Search API
Before 2006, chikungunya fever infections were rarely identified in the United States. However, starting in 2014, cases of chikungunya began to appear among U.S. travelers returning from affected regions in the Americas.
Local transmission of the virus has since been documented in Florida, Texas, Puerto Rico, and the U.S. Virgin Islands.
As of August 19, 2025, there have been 50 reported travel-related cases in the U.S.
Last year, 199 cases were confirmed.
The U.S. Centers for Disease Control and Prevention (CDC) has highlighted several countries where travelers are acquiring this mosquito-borne disease.
The CDC has issued a chikungunya travel health notice for outbreaks in Bolivia, China, Kenya, Madagascar, Mauritius, France, the Department of Mayotte and Réunion, Somalia, and Sri Lanka.
According to the Pan American Health Organization (PAHO), Brazil is leading all countries in the region with over 204,000 cases in 2025.
The CDC recently wrote that international travelers can protect themselves by preventing mosquito bites. And, if you are pregnant, you should reconsider travel to the affected areas, particularly if you are close to delivering your baby.
"The CDC recommends chikungunya vaccination for travelers going to areas with current outbreaks, and also for people traveling to regions or countries with elevated risk—particularly if they'll be staying for six months or longer," Jeri Beales, MSN, RN, BS, informed Vax-Before-Travel.
"This is especially true for individuals who are older and have chronic conditions like diabetes."
"The list of countries and regions with ongoing outbreaks and elevated risks changes frequently, so be sure to seek advice from a travel clinic or physician's office that specializes in travel health before your trip," added Beales, with Destination Health Travel Clinic in the greater Boston, MA area.
Currently, two chikungunya vaccines are approved for use and commercailly in the U.S. at certified travel clinics and pharmacies.

As summer draws to a close in August 2025, millions of beachgoers flock to New Jersey's extensive coastline. While many vacationers enjoy the waves and surfing at the shore, this year, mosquito bites may become a popular topic of conversation.
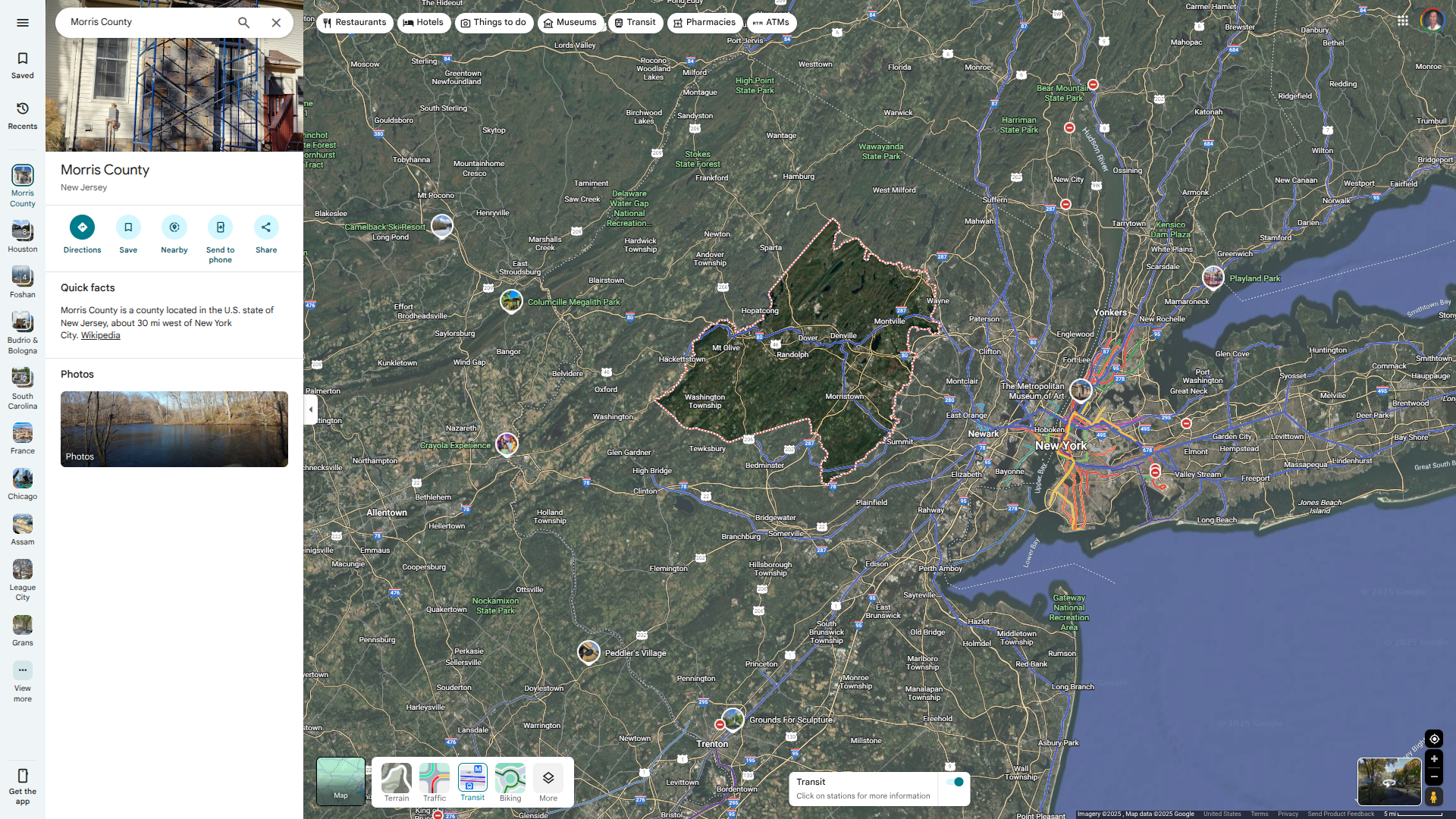
