Search API
Strong support from the Indian government to eradicate polio in the late 1980s. In the years leading up to the last wild polio outbreak, nearly one billion vaccines were distributed to millions of children annually.
Those efforts led the World Health Organization to declare India polio-free in 2014
To maintain that status, polio vaccination campaigns continue across India. On December 8, 2024, local media reported that Rajasthan aims to distribute polio vaccines to over 87 lakh children.
Unfortunately, on December 3, 2024, the WHO announced that the risk of the international spread of poliovirus remains a Public Health Emergency of International Concern and recommended extending Temporary Recommendations for another three months.
This WHO notice does not impact India's polio-free classification.
While the U.S. CDC includes India in its Travel Health Advisories for chikungunya, dengue, and zika diseases, no polio vaccination requirement is mentioned for international visitors. The CDC has identified 37 countries with polio vaccination recommendations in its Level 2 Advisory issued in August 2024.
The World Health Organization (WHO) today announced that between 24 October and 5 December 2024, the Panzi health zone in Kwango Province of the Democratic Republic of the Congo (DRC) recorded 406 cases of an undiagnosed disease with symptoms of fever, headache, cough, runny nose, and body ache.
Most cases reported are among children, particularly those under five years of age.
The WHO's Disease Outbreak News wrote on December 8, 2024, that 31 deaths had been registered.
Given the clinical presentation and symptoms reported so far and the number of associated deaths, acute pneumonia, influenza, COVID-19, measles, and malaria are considered potential causal factors, with malnutrition as a contributing factor.
Laboratory tests are underway to determine the exact cause. At this stage, it is also possible that more than one disease is contributing to the cases and deaths.
The WHO says the overall risk level to the affected DRC communities is assessed as high.
At the national level, the risk is considered moderate due to the localized nature of the outbreak within the Panzi health zone in Kwango province. However, the potential for spread to neighboring areas, coupled with gaps in surveillance and response systems, this assessment underscores the need for heightened preparedness.
At the regional and global levels, the risk remains low at this time.
However, the proximity of the affected area to the border with Angola raises concerns about potential cross-border transmission, and continued monitoring and cross-border coordination will be essential to mitigate this risk.
The current confidence in the available information remains moderate, as significant clinical, epidemiological, and laboratory data gaps persist.
One aspect of this new WHO report is that there are vaccines available for many of these suspected diseases.

The Florida Department of Health recently published its Arbovirus Surveillance Update 48, which discloses mosquito-borne disease activity, such as Dengue virus.
As of December 7, 2024, 70 cases of locally acquired dengue were reported from ten counties led by Miami-Dade (44). Most of this year's dengue cases are serotyped as DENV-3 and 4.
In 2023, 186 people contracted dengue in Florida.
This virus is transmitted to people by infected mosquitoes. Furthermore, women infected with dengue during pregnancy can pass the virus to their fetus.
As of today, the U.S. Centers for Disease Control and Prevention, Canada Health, and the United Kingdom have not issued vaccination requirements for visitors traveling to southeast Florida.
Dengue vaccines are available in numerous countries but not in the U.S.

