Search API
The Democratic Socialist Republic of Sri Lanka's Ministry of Health recently highlighted a noticeable increase in the Chikungunya outbreak in the Colombo and Kotte areas.
As of March 14, 2025, Weekly Epidemiological Report #12 revealed 173 chikungunya cases had been reported in Colombo, Gampaha, and Kandy.
Local media reported that Acting Consultant Community Physician Dr. Kumudu Weerakoon stated that the Chikungunya virus spread to Sri Lanka in 1960. After several years of low transmission, medical experts said in May 2025 that an effective way to control the spread of Chikungunya is to eliminate as many mosquito breeding sites as possible.
While Sri Lanka is an island country in South Asia in the Indian Ocean, it is located thousands of miles to the east of the Chikungunya outbreaks in Mayotte, Mauritius, and Réunion.
International travelers departing from the United States and Europe can receive a preventive vaccine when visiting these Chikungunya outbreak areas in May 2025.
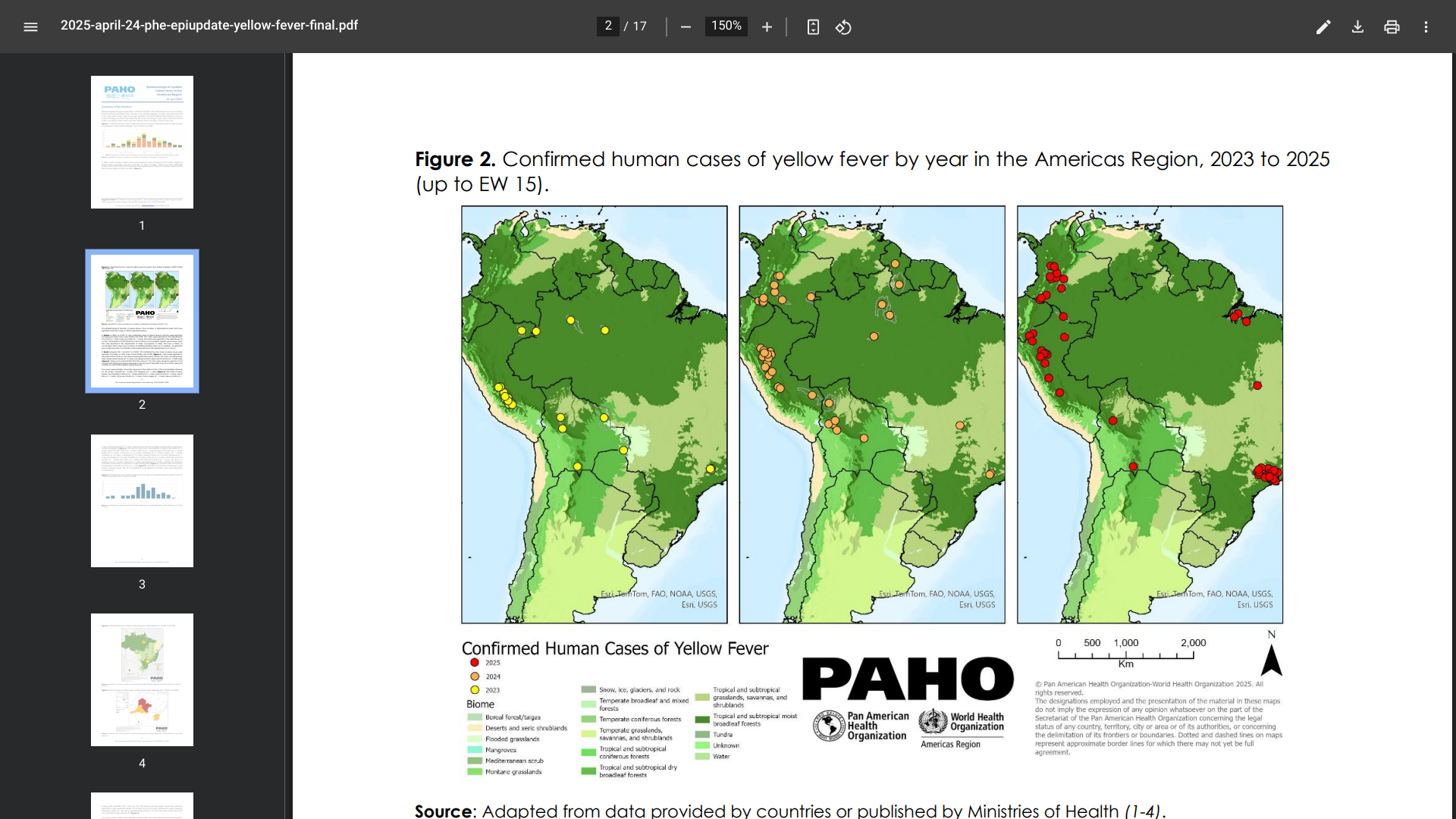
Researchers believe the yellow fever virus has existed for thousands of years, originating in Africa and spreading to the Region of the Americas in the 17th century.