According to news posted today, the New Jersey Departments of Health (NJDOH) and Environmental Protection are investigating a case of malaria in a resident of Morris County with no international travel history.
NJDOH wrote on August 18, 2025, that it is possible the resident was infected by a virus-carrying mosquito with malaria in New Jersey.
If confirmed, this would be the first known locally acquired case of malaria in New Jersey since 1991.
"While risk to the general public is low, it's important to take the necessary precautions to prevent locally acquired malaria in New Jersey. The most effective ways are to prevent mosquito bites in the first place and to ensure early diagnosis and treatment of malaria in returning travelers,” said Acting Health Commissioner Jeff Brown, in a press release."
“Anyone traveling to countries with widespread malaria should take appropriate steps to prevent malaria while traveling and monitor for symptoms.”
Malaria is a mosquito-borne disease caused by a parasite transmitted by certain mosquitoes and is widespread in many tropical and subtropical countries.
For example, the state of Florida has reported numerious travel-related malaria cases involving travelers visiting Cuba in 2025.
While approved for use in Africa, malaria vaccines are currently unavailable in the United States.
The U.S. CDC reported today that the number of acute respiratory illnesses causing people to seek healthcare is at a very low level nationwide.
However, Respiratory Syncytial Virus (RSV) is a prevalent respiratory virus that is typically found first in Florida each year.
The CDC says young children face a higher risk of severe illness due to RSV.
Recent Florida Department of Health data show that Florida's RSV season lasts longer than in other parts of the country and exhibits unique regional patterns.
As of August 9, 2025, Florida reported there have been a total of 22 RSV outbreaks in the current season, with zero new outbreaks in the current week. Florida's Central Region, which includes Orlando, has reported 13 of these outbreaks this year.
Florida's health department notes that identifying unique seasonal and geographic trends in RSV activity in Florida has significant implications for prescribing patterns and initiating prophylaxis in children.
Additionally, the American Academy of Pediatrics (AAP) currently recommends that pre-approval for prophylactic treatment be made based on state surveillance data.
