Search API
Public Health France reported (Semaine 39-2025) today that a total of 570 locally acquired cases of Chikungunya Fever have been reported since the beginning of 2025.
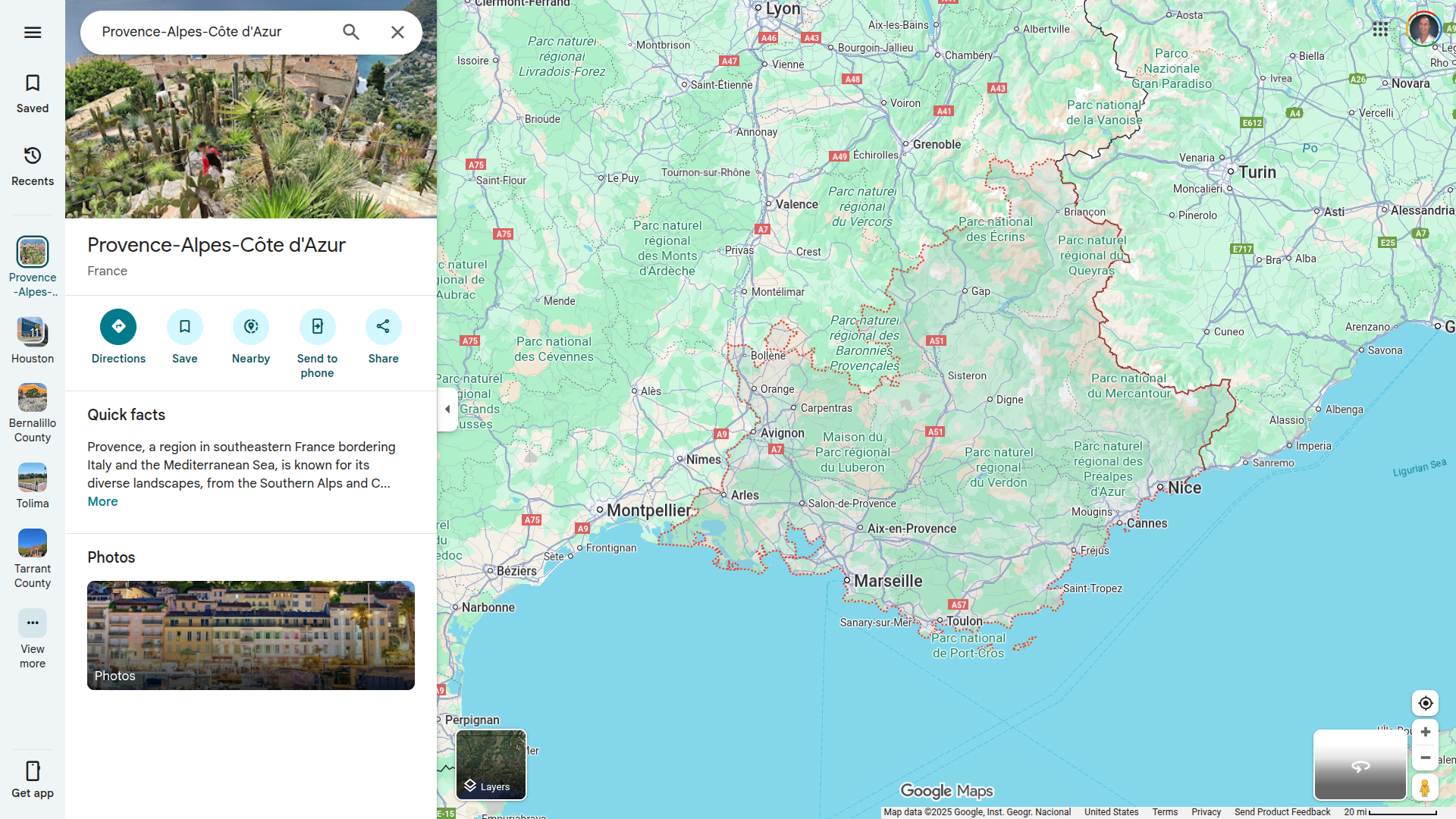
The Paca region, a favorite tourist destination, is the most affected by the indigenous circulation of the Chikungunya virus.
