Ebola Vaccines 2025
Since 2014, Ebolavirus vaccine technologies have included replication-deficient adenovirus vectors, replication-competent vesicular stomatitis virus, human parainfluenza virus vectors, and virus-like nanoparticle preparations. The U.S. Biomedical Advanced Research and Development Authority (BARDA) has funded and is developing vaccine candidates against the six filoviruses. The World Health Organization (WHO) has approved Ebola vaccines to protect people against outbreaks of Zaire Ebolavirus since 2019.
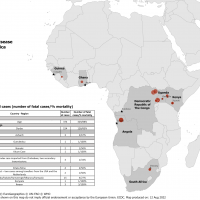
As of March 2025, Sudan Ebolavirus vaccine candidates are in development. In 2024, ring vaccinations were introduced as an additional control measure for Ebola outbreaks. In 2021, the International Coordinating Group (ICG) on Vaccine Provision established a global Ebola vaccine stockpile.
Zaire Ebolavirus Vaccines
Zaire Ebolavirus vaccines have been approved by the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), the World Health Organization (WHO), and the United Kingdom. As of October 2024, the U.S. Centers for Disease Control and Prevention (CDC) recommends two licensed vaccines for the prevention of Ebola caused by Orthoebolavirus zairense: the rVSVΔG-ZEBOV-GP (ERVEBO) and the Ad26.ZEBOV and MVA-BN-Filo.
Merck's Ervebo® vaccine. Since its approval, 7,370 doses of the Ervebo vaccine have been administered in response to two EVD outbreaks in Africa. About 500,000 doses are stored in Switzerland.
Johnson & Johnson Zabdeno and Mvabea (Ad26.ZEBOV, MVA-BN-Filo) Ebola vaccine regimen.
CanSinoBio's Ad5-EBOV vaccine.
U.S. NIAID/Nin collaborated to develop the 3-EBOV/MVA-BN-Filo vaccine.
MVA-BN (Mvabea®) was approved by the EMA in 2020 as part of a prime-boost vaccine regimen for the prevention of Ebola virus disease caused by the Zaire Ebolavirus in individuals aged 1 year and older.
Zaire Ebolavirus Vaccine Boosters
A study published by the journal Nature on September 3, 2024, guides booster vaccination recommendations and helps identify populations likely to benefit from Ebola revaccination.
Zaire Ebolavirus Vaccine Candidates
INOVIO's INO-4201 is a DNA vaccine candidate targeting the glycoprotein of the Zaire Ebola virus. It is designed to prevent ZEBOV infection. The candidate was evaluated in a Phase 1b clinical trial. INO-4201 was well-tolerated and boosted humoral responses in 100% (36 of 36) of treated participants. As of August 8, 2024, INOVIO anticipates submitting its revised protocol to the FDA for a Phase 2/3 clinical trial with INO-901 as a heterologous booster for the vaccine.
S.K. Biosciences entered into a development licensing agreement with Hilleman Laboratories in November 2023 the jointly develop a second-generation Zaire Ebola virus vaccine. "We look forward to working closely with MSD to accelerate broad access to the second-generation Zaire ebolavirus vaccine and help to improve vaccine coverage for populations in LMICs," said Dr. Raman Rao, CEO of Hilleman Laboratories.
The bivalent adenovirus vectored vaccine is conducting a phase 1 study (NCT05301504). The Sabin Vaccine Institute USA produces the ChAd3-SUDV monovalent adenovirus vector vaccine.
YF-EBO is a live YF17D-vectored dual-target vaccine candidate expressing EBOV glycoprotein (G.P.) as a protective antigen. A single dose of YF-EBO was sufficient to induce high levels of EBOV GP-specific antibodies and cellular immune responses that protected against lethal infection using EBOV GP-pseudotyped recombinant vesicular stomatitis virus (rVSV-EBOV) in interferon-deficient (Ifnar-/-) mice as a surrogate challenge model. Concomitantly induced yellow fever virus (YFV)-specific immunity protected Ifnar-/- mice against intracranial YFV challenge.
INOVIO announced on April 12, 2023, that an abstract had bee-4201 as an, la booster for rVSV-ZEBOV (Ervebo) at the, had been accepted for presentation at the 33rd European Congress of Clinical Microbiology and Infectious Diseases.
Sudan Ebolavirus Vaccine Candidates
As of April 26, 2025, no vaccines have been approved to protect people against the Sudan Ebola virus (SUDV). However, the WHO confirmed that candidate vaccines are being tested in the Solidarity Against Ebola human clinical studies, and the Vaccine Institute is developing a single-dose vaccine candidate for Sudan Ebolavirus. Based on the same cAd3 platform as its Marburg vaccine candidate, Sabin's Sudan ebolavirus vaccine was found to be promising in Phase 1 clinical and non-clinical studies. Results showed it to be safe while eliciting rapid and robust immune responses that lasted up to 12 months.
IAVI's rVSV Sudan ebolavirus vaccine candidate (IAVI C108, rVSVΔG-SUDV-GP) was confirmed on June 27, 2023. The first participants were vaccinated with an SUDV candidate in a first-in-human Phase I clinical trial in the U.S. In January 2025, about 2,160 doses of the vaccine candidate were being deployed in Kampala, Uganda.
Previously, BARDA issued financial awards to IAVI to support the development of rt IAVI's SUDV vaccine candidate.
Serum Institute of India's experimental Ebola virus vaccine.
GeoVax Labs, Inc.'s vectored vaccine, MVA-VL, P-SUDV, was genetically engineered to target Sudan Ebolavirus. Data published on July 25, 2022, demonstrates the MVA-VLP platform's single-dose protection and potency for use in emergencies to contain outbreaks.