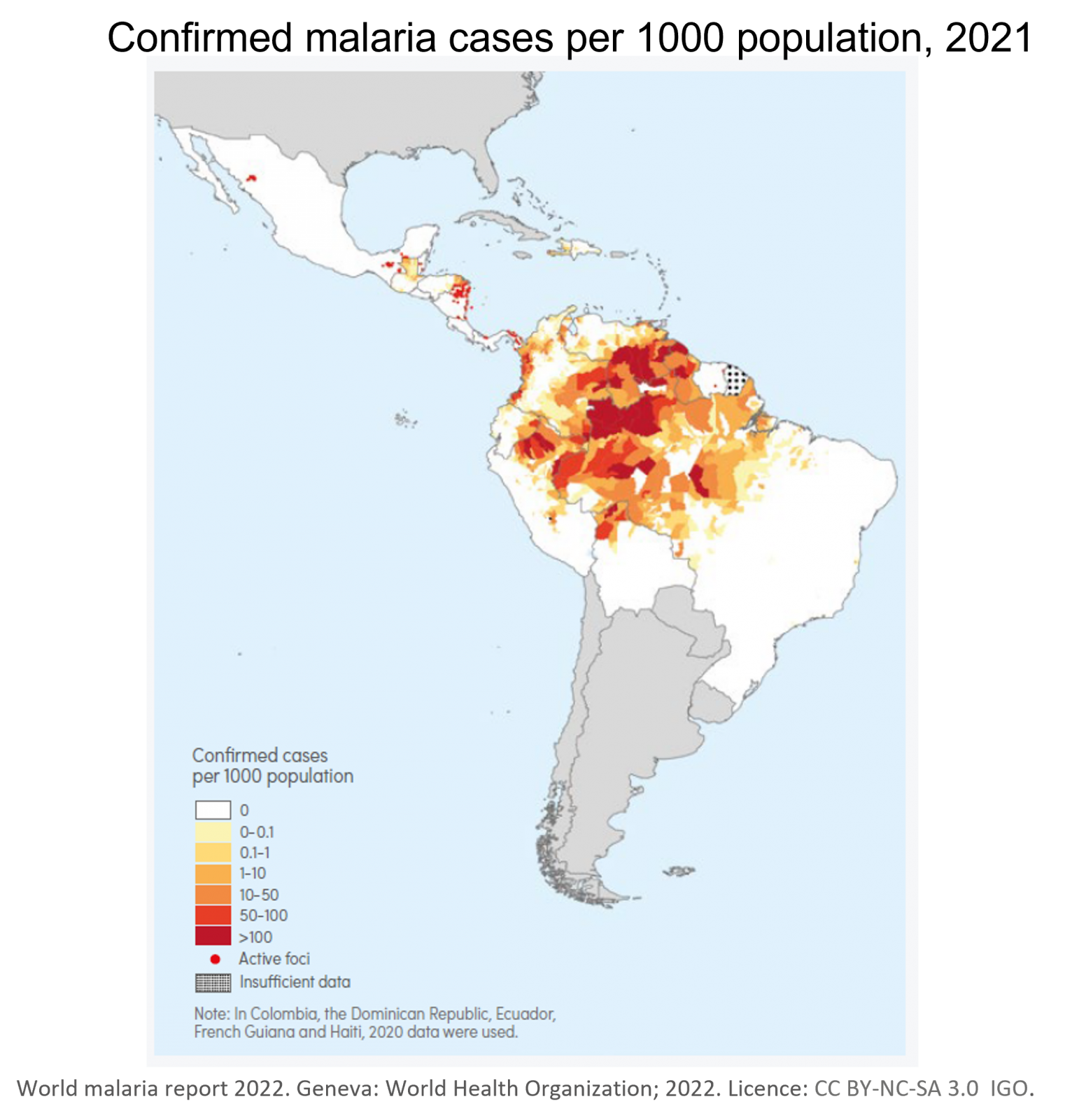
In the Region of the Americas, outbreaks of Oropouche virus disease have occurred historically in the Amazon region in rural and urban communities in Brazil, Colombia, Ciba, Ecuador, French Guiana, Panama, Peru, and Trinidad and Tobago.
On December 5, 2024, the World Health Organization (WHO) issued Disease Outbreak News regarding the current outbreak.
As of late November 2024, a total of 11,634 confirmed Oropouche cases, including two deaths, have been reported in the Region of the Americas across ten countries and one territory: Bolivia, Brazil, Canada, Cayman Islands, Colombia, Cuba, Ecuador, Guyana, Panama, Peru and the United States of America.
In the USA, the Florida Department of Health published its Arbovirus Surveillance Update 48 on November 30, 2024, revealing 90 travel-associated Oropouche fever cases have been reported this year in travelers to Cuba.
The WHO's News report highlights the need to strengthen epidemiological and entomological surveillance and reinforce the population's preventive measures.
This advice is crucial due to the expansion of the virus's transmission area and the growing need to understand better the disease spectrum, including possible new transmission routes. Oropouche is spread primarily by the bite of infected midges (small flies) and mosquitoes.
While it is unknown if Oropouche can be spread by sex, travelers to outbreak areas should take precautions during travel and for six weeks after returning to the USA from abroad.
According to the U.S. CDC, these vectors could affect the general population and vulnerable groups, such as pregnant women, their fetuses, and newborns.
Unfortunately, there are no Oropouche preventive vaccines available in 2024.
Based on available information, the WHO assesses the overall public health risk posed by the Oropouche virus as high at the regional level and low at the global level. Based on the current information on this event, WHO advises against applying travel or trade restrictions.

In Europe, dengue viruses, transmitted by Aedes albopictus mosquitoes, are primarily associated with infections acquired in endemic countries.
However, autochthonous (locally acquired) dengue cases have surged in the past five years, with significant reports from Spain, Croatia, France, and Italy. In 2023, Italy reported its highest-ever number of locally transmitted dengue virus cases.
The year 2023 was exceptional, not just due to the total number of reported cases but also for the uncommon co-occurrence of a few spatially disjointed autochthonous transmission chains of more than one DENV serotype, wrote researchers in an article published by the journal Nature on December 5, 2024.
The Italian National Public Health Authority reported 213 locally acquired dengue cases in 2024, a significant increase from the 82 confirmed cases last year.
Specifically, Italy's dengue outbreaks have become regionalized as infected mosquitoes spread the virus.
As of October 28, 2024, Eurosureliiance reported 138 confirmed and 61 probable cases of DENV-2 in Fano, a small coastal city in Italy's Marche Region.
With the holiday travel season fast approaching, Italy is anticipating additional dengue cases to be confirmed in 2024.