As of September 25, 2025, mosquito-transmitted cases have been reported from Provence-Alpes-Côte d'Azur, Corsica, Occitanie, Auvergne-Rhône-Alpes, Île-de-France, Grand Est, Bourgogne-Franche-Comté, and Nouvelle-Aquitaine.
Additionally, the Ministry confirmed 993 imported cases of Chikungunya, many of whom had visited the French Departments of Mayotte and Réunion.
In total, the ongoing Chikungunya outbreak in France may set new records for the country.
As an option to prevent this disease, approved vaccines are offered in France, throughout Europe, and at travel clinics and pharmacies in the United States.
While most rabies cases in the United States are from a bite by an infected bat, a broad investigation was begun in Coffee County, Alabama, after a horse was confirmed positive for Rabies. This viral disease is almost always fatal if untreated.
The owner, family members, and a neighbor who was exposed have begun Rabies post-exposure treatment.
The horse's owners reported noticing scratch marks on her nose, and she began rubbing and showing irritation in that area. The ill horse stopped eating, symptoms worsened over the 72 hours before her death, and she became violent and started attacking and biting herself.
The owners assumed the scratches came from a fox or raccoon that she had approached. Other unvaccinated horses on the property are being observed for a period of time.
Dr. Dee W. Jones, Alabama State Public Health Veterinarian, said in a press release on September 24, 2025, "Rabies is not as common in horses as in wildlife and domestic animals, but it is not rare. Rabies vaccines are available for horses and other livestock if recommended by a veterinarian. I encourage all horse owners to make Rabies a part of their annual vaccination, even though it is not legally required like in dogs and cats."
Vaccinating animals reduces the risk of rabies infection should exposure occur; thus, vaccinations protect animals, as well as their owners and caretakers.
Rabies prevention is multifaceted. It involves people taking precautions with wildlife, ensuring their pets are up to date on rabies vaccinations, and consistently reporting any animal bites or other exposures to their medical provider and the state health department.

The New Mexico Department of Health (NMDOH) today reported a case of plague from Bernalillo County, the second case of the year.
The 77-year-old man was hospitalized in Albuquerque and has since been discharged.
NMDOH stated in a media release on September 24, 2025, that there have been no deaths from plague in 2025.
Since 2000, an average of two human plague cases have been reported per year in New Mexico.
According to the U.S. CDC, an average of seven human plague cases are reported each year in the United States.
Plague is a bacterial disease primarily affecting rodents and is typically transmitted to humans through the bites of infected fleas, but can also be transmitted by direct contact with infected animals, including rodents, wildlife, and pets.
"The bacterium that causes plague can be found in wild rodents and their fleas throughout New Mexico," commented Dr. Erin Phipps, state public health veterinarian for the NMDOH.
"Keeping pets on the flea control product recommended by your veterinarian helps protect them and your family."
Symptoms of plague in humans include sudden onset of fever, chills, headache, and weakness. In most cases, there is a painful swelling of the lymph node in the groin, armpit, or neck.
Symptoms of plague in cats and dogs include fever, lethargy, and loss of appetite. There may be a swelling in the lymph node under the jaw.
See your doctor about any unexplained illness you may have involving sudden and severe fever.
With prompt diagnosis and appropriate antibiotic treatment, the fatality rate in people and pets can be significantly reduced. Physicians who suspect plague should promptly report to the NMDOH.
Plague vaccines have been used since the late 19th century; however, their availability remains limited in 2025.