Soligenix, Inc. proposes developing SuVax™, a single-vial, adjuvanted, heat-stable subunit vaccine to prevent filovirus infection for use in the event of a Sudan ebolavirus outbreak. On September 25, 2023, the thermostabilized bivalent and trivalent filovirus vaccine candidates demonstrated two-year stability at 40°C when formulated in a single vial, requiring reconstitution only with sterile water immediately before use. The filovirus vaccines represent the only recombinant subunit vaccines to date that have demonstrated complete protection against challenges with Zaire ebolavirus, Sudan ebolavirus, and Marburg marburgvirus in NHPs.
The U.S. government initially invested $35 million to produce up to 100,000 doses of ChAd3-SUDV. These vaccines may be part of ongoing U.S. preparedness efforts and response to future global outbreaks.
The National Institutes of Health Rocky Mountain Laboratories in Hamilton, Montana, developed a candidate for a vesicular stomatitis virus-based Sudan virus vaccine (VSV-SUDte). The investigators anticipate that administering VSV-SUDV at a dosage similar to that of VSV-EBOV would provide rapid protective immunity against SUDV.
VRC-EBOADC086-00-VP, a chimpanzee adenovirus serotype three vector-based Ebola vaccine, encodes wild-type glycoprotein from the Sudan strain of Ebolavirus and is administered intramuscularly. A Phase I Open-Label, Dose-Escalation Clinical Trial to Evaluate Two Doses of Safety, Tolerability, and Immunogenicity. In August 2023, a study found the cAd3-EBO S vaccine was safe at both doses, rapidly induced responses in most participants after a single injection, and was well tolerated. The rapid onset and durability of the vaccine-induced antibodies make this vaccine a strong candidate for emergency deployment in SDV outbreaks.
Ebolavirus Passive Immunization
The Lancet Infectious Diseases reported on November 30, 2023, that monoclonal antibodies (mAbs) were approved for emergency use by the U.S. FDA and used in clinical trials during the 2018–20 Ebola virus disease (EVD epidemic. These trials demonstrated that mAbs continued to increase the number of EVD survivors. The WHO recommended in 2022 that two monoclonal antibody treatments be used in the treatment of Ebola: mAb114 (Ansuvimab; Ebanga) and REGN-EB3 (Inmazeb). The U.S. National Institutes of Health (NIH) states that monoclonal antibodies (mAbs) are manufactured in a laboratory to combat a specific infection and are administered during an infusion. mAbs are different fromines, says the NIH.
On December 22, 2020, Ridgeback Biotherapeutics L.P. confirmed that the U.S. FDA approved Ebanga for the treatment of Ebola. The WHO issued a strong recommendation in August 2022.
On May 2, 2022, the U.S. FDA issued a priority review voucher for a material threat medical countermeasure (MCM) product application for INMAZEB (atoltivimab, maftivimab, and odesivimab-ebgn), manufactured by Regeneron Pharmaceuticals, Inc. As a result, the FDA approved Inmazed in October 2020.
On October 14, 2020, the U.S. Food and Drug Administration (FDA) approved an antibody cocktail from Regeneron that has been shown to reduce mortality rates associated with Ebola. The treatment, known as REGN-EB3, is a mixture of three monoclonal antibodies (atoltivimab, maftivimab, and odesivimab-ebgn) marketed under the brand name Inmazeb. Inmazeb is indicated for the treatment of infections caused by Zaire ebolavirus in adult and pediatric patients, including neonates born to mothers who are RT-PCR positive for Zaire ebolavirus infection.
The U.S. Administration for Strategic Preparedness and Response announced on October 4, 2022, a $109.8 million contract with Mapp Biopharmaceutical Inc. for the advanced development and potential purchase of an mAb therapy to treat Sudan Ebolavirus.
The Lancet Infectious Diseases published results from an observational cohort study on November 30, 202. The study concluded that almost 25% of survivors were seronegative on discharge from the Ebola treatment center, and antibody concentrations decreased rapidly over time. These results suggest that monoclonal antibodies may negatively impact the production of anti-Ebola virus antibodies in survivors of Ebola virus disease, potentially increasing the risk of reinfection or reactivation.
Ebolavirus Treatments
Obeldesivir (ODV; GS-5245) is an orally administered ester prodrug of the parent nucleoside GS-441524 with broad-spectrum antiviral activity inhibiting viral RNA–dependent RNA polymerases. Results from a study published in March 2025 support the potential of ODV as an oral post-exposure prophylaxis with activity against filoviruses, such as the Ebola virus.
On April 8, 2024, RedHill Biopharma announced that its two novel, oral, host-directed investigational drugs, opaganib and RHB-107 (upamostat), demonstrated a robust synergistic effect when combined individually with remdesivir (Veklury®), significantly improving viral inhibition while maintaining cell viability. Opaganib is believed to be the first host-directed molecule to show activity in the EVD, having recently delivered a statistically significant increase in survival time in a separate U.S. Army-funded in vivo Ebola virus study. When administered to the animals within 24 hours of virus exposure once daily for ten days, the drug conferred complete protection against lethal infection with Sudan ebolavirus. On October 14, 2024, RedHill announced an agreement with the U.S. Government.
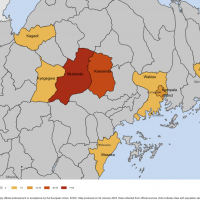
RHB-107 was recently accepted for inclusion in the ACESO PROTECT adaptive platform trial for the early treatment of COVID-19 patients in the outpatient setting. The 300-patient PROTECT Phase 2 RHB-107 arm has received FDA clearance to start. The study is being conducted in the U.S., Thailand, the Ivory Coast, South Africa, and Uganda, and is estimated to be completed by the end of 2024. RHB-107 met primary endpoints and demonstrated tolerability in the endpoint Phase 2 study, delivering promising efficacy results.