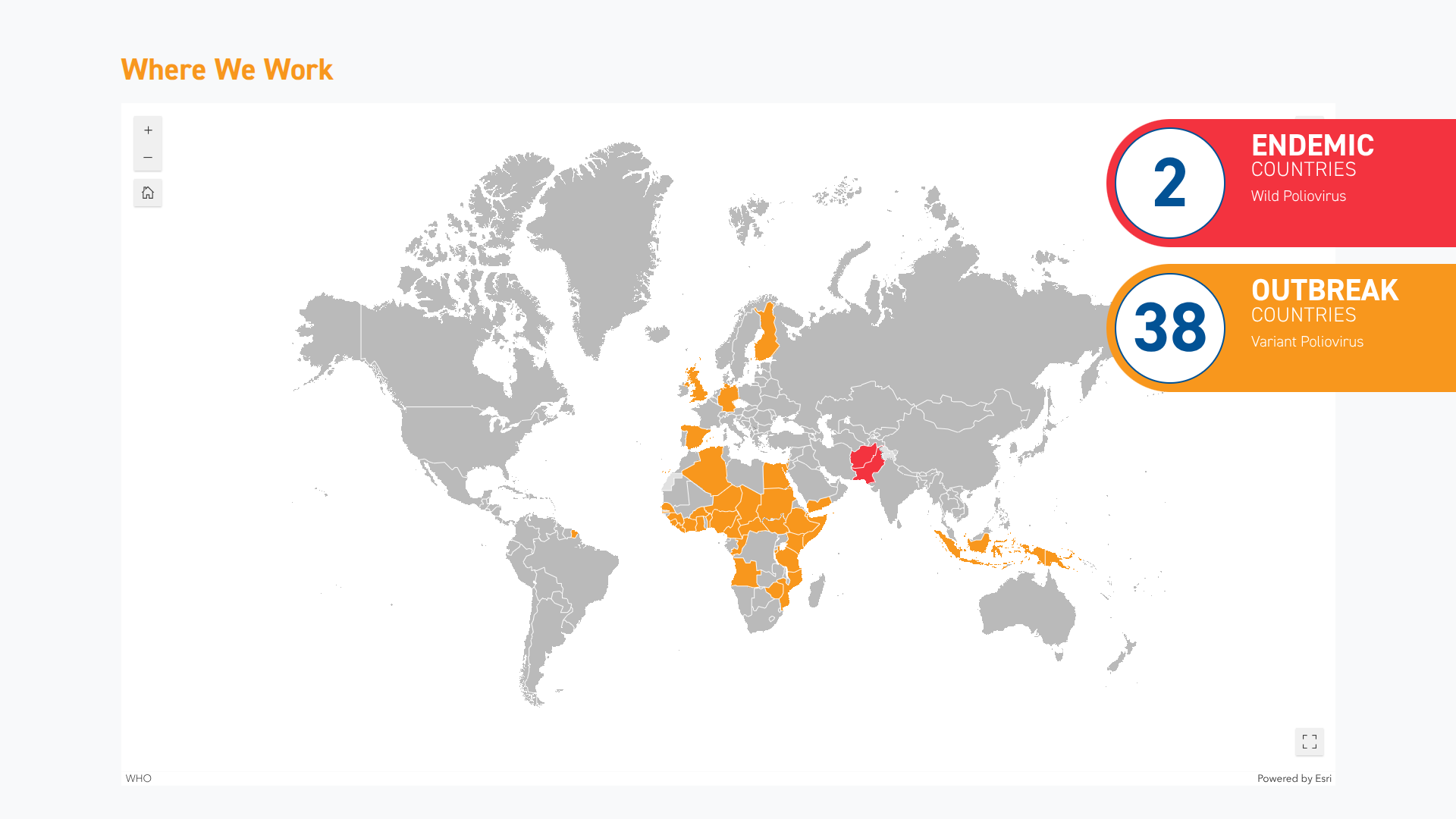
When the World Health Organization confirmed in June 2025 that the spread of the poliovirus remained a Public Health Emergency of International Concern, it identified several countries where visitors are at risk of contracting this severe disease.
As of August 27, 2025, new data from the Global Polio Eradication Initiative (GPEI) reveal an unexpected surge in polio cases in the Republic of Yemen, situated in southern Arabia.
According to the GPEI, 25 circulating vaccine-derived poliovirus type 2 (CVDPV2) cases were reported this week. This updated data brings the number of cases in Yemen for 2024 to 187 and 29 for 2025.
'The recent increase in reported cases and environmental sample isolates from 2024 and 2025 is not particularly linked to an increase in poliovirus transmission, but rather to retrospective testing,' wrote the GPEI.
CVDPV2 is a strain of poliovirus that can emerge in under-vaccinated populations when the oral polio vaccine (OPV) strains genetically revert to a form that can cause paralysis.
To address the shortcomings of this vaccine, the nOPV2 vaccine has been deployed over 1 billion times in various countries.
In the United States, the inactivated polio vaccine (IPV) was developed in 1955 and has been offered since 2000. IPVs produce antibodies in the blood that target all three types of poliovirus, thereby preventing the virus from spreading.
As of September 2, 2025, the U.S. CDC recommends IPV booster doses for specific travelers visiting areas where poliovirus has been detected, such as Israel and Germany.
IPVs are currently offered at travel clinics and pharmacies in the U.S.