Search API
The Czech Republic (Czechia) is currently experiencing what may be the largest hepatitis A epidemic in the last 46 years, as reported by Ivana Lesková from MF DNES.
Since the arrival of the virus from Slovakia in April 2024, the State Institute of Health has documented 2,141 cases of hepatitis A and 26 related fatalities, including ten in Prague.
As of October 28, 2025, the Institute of Health has noted a significant increase in demand for hepatitis A vaccinations.
This year alone, more than 127,000 doses have been administered—almost double the total from last year. Due to this surge in demand, there are currently shortages of the vaccine.
However, the State Institute for Drug Control has announced to the local media that extraordinary vaccine shipments are on their way to the Czech Republic.
This vaccine shortage extends the HepA risk to over 20 million international travelers who may visit Czechia this year.
Currently, the U.S. CDC recommends that unvaccinated travelers aged 1 year or older visiting Czechia in 2025 speak with a healthcare provider about immunization options.
For international travelers who are allergic to a vaccine component, they should receive a single dose of immune globulin, which provides adequate protection for up to 2 months, depending on the dosage given.
Unvaccinated travelers who are over 40 years old, are immunocompromised, or have chronic medical conditions planning to depart for a risk area in less than 2 weeks should get the initial dose of vaccine and, at the same appointment, receive immune globulin, says the CDC.
According to the Pan American Health Organization (PAHO) mosquito-transmitted disease dashboard, Mexico has reported over 109,771 dengue fever cases in 2025.
As of October 27, 2025, there have been 48 dengue-related fatalities confirmed this year.
Last year, Mexico reported 558,846 dengue cases and 478 related fatalities.
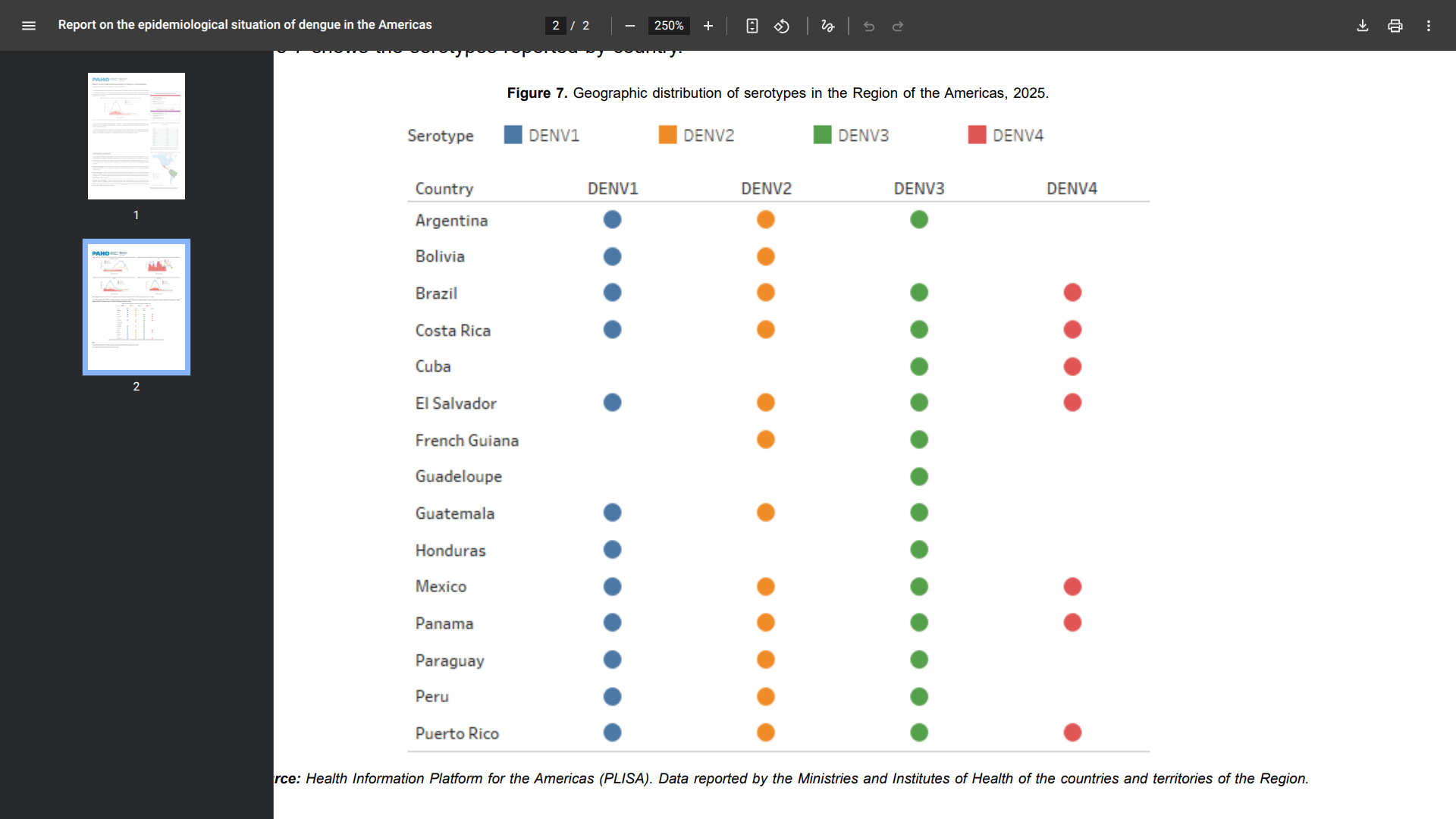
Specifically, during epidemiological week 39, 17 countries reported the circulation of dengue in the Region of the Americas: Brazil, Costa Rica, El Salvador, Mexico, and Panama. As of this week, the subregion exhibits a decrease of 77% compared to the same week in 2024
Several of these locations reported the the simultaneous circulation of DENV-1, DENV-2, DENV-3, and DENV-4 virus subtypes.
To Mexico's north, the Texas DSHS Arbovirus Activity Report Week #42 disclosed 45 dengue cases this year.
In 2024, Texas reported 143 dengue cases and one related fatality.
In Cameron County, one locally transmitted dengue case was confirmed.
Without access to dengue vaccines, Texas says, since Aedes mosquitoes usually bite people during the day, especially during early morning hours before daybreak and in the late afternoon before dark, when they are most active, use a mosquito repellent containing "DEET" on exposed skin to prevent infections.