As of May 14, 2025, the Pan American Health Organization (PAHO) says yellow fever has become endemic in 13 countries in the Americas.
The PAHO reported 189 confirmed human cases of yellow fever (YF) in four countries in the Americas Region, of which 74 have been fatal.
The breakdown of reported YF cases is as follows: The Plurinational State of Bolivia, with two cases, including one fatal case; Brazil with 102 cases, including 41 fatal cases; Colombia with 53 cases, including 21 fatal cases; and Peru with 32 cases, including 11 fatal cases.
In 2025, YF cases were detected mainly in the state of São Paulo in Brazil and the department of Tolima in Colombia, areas outside the Amazon region of both countries.
The PAHO/WHO encourages Member States to continue surveillance and vaccination efforts in YF-endemic areas.
'It is essential that countries achieve vaccination coverage of at least 95% in populations in at-risk areas,' writes the PAHO.
And that health authorities ensure that they have a strategic reserve inventory that allows them to maintain routine YF vaccination and, at the same time, respond effectively to possible outbreaks.
In the United States, YF vaccination appointments are offered at travel clinics and pharmacies in 2025.
In 2025, the State Institute of Public Health (SZÚ) reported a rise in cases of infectious jaundice across the Czech Republic (Czechia). By the end of April, 450 reported cases of viral hepatitis A had been reported.
Tragically, six patients had died due to hepatitis A, a vaccine-preventable disease.
Czech health officials informed the media on May 13, 2025, that the actual number of infections is likely much higher because it is difficult to track the spread of the virus, which causes liver inflammation that can be fatal in rare cases.
In comparison, the SZÚ recorded 636 cases and two related deaths in 2024.
This year, Hepatitis A affects regions across the Czech Republic. The regions of Central Bohemia – 87, Moravia-Silesia – 83, and Prague – 73 report the most cases.
"In Prague, almost 1/3 of the disease is reported in homeless people," stated SZU.
In 2025, the spread of hepatitis A impacted other European countries, such as Slovakia, Hungary, Ireland, and the United Kingdom.
Effective Hepatitis A vaccines are available in the Czech Republic, as in the United States.
Basic protection is achieved after a single injection. A second dose is required to obtain long-term protection, which is given 6-18 months after the first dose.

When the U.S. CDC issued a global Travel Health Advisory for 57 countries reporting measles outbreaks in March 2025, it should have included the Kingdom of Morocco, where measles has become endemic.
According to the World Health Organization (WHO) DON568, more than 25,000 suspected measles cases were reported from all 12 regions in this northwest African country from October 2023 through April 13, 2025, and 184 related fatalities.
The first cases were reported in the Souss Massa region in central Morocco, before spreading to additional provinces.
Recently, the WHO reported a declining trend in cases observed for ten consecutive weeks in 2025.
As of May 13, 2025, genomic characterization of measles virus specimens collected during Morocco's 2024–2025 outbreak revealed the exclusive circulation of genotype B3, which is common in many parts of Africa and associated with outbreaks globally.
The measles vaccine was introduced into Morocco's national immunization schedule in 2003. According to WHO/UNICEF Estimates of National Immunization Coverage, Morocco has been below the 95% threshold required to achieve the elimination goal for the last three years.
The WHO reports that the overall risk is assessed as moderate at the national and regional levels, particularly given the risk of cross-border transmission in areas with low vaccination coverage.
The CDC does recommend that international travelers be protected against this highly transmissible virus before visiting at-risk areas in May 2025.

In 1904, the Isthmus of Panama reported that tropical diseases such as malaria led to the death of an estimated 12,000 workers during the Panama Canal project.
Over 100 years later, the mosquito-transmitted malaria continues to impact the health of the Republic of Panama.
On May 9, 2025, Panama's Ministry of Health (Minsa) reported that two deaths from malaria had been recorded in 2025. The victims were from Eastern Panama in February and from Veraguas in March.
These are Panama's first malaria-related fatalities since 2017.
In 2024, a total of 15,109 cases were reported, and in 2023, 11,659 malaria cases were reported. This data represents a sustained increase in the transmission of this disease.
Minsa stated that this increase has been linked to increased human mobility toward areas of active transmission and the effects of climate variability and change, which can favor the proliferation of the transmitting mosquito and contact with vulnerable populations. It urges citizens to collaborate actively with prevention strategies and seek prompt medical attention if they experience symptoms consistent with malaria.
Throughout 2025, several countries in the Region of the Americas have reported malaria outbreaks.
As of May 13, 2025, the U.S. CDC Yellow Book recommends that travelers to certain areas of Panama take prescription medicine to prevent malaria. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to a travel medicine professional about which malaria medication you should take.