The CDC and AAP say RSV monoclonal antibody (mAb) therapy prevents serious lower respiratory tract disease (LRTD) caused by RSV in newborns and young children during their first RSV season.
A CDC report released on May 8, 2025, demonstrated that in 2024–25, RSV hospitalization rates were 45-52% lower in infants younger than 3 months old and 28-43% lower in infants younger than 8 months old who received an approved mAB compared to the 2018-2020 seasons before product introduction.
Both of these health agencies recommended that new mothers speak with a healthcare provider about immunization options before exposing an infant to RSV.
In addition to RSV, Florida has reported numerious chikungunya, dengue, and malaria cases in 2025.

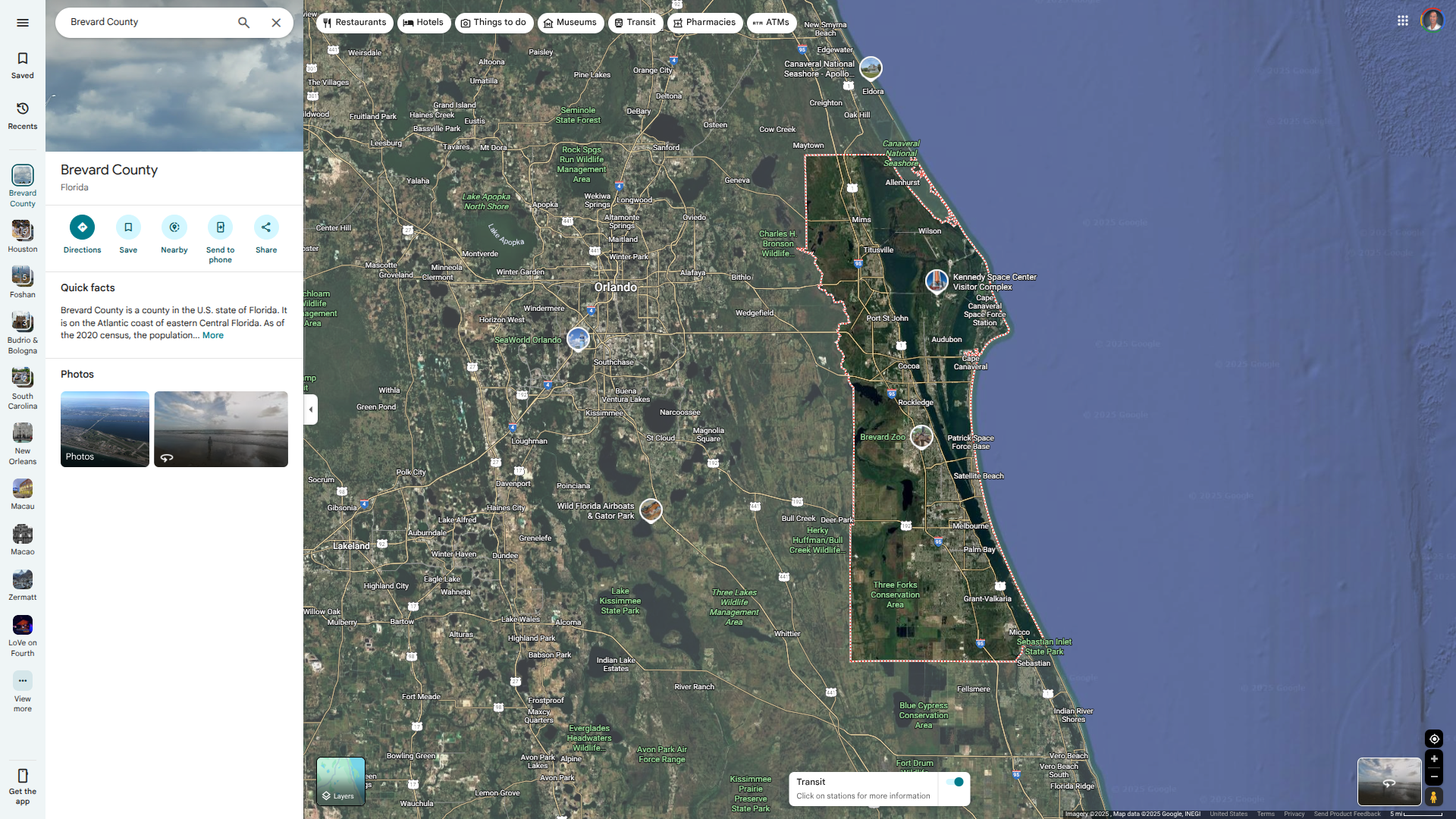
The Florida Department of Health (FDH) today reported that additional locally-acquired and travel-related Dengue fever cases have been confirmed in various counties in 2025.