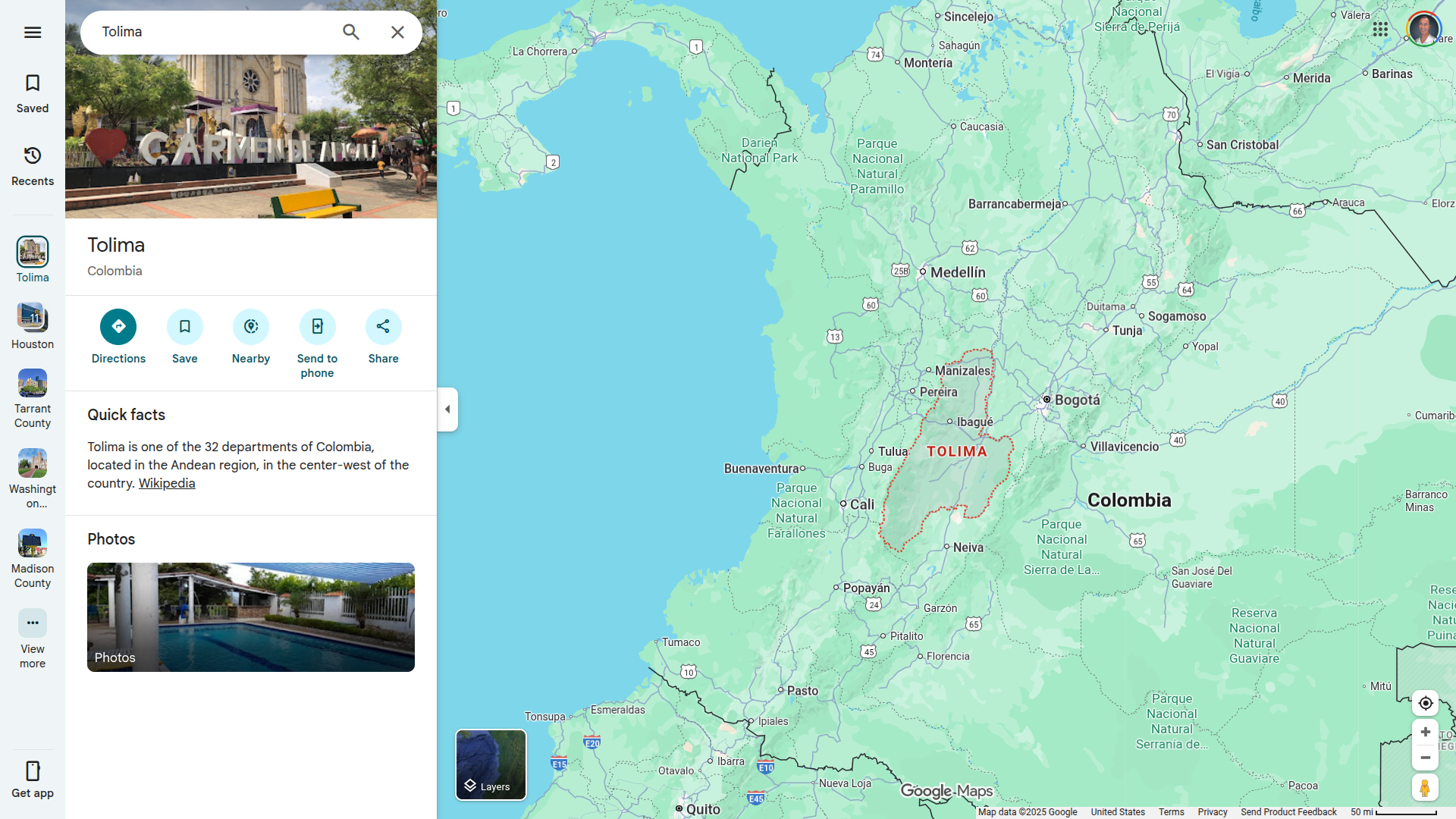
On September 23, 2025, a Facebook post reported a total of 134 confirmed yellow fever cases (resulting in 58 deaths) in the Republic of Colombia for 2025.
The majority of cases have been reported in the Tolima Department, with 114 cases and 43 deaths.
This department is located west of Bogota, Colombia's capital city.
Other yellow fever cases have been reported in Huila, Cauca, Nariño, Putumayo, Caldas, Meta, Vaupés, and Guaviare y Caquetá.
Published in early September, the U.S. CDC's Level 2 Travel Health Notice stated some of these cases have been reported in new areas that border areas where vaccination has historically been recommended (see map). Travelers to these newly affected areas are now recommended to get vaccinated.
A booster dose may be given to sure travelers or those who received their last dose of yellow fever vaccine at least 10 years previously and will be in a higher-risk setting, such as areas in Colombia where cases have been reported.
In the United States, yellow fever vaccines are commercially offered at travel clinics and pharmacies.
Madison County Public Health (MCPH) recently announced its first recorded human case of eastern equine encephalitis (EEE) in Madison County, New York.