Furthermore, while two malaria vaccines are being deployed in Africa, they have not been offered in the Americas.
Additionally, the CDC has included Panama in its Travel Health Advisories for Dengue and Oropouche outbreaks.
Since August 2024, widespread outbreaks of the chikungunya virus disease have been reported in the western Indian Ocean.
As of May 12, 2025, France's Departments of La Réunion and Mayotte have been significantly impacted.
The World Health Organization (WHO) Disease Outbreak News (567) today wrote, 'Although chikungunya outbreaks and endemic transmission occur annually in several countries and territories around the world, the Indian Ocean islands have not experienced major outbreaks for nearly two decades.'
In La Réunion, over 47,500 cases and twelve associated deaths have been reported as of May 4, 2025, with sustained high transmission across the island.
In Mayotte, the first locally transmitted cases since 2005–2006 have been detected, raising concern about similar large outbreaks. As of early May 2025, about 90 cases had been confirmed.
France's public health response measures, including enhanced surveillance, vector control activities, and novel targeted vaccination efforts, have been implemented to contain the outbreaks.
However, further outbreak activity in the islands of the Indian Ocean can be expected, says the WHO.
Seperately, the U.S. CDC issued a Level 2 - Practice Enhanced Precautions travel advisory that says, 'If you are pregnant, reconsider travel to the affected areas, particularly if you are close to delivering your baby. Mothers infected around the time of delivery can pass the virus to their baby before or during delivery.'
According to the CDC, vaccination is recommended for travelers visiting an area with a chikungunya outbreak, such as these French departments in the Indian Ocean.
Chikungunya vaccines are approved for use in the United States and are commercially available at travel clinics and pharmacies.

North Dakota Health and Human Services (HHS) reports two additional measles cases in Cass County, bringing the state’s total to 11 cases in 2025. Both individuals were unvaccinated and acquired measles through international travel.
HHS stated on May 11, 2025, that exposed vaccinated individuals don’t need to be quarantined.
However, individuals who have not received a dose of the measles, mumps, and rubella (MMR) vaccine should be quarantined (stay home) and monitored for symptoms for 21 days.
These are not related to recent cases in Williams County.
"Due to the current measles outbreak, please isolate at home if you have symptoms of runny nose, fever, cough, and rash,” said Dr. Beverly Tong, Upper Missouri District Health Unit deputy director, in a press release on May 6, 2025.
“Isolation should continue until at least four full days after the onset of a rash."
"Time from exposure to onset of rash is generally around seven to 21 days, and you can spread measles up to four days before the rash appears. Don't hesitate to contact your health care provider's office if you wish to be tested. They will instruct you on when and where to arrive at their clinic to minimize risk to others."
Because some new measles cases are not linked to earlier known exposures, there is concern about potential community transmission. As a precaution, HHS recommends that all residents and travelers to Williams County ensure they are vaccinated against measles. This includes considering early MMR vaccination for infants aged 6 through 11 months.
Few disease outbreaks have been as deeply traumatic as the 2014 Ebola outbreak in West Africa. By the time the outbreak stopped in 2016, nearly 30,000 had been infected, and 11,000 people had died.
With no vaccine available at the outbreak's start, the affected countries, Guinea, Sierra Leone, and Liberia, were unprepared to respond.
This unfortunate situation has changed with the approval of Ebola vaccines and therapeutics.
Launched in January 2021, the International Coordinating Group on Vaccine Provision, which includes the World Health Organization, UNICEF, and others, now coordinates a stockpile.
It is a Gavi-funded, globally managed reserve of Merck's ERVEBO® (rVSV-ZEBOV) vaccine that ensures rapid, equitable access to life-saving immunisation during outbreaks.
The vaccine stockpile in Switzerland is maintained at a target level of 500,000 ERVEBO doses, as the WHO’s Strategic Advisory Group of Experts on Immunization recommends.
A challenge in maintaining a stockpile is ensuring that doses are always available and do not expire.
“All Ebola outbreaks that have occurred since we had a stockpile were quickly stopped – thanks to the vaccines and rapid other response measures,” said Allyson Russell, an epidemiologist and senior programme manager in Gavi’s High Impact Outbreaks team, in a April 30, 2025 news release.
In the United States, ERVEBO® is approved by the Food and Drug Administration for preventing disease caused by the Zaire Ebola virus in individuals 12 months of age and older as a single-dose administration.
Zaire Ebola vaccines aren't effective against the other three orthoebolaviruses that cause severe disease, including the Sudan virus.
Since there are no well-controlled studies of ERVEBO in pregnancy, the U.S. CDC says, 'The risk of exposure to Ebola should be weighed against potential vaccine-related risk during pregnancy based on individual informed decisions.'
As of May 12, 2025, access to Ebola vaccines in the U.S. is restricted.