As of August 9, 2025, FDH confirmed ten locally acquired dengue cases (DEN-3, DENV-4) were reported in Miami-Dade (2) and Brevard (8) counties in 2025.
While several cities are located in Brevard County, Melbourne has the largest population at risk for this mosquito-transmitted disease, with over 87,000 residents.
To alert residents, DOH-Brevard has issued a Mosquito-Borne Illness Alert that is scheduled to be in effect through September 12, 2025.
Additionally, there have been 141 travel-related Dengue cases in Florida, most related to travelers from Cuba.
The FDH says Dengue infections can present as a flu-like illness with severe muscle aches and joint pain, fever, and sometimes a rash, and may appear within 15 days after being bitten by an infected mosquito.
Furthermore, Dengue fever is not contagious.
Currently, Dengue vaccines are unavailable in the continental U.S. However, Puerto Rico is testing a first-generation vaccine on children.

There is a global resurgence of chikungunya that started with increasing outbreaks in the Indian Ocean islands in March 2025, which has continued into mid-August.
According to the World Health Organization (WHO), these outbreaks mirror trends seen 20 years ago when a major outbreak began in the Indian Ocean before spreading globally and affecting nearly half a million people.
Recent estimates suggest that 5.6 billion people live in areas suitable for the spread of diseases carried by the Aedes mosquito, including chikungunya.
In the Region of the Americas, over 209,000 cases and three related fatalities have already been confirmed in 2025.
In the United States, Florida has reported four travel-related cases of chikungunya confirmed this year. The countries of origin were Bolivia, Brazil, Indonesia, and Sri Lanka.
Eleven instances of chikungunya were confirmed in Florida in 2024
To clarify how this mosquito-borne disease is transmitted during international travel, the WHO published a new Q&A on August 8, 2025, with information for the public on the disease, how it spreads, its symptoms, treatment, prevention, and more.
Additionally, the WHO and the U.S. CDC recommend that those traveling to an area reporting chikungunya cases speak with a travel vaccine expert regarding prevention options.

While local cases of malaria are rarely reported in the United States, there were 10 cases across four states in 2023.