On September 22, 2025, MCPH stated in a press release that it had been notified of a confirmed case in a Madison County resident by the Wadsworth Center and is currently investigating. The individual is currently hospitalized for EEE infection.
This disease is often fatal (30%), and many patients who survive EEE experience neurologic impairment.
"Temperatures are getting cooler, and although we are seeing a significant decrease in mosquitoes, they remain not only a nuisance, but a potential health threat. Residents should continue to take steps to prevent mosquito bites to reduce the risk of mosquito-borne disease infection," MCPH Director Eric Faisst stated.
In July 2025, the New York State Department of Health notified MCPH of a mosquito pool that tested positive for EEE. From 1971 through 2024, 12 individuals in New York were diagnosed with EEEV; seven of them died.
About one year ago, a Ulster County resident died following an EEE infection.
This is concerning news since Madison County is located adjacent to Syracuse, New York, which has a population of over 600,000.
EEE is a rare but severe viral disease spread by infected mosquitoes that can affect people and horses. People of all ages are susceptible to infection. While most people bitten by an infected mosquito will not develop symptoms, severe cases may begin with the sudden onset of headache, high fever, chills, and vomiting.
There is no commercially available human vaccine or treatment for EEE. The best protection is to prevent mosquito bites, says MCPH.
The World Health Organization (WHO) recently published its 58th situation report on the multi-country outbreak of mpox, detailing the global epidemiological situation and providing an update on the continuing emergency in Africa, where over 90% of cases have been confirmed. Both clades of the monkeypox virus (MPXV) continue to circulate.
As of September 19, 2025, the WHO reported 59 countries across all WHO regions reported a total of 3,780 confirmed cases, including 15 deaths (case fatality ratio 0.4%) in August.
The Eastern Mediterranean and European regions reported an increase in cases in August compared to July 2025.
Nineteen countries in Africa have reported active mpox transmission in the past six weeks.
Clade IIb MPXV continues to be mostly reported in West Africa, Central African countries report both clade Ia and clade Ib MPXV, and East African countries report clade Ib MPXV.
Even though the WHO has downgraded the global Mpox situation, it continues to provide guidance and technical support to countries on targeted vaccination strategies. WHO is supporting countries on planning for the use of dose-sparing options (single dose or intradermal fractional dosing) of MVA-BN vaccine.
More than 1.1 million MVA-BN vaccine doses have been administered.
Mpox vaccination activities have started in 11 countries with the MVA-BN vaccine (Angola, Côte d'Ivoire, the Central African Republic, Democratic Republic of the Congo, Kenya, Liberia, Nigeria, Rwanda, Sierra Leone, South Africa, and Uganda). Most countries are implementing a single-dose strategy targeting population groups at high risk of exposure to the human-to-human transmitted virus.
The U.S. CDC recently stated that clade II mpox has become endemic in Liberia and Sierra Leone.
To ensure the United States has an ample supply of vaccines, Emergent BioSolutions Inc. recently announced a $56 million contract to supply ACAM2000® (Smallpox and Mpox (Vaccinia) Vaccine, Live) to the U.S. government.
Deliveries are expected to begin in September.
In the United States, the MVA-BN (JYNNEOS) vaccine remains available at health clinics as of September 22, 2025.

An unprecedented situation arose during the summer of 2025, with the first locally acquired cases of Chikungunya virus disease detected as early as June, notably affecting the Grand Est region for the very first time.
Since the beginning of 2025, France has reported 480 cases of Chikungunya virus infection.