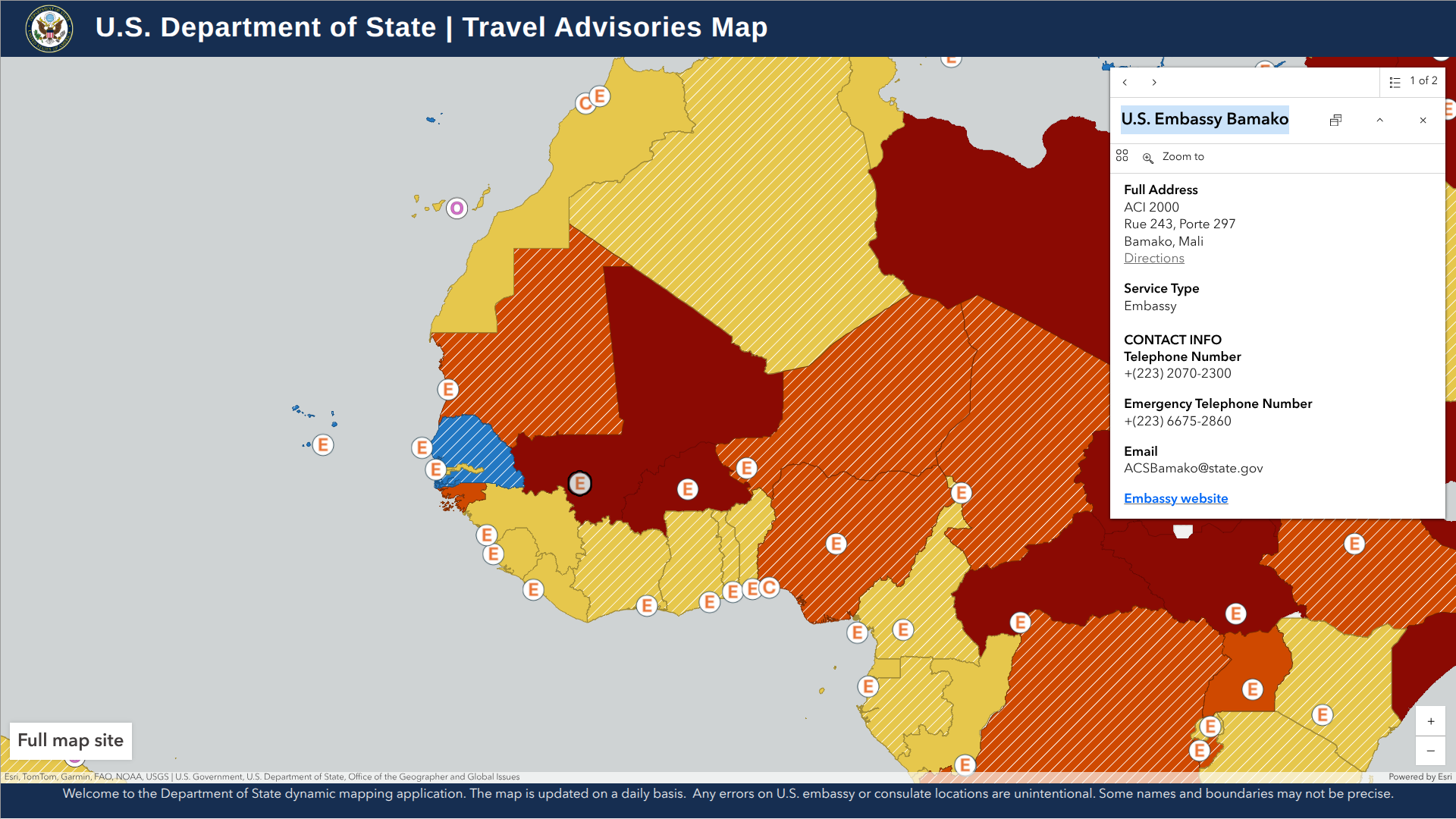
The travel advisory for the Republic of Mali, a landlocked country in West Africa, has been elevated to Level 4 status by the U.S. Department of State.
As of October 24, 2025, the State Department stated U.S. residents 'should not visit Mali for any reason.'
Furthermore, the U.S. government cannot provide routine or emergency services to U.S. citizens outside Bamako due to safety risks.
Have a plan to leave in an emergency that does not depend on U.S. government help, and enroll in the Smart Traveler Enrollment Program to receive digital alerts from the U.S. embassy. Enrolling helps the U.S. embassy contact you or your emergency contact in an emergency.
About 200,000 international travelers visit Mali annually.
From a health perspective, medical services for routine and emergency procedures are limited in Mali. Health facilities are available in major cities. It may be harder to find adequate health care in rural areas.
The U.S. CDC previously issued Level 1: Practice Usual Precautions for Mali regarding dengue and measles outbreaks. In addition to these diseases, the CDC recommends vaccination against yellow fever, typhoid, polio, and malaria medications when visiting Mali in 2025.
These vaccines and medications are offered at travel pharmacies.