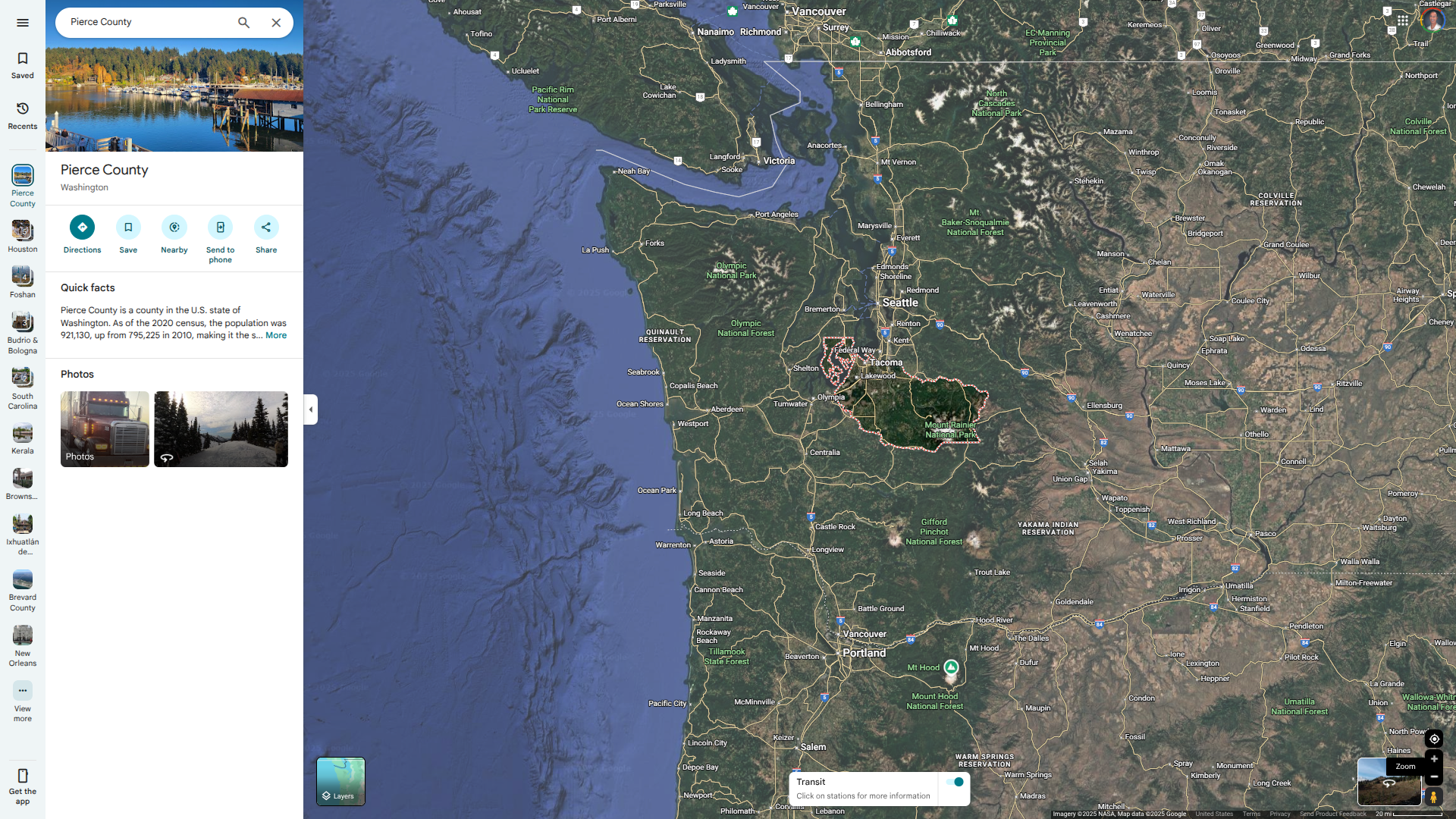
According to a news release, Washington State may soon be added to this list of affected areas.
On August 6, 2025, a press release announced that a resident of East Pierce County, who had not traveled recently, was diagnosed with malaria in early August. Dr. James Miller, the Tacoma-Pierce County Health Officer, stated, "The risk of contracting malaria in Pierce County remains very low."
"Malaria is generally rare in the U.S., and the vast majority of cases occur after exposure to countries where malaria transmission is ongoing."
In the U.S., approximately 2,000 to 2,500 cases of malaria are reported each year, primarily linked to travel. In 2025, states like Florida have reported numerous travel-related cases (28), related principally to travelers from Cuba.
Previously, Florida reported local cases on both coasts.
It is important to note that malaria does not spread directly from person to person.
Malaria is a mosquito-borne disease caused by a parasite. The incubation period—the time from infection to the onset of symptoms—ranges from 7 to 30 days.
Malaria can be treated and cured with prescription antimalarial medications; however, if not diagnosed and treated quickly, it can become life-threatening.
In Africa, two approved vaccines that help prevent malaria are currently in use. However, as of August 7, 2025, these vaccines are not available in the U.S.