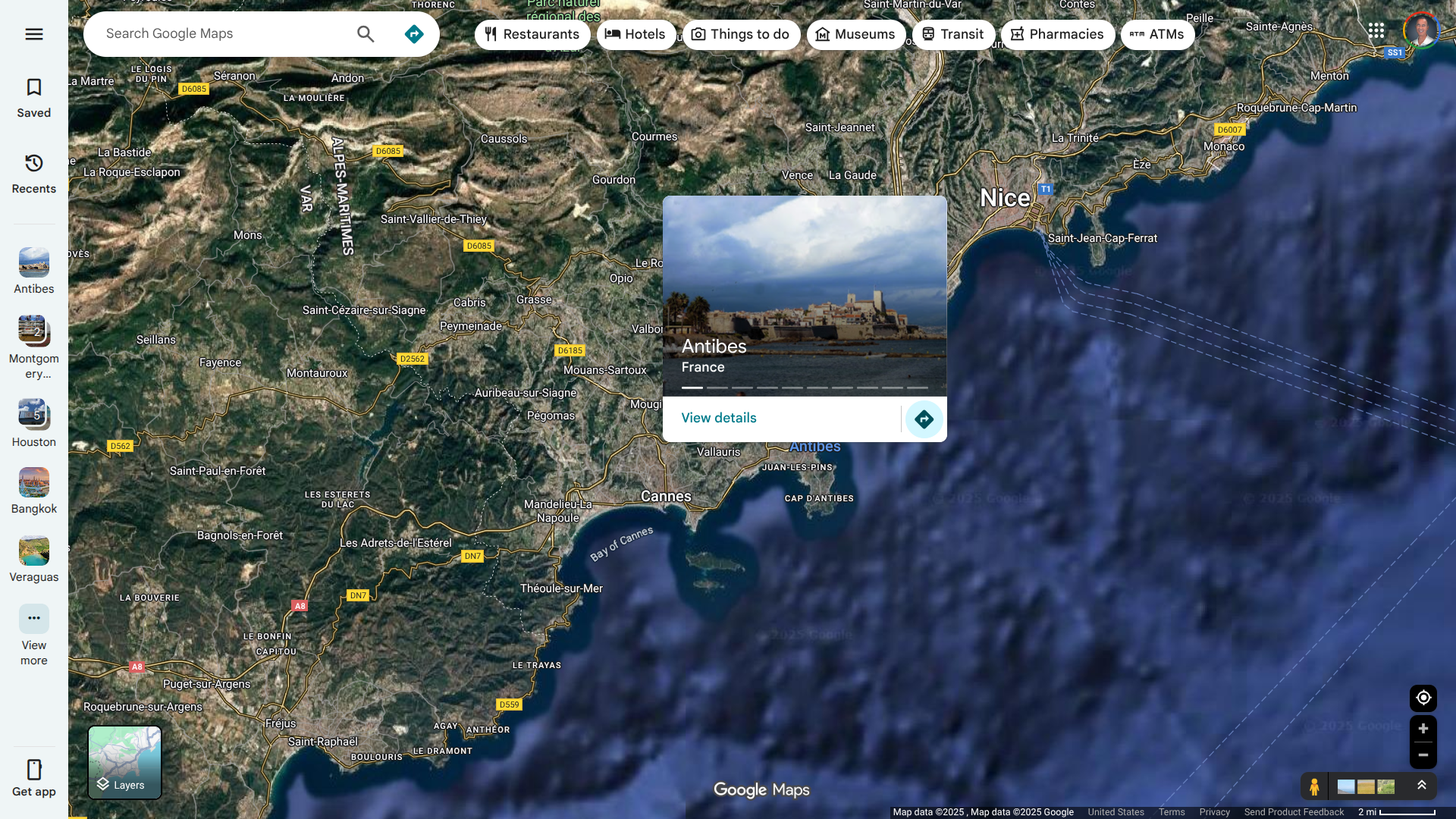
In mid-September 2025, the French Health Ministry reported 97 new locally acquired cases of Chikungunya in thirty-eight active clusters. The largest cluster is located in Antibes and consists of 87 cases.
This area of France's Mediterranean coast is a popular vacation destination, located between Cannes and Nice.
The European Centre for Disease Prevention and Control (ECDC) stated on September 12, 2025, that Chikungunya is not endemic in mainland Europe, with the majority of cases being travel-related.
However, when environmental conditions are favourable, in areas where the Aedes aegypti mosquito is established, viraemic travel-related cases may lead to local transmission of the virus, as demonstrated by the sporadic events of chikungunya virus transmission since 2007.
For more information on locally acquired Chikungunya cases in Europe, refer to the ECDC's seasonal surveillance report.
In addition to avoiding mosquito bites, the French and U.S. governments have approved vaccines for use in areas with Chikungunya outbreaks.
As of September 22, 2025, the U.S. CDC advises international travelers to speak with a travel vaccine expert regarding immunization options before traveling abroad.