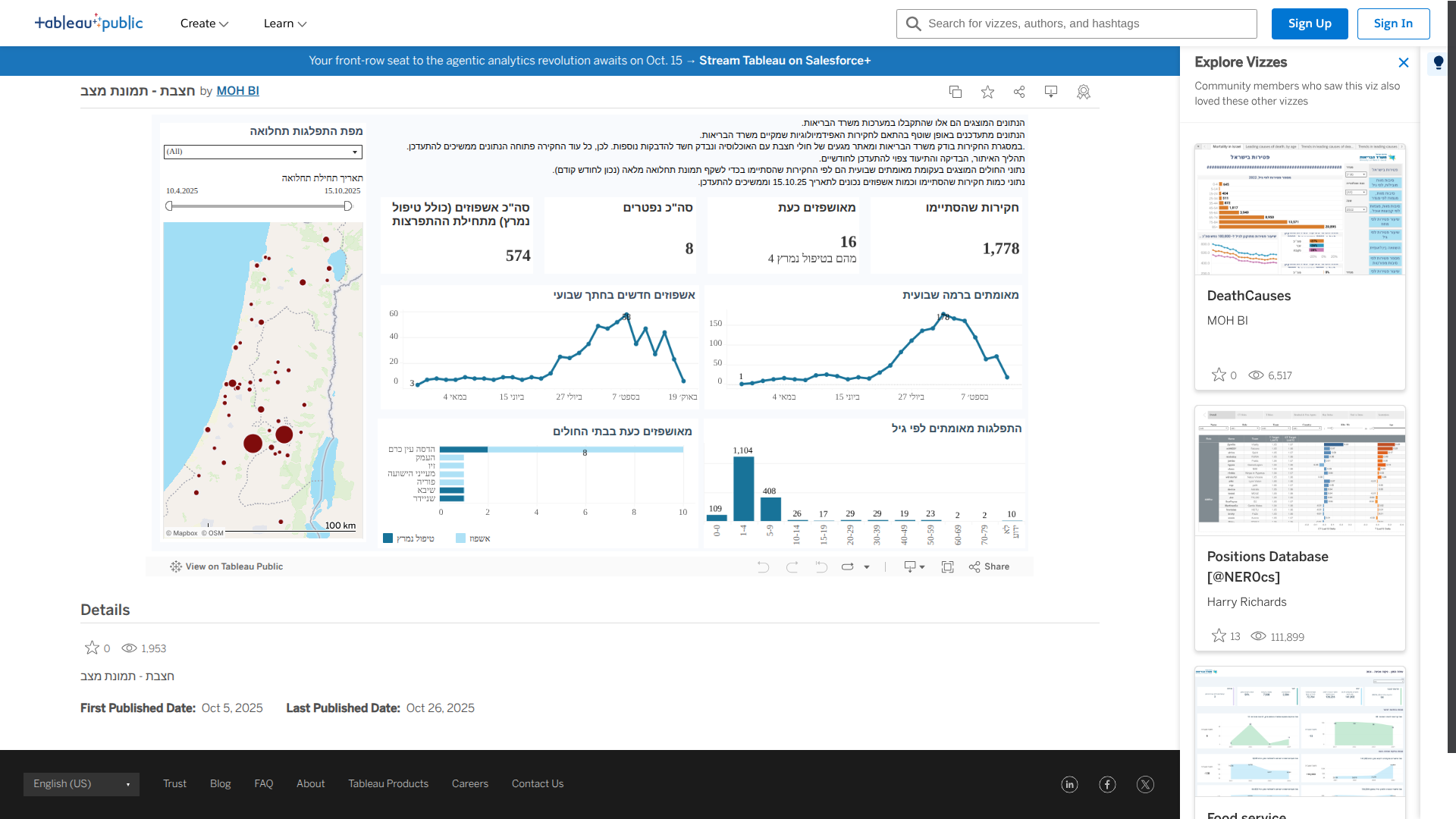
Israel's Health Ministry has reported the death of an unvaccinated toddler from a measles infection. The child died due to complications related to the virus.
As of October 26, 2025, this child marks the eighth death recorded since the measles outbreak began, with all cases involving infants who did not have any underlying medical conditions and were unvaccinated.
During 2025, there have been 1,778 measles cases and 574 hospitalizations.
The Ministry reported in a press release that the current measles outbreak areas include Jerusalem, Beit Shemesh, Bnei Brak, Harish, Modi'in Illit, Nazareth Illit, Kiryat Gat, Ashdod, Safed, Netivot, and the Mateh Binyamin Regional Council.
In these areas, people can visit family care centers and health maintenance organizations, and vaccinations are available without an appointment.
The Ministry advises unvaccinated individuals and parents of infants who have received one dose of the vaccine to avoid participating in large gatherings in outbreak areas due to the risk of infection.
As a result of the Ministry's efforts to increase vaccination coverage, vaccinations in Jerusalem have increased by 500% since September compared to the same period last year, and by 630% in Beit Shemesh.
In light of these figures, the first-dose vaccination coverage (for ages 1-6) against measles in Jerusalem rose from 77% to 84%, and in Beit Shemesh from 72% to 82.6%.