The U.S. CDC today published a Morbidity and Mortality Weekly Report that confirmed Nirsevimab (Beyfortus™), a U.S. FDA-approved monoclonal antibody that protects infants and young children against severe respiratory syncytial virus (RSV) infection, experienced significant uptake in New York City (NYC).
Among infants born in NYC during the recommended nirsevimab administration period for the 2023–24 RSV season and who reportedly received nirsevimab, 37% of Vaccines for Children (VFC)–eligible and 45% of non–VFC–eligible infants received it within the first 7 days of life.
These authors wrote on December 5, 2024, 'Ensuring birthing hospital VFC enrollment and establishing protocols to offer nirsevimab to eligible infants before hospital discharge might increase nirsevimab administration within the first week of life.'
Furthermore, Beyfortus has been found to be very protective.
On November 26, 2024, a study published by The Pediatric Infectious Disease Journal concluded that in immunized infants, RSV-positive bronchiolitis was less frequent and less severe, with a significantly reduced hospitalization length than in nonimmunized infants, producing substantial healthcare cost savings.

The World Health Organization (WHO) today announced that it is deploying experts to support health authorities in the Democratic Republic of the Congo (DRC) in carrying out further investigations to determine the cause of an undiagnosed disease that has been reported in Panzi, a locality in Kwango province.
So far, the disease has been reported in seven of the 30 health zones in Kwango province.
According to the Ministry of Public Health, 394 cases and 30 deaths have been reported so far in the Panzi health zone. Symptoms of the illness include headache, cough, fever, breathing difficulties, and anemia. Until laboratory test results are received, the cause is unclear.
As of December 6, 2024, laboratory tests are being conducted to determine the cause of this respiratory pathogen. Diseases such as Influenza, COVID-19, malaria, measles and others. Some officials have called this unknown outbreak a Disease X situation.
Disease X was included for the first time in February 2018 by the WHO Blueprint for Epidemics, representing the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease.
"Our priority is to support the affected families and communities effectively. All efforts are underway to identify the cause of the illness, understand its modes of transmission, and ensure appropriate response as swiftly as possible," said Dr. Matshidiso Moeti, WHO Regional Director for Africa, in a media release.
Panzi is a rural community over 700 km from the DRC's Kinshasa. With over 17 million residents, it is an international gateway to numerous destinations.
As of today, the WHO has not called for travel restrictions.
The World Health Organization (WHO) today announced it has granted prequalification to the molecular diagnostic test for tuberculosis (TB) called Xpert® MTB/RIF Ultra.
As of December 5, 2024, this is the first test for TB diagnosis and antibiotic susceptibility testing that meets WHO's prequalification standards.
This nucleic acid amplification test (NAAT) Xpert® MTB/RIF Ultra detects the genetic material of Mycobacterium tuberculosis, the bacterium that causes TB, in sputum samples and provides accurate results within hours.
Simultaneously, the test identifies mutations associated with rifampicin resistance, a key indicator of multidrug-resistant TB.
"This first prequalification of a diagnostic test for tuberculosis marks a critical milestone in WHO's efforts to support countries in scaling up and accelerating access to high-quality TB assays that meet both WHO recommendations and its stringent quality, safety, and performance standards," said Dr. Yukiko Nakatani, WHO Assistant Director-General for Access to Medicines and Health Products, in a press release.
"It underscores the importance of such groundbreaking diagnostic tools in addressing one of the world's deadliest infectious diseases."
Tuberculosis outbreaks are one of the world's leading infectious disease killers, causing over a million deaths annually and imposing immense socioeconomic burdens, especially in low- and middle-income countries. Accurate and early detection of TB, especially drug-resistant strains, remains a critical and challenging global health priority.
In the United States, TB cases have been increasing over the past few years.
Additionally, TB is a vaccine-preventable disease, with over 10 BCG vaccines available worldwide.

As the holiday season 2024 approaches, the UK Health Security Agency (UKHSA) reminds international travelers heading abroad to take precautions against mosquito-transmitted diseases, such as malaria.
Malaria is typically transmitted in tropical and subtropical areas, where anopheles mosquitoes can survive.
UKHSA provisional data as of December 2024 indicate that 753 travel-acquired malaria cases were reported in the UK between January and June 2024. The majority of these patients were located in the London area.
The annual malaria report for 2023 shows that 2,106 cases of imported malaria were reported in the UK. This is 26% higher than the cases reported in 2022 and the highest total number of cases seen in the UK since 2001.
Malaria is a potentially fatal disease that is almost entirely preventable when malaria prevention tablets are taken appropriately.
Dr. Dipti Patel, Director of the National Travel Health Network and Centre commented in a media release, "People traveling abroad during the Christmas break should plan to ensure they have a safe and healthy trip... and consult a GP, pharmacy, or travel health clinic at least 4 to 6 weeks before the trip."
"This is to ensure that your vaccinations are current and that you receive any necessary health advice."
Furthermore, two malaria vaccines are now being deployed in Africa, where 90% of infections are reported.