According to the U.S. CDC, international travelers planning to visit Israel in 2025 should be fully vaccinated against measles and polio.
In the USA, these vaccines are offered at travel clinics and pharmacies.
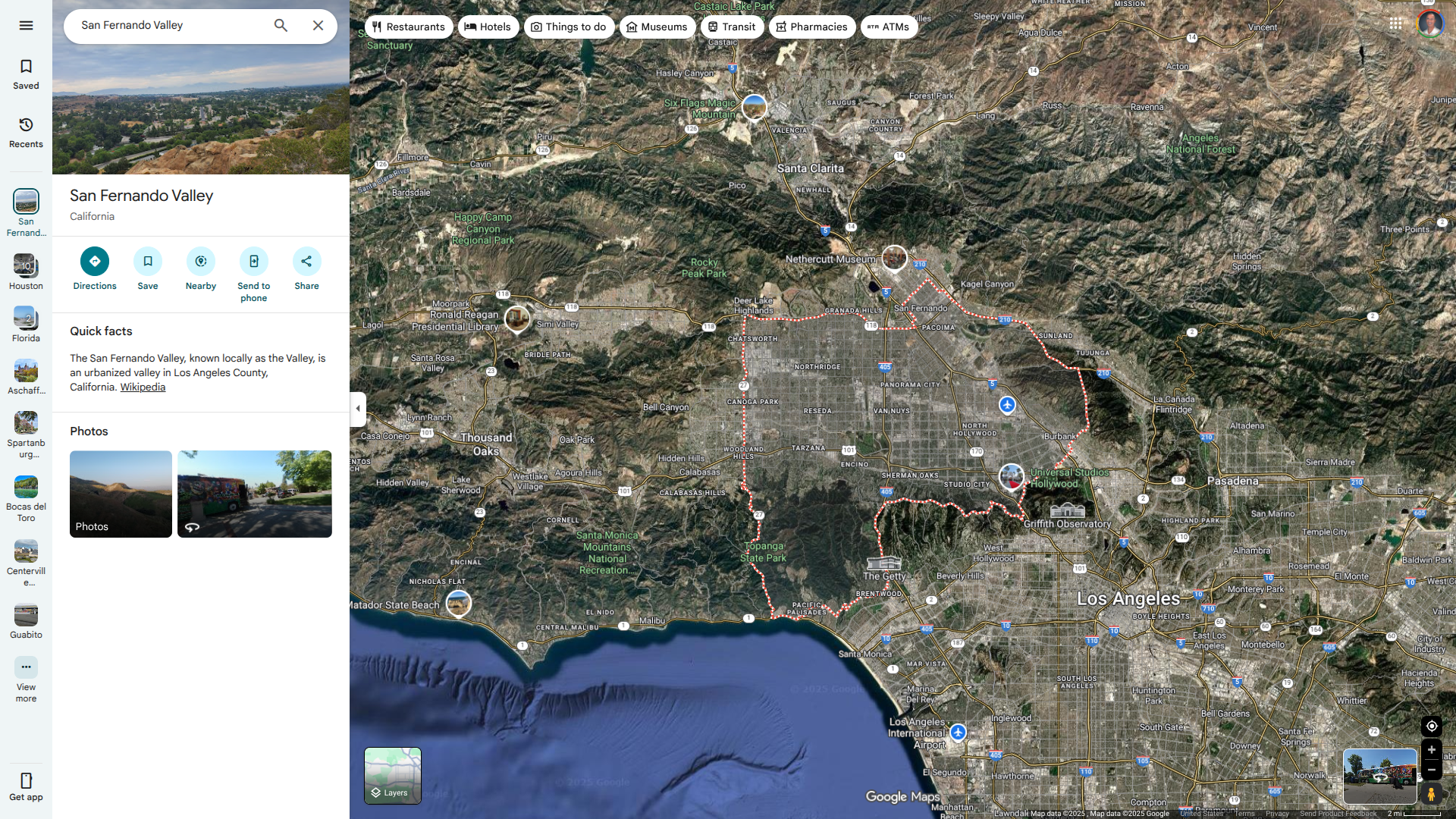
The Los Angeles County Department of Public Health (LACDPH) recently confirmed the first local death from the West Nile virus (WNV) in the 2025. The resident of the San Fernando Valley was hospitalized and died from a neurological illness caused by severe West Nile virus.
A total of 14 West Nile virus infections have been documented in Los Angeles County in 2025, excluding Long Beach and Pasadena. Half of the infected people live in the San Fernando Valley region.
Public Health reports West Nile virus cases every year, generally from June to November, as the virus is endemic in the region.
According to LACDPH, about 1 in 150 people will have severe WNV symptoms that may include high fever, stiff neck, muscle weakness, and sometimes rash. Symptoms usually appear 3 to 14 days after being infected.
West Nile virus is the most common mosquito-borne disease affecting residents of LA County, which has also reported locally acquired dengue cases in 2025.
"To the family and friends grieving the loss of a loved one due to West Nile virus, we extend our heartfelt condolences,” said Muntu Davis, MD, MPH, Los Angeles County Health Officer, in a press release on October 24, 2025.
“This tragic loss reminds us how dangerous mosquito-borne diseases like West Nile virus and dengue can be. Protect yourself and your neighbors by using insect repellent, getting rid of standing water where mosquitoes breed, and keeping window and door screens in good repair. Small actions like these can make a big difference in preventing illness.”
In collaboration with local vector control agencies, Public Health monitors the risk of WNV infection. It actively engages residents to provide information about reducing the risk by promoting protective measures against mosquitoes.
As of October 27, 2025, there is no WNV vaccine available in the USA.
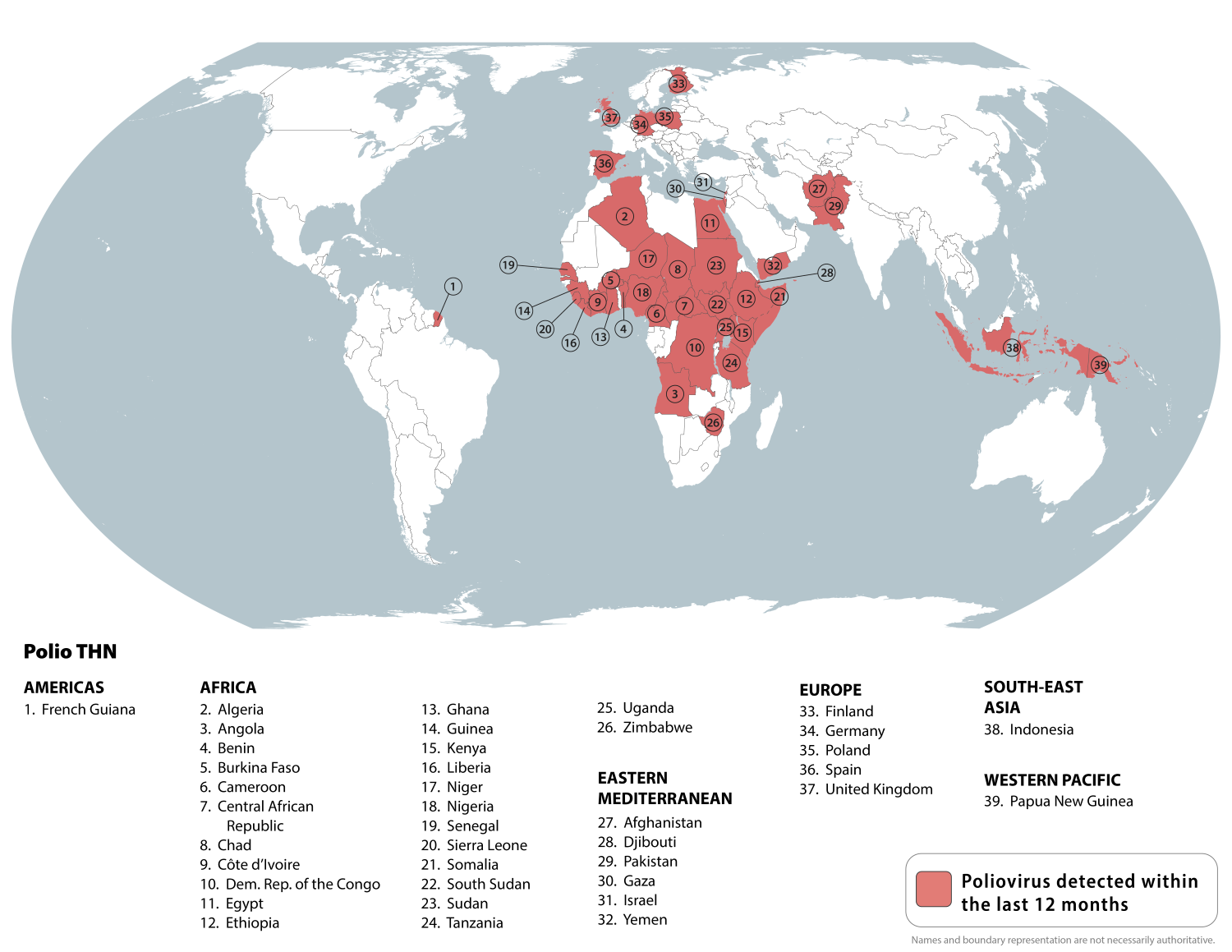
The World Health Organization (WHO) today announced that polio vaccine coverage in Europe is at its lowest level in several years, leaving more than 450,000 infants unprotected.
In 2024, polio vaccination rates in Europe decreased.
"Gaps in immunization coverage make children vulnerable and pose a health security risk to our region and beyond," stated Ihor Perehinets, MPH, the regional emergency director for WHO's European office, in a press release issued on October 24, 2025.
This WHO warning comes as new polio cases have been confirmed in Afghanistan and Papua New Guinea, according to the Global Polio Eradication Initiative.
In Afghanistan, two patients were infected with wild poliovirus type 1 (WPV1), with paralysis onset in early October, bringing the country's total WPV1 cases to nine for 2025.
Meanwhile, Papua New Guinea (PNG) reported two cases of circulating vaccine-derived poliovirus type 2 (cVDPV2) this week in Central and Enga provinces, with paralysis onset in August. So far this year, PNG has confirmed three cVDPV2 cases.
Furthermore, poliovirus type 2 has been detected through routine wastewater surveillance in 6 countries in the Region (Finland, Germany, Israel, Poland, Spain, and the United Kingdom) since September 2024.
WHO/Europe, together with other GPEI partners, continues to support national and local public health authorities in their investigations and monitoring of the situation, as well as in strengthening immunization programs and rapidly responding to detections of the virus to prevent it from spreading.
To alert international travelers to their polio risk in 2025, the U.S. CDC has issued a Travel Health Notice listing 39 countries. The CDC advises travelers to be fully vaccinated before visiting these areas.
Since the Zika virus was first detected in the Americas in 2015, the Pan American Health Organization (PAHO) and the World Health Organization (WHO) have reported cases from 52 countries and territories in the region.
As of October 24, 2025, the PAHO Zika data dashboard indicates that there have been over 23,000 cases and four related fatalities in the Region of the Americas this year.
The current leaders are Brazil (21,762), Bolivia (1,012), and Argentina (849).
And in the Central America Region, Costa Rica, El Salvador, and Guatemala are the unfortunate leaders in reporting this mosquito-transmitted disease.
This PAHO data aligns with 2024, when 44,480 cases and two related fatalities were confirmed across all countries for the entire year.
Last year, Brazil reported about 90% of all cases.
In the Americas, one in four Zika-infected people may develop symptoms, but in those who are affected, the disease is usually mild, with symptoms lasting between 2 and 7 days. The clinical appearance is often similar to dengue or chikungunya.
According to the PAHO, Zika virus infection during pregnancy poses severe risks to the fetus, ranging from congenital Zika syndrome to microcephaly to milder neurodevelopmental issues.
From a severity perspective, there is scientific consensus that Zika is a cause of Guillain-Barré syndrome.
As of October 2025, the UK travel advisory says that since there is no vaccination or medication to prevent Zika infection, women should avoid becoming pregnant while traveling to at-risk countries such as those listed above, and for 2 months after their last possible Zika virus exposure.
Prevention involves reducing mosquito populations and avoiding bites, which occur mainly during the day, says the UK advisory.
In the future, a Zika vaccine candidate may be approved for human use.