Historically, local cases of dengue fever have been concentrated in Miami-Dade County. However, recent reports indicate that mosquitoes in northeast Florida are now also transmitting the disease, placing about 600,000 people at risk.
On August 2, 2025, the Brevard County health department reported its sixth locally acquired dengue case of the year.
In response, the Florida Department of Health in Brevard County (DOH-Brevard) has issued a Mosquito-Borne Illness Alert that expires in September 2025.
DOH-Brevard and Brevard County Mosquito Control are coordinating surveillance and prevention efforts along this Atlantic Ocean coastal community by enhanced monitoring for mosquitoes and diseases, as well as targeted mosquito treatment and overnight spraying to reduce the risk of disease transmission.
This area of Florida includes these cities: Melbourne, Titusville, and Cocoa Beach. And to the west, Orlando.
Two other local dengue cases were reported by Miami-Dade in 2025.
Furthermore, there have been over 120 travel-related dengue cases confirmed in Florida in 2025.
Dengue fever is not contagious, causes flu-like symptoms, and can be prevented with vaccination. Currently, a first-generation dengue vaccine is being evaluated in children living in Puerto Rico.
Globally, a second-generation dengue vaccine is offered in numerious countries in 2025.
The Louisiana Department of Health (LDH) recently announced it was urging residents to take precautions to prevent infection from Vibrio vulnificus.
As of July 31, 2025, 17 cases of Vibrio vulnificus have been reported by LDH among Louisiana residents. All of these patients were hospitalized, and four of these illnesses resulted in death.
Of those 17 cases, 75% reported wound/seawater exposure.
During the same period over the previous 10 years, an average of seven Vibrio vulnificus cases and one death have been reported each year in Louisiana.
LHD says Vibrios are bacteria that naturally live in warm coastal waters and are found in higher numbers between May and October, when water temperatures are warmer.
About a dozen species of Vibrio can cause human illness. Some species, such as Vibrio vulnificus, can cause severe and life-threatening infections. Many people with Vibrio vulnificus infection can become seriously ill and need intensive care or limb amputation.
About one in five people with this infection dies, sometimes within a day or two of becoming ill. It can cause illness when an open wound is exposed to coastal waters or when a person eats raw or undercooked seafood, particularly oysters.
LHD wrote in this press release the precautions that can help keep you safe:
Stay out of brackish or salt water if you have a wound, including cuts and scrapes.
Wash wounds and cuts thoroughly with soap and water if they have been exposed to brackish or salt water, raw seafood, or raw seafood juices.
Use caution when consuming raw or undercooked seafood, especially if you have a weakened immune system, are pregnant, or have certain medical conditions like liver or stomach disorders. And wear protective gloves when handling raw seafood.
More information from LDH can be found at this U.S. CDC link.
Along the eastern Gulf of America, Florida reported 11 Vibrio vulnificus infections in various countries this year.
The Florida Department of Health reported that fatalities had occurred in Hillsborough, Bay, Broward, and St. Johns counties in 2025.
In 2024, Florida reported 82 cases and 19 fatalities, many in Citrus, Hernando, Hillsborough, Lee, Pasco, Pinellas, and Sarasota counties.

Throughout 2025, the Florida Department of Health has reported travel-related cases of Dengue fever and Oropouche fever in international travelers returning from Cuba.
Recent data from the Pan American Health Organization indicates that Chikungunya fever, which is also transmitted by mosquitoes, may soon be added to Florida's list of health concerns.
As of August 5, 2025, there have been a total of eight locally acquired Chikungunya cases reported in Cuba this year, with an outbreak confirmed in the Matanzas municipality of Perico, according to the Pedro Kourí Institute of Tropical Medicine.
In Florida, four travel-related cases of Chikungunya were confirmed as of July 2025, with the countries of origin being Bolivia, Brazil, Indonesia, and Sri Lanka.
Fortunately, Chikungunya is a vaccine-preventable disease, with two options available in the United States.
Furthermore, Florida has confirmed 59 dengue cases related to travel from Cuba have been reported in 2025.
Additionally, in 2024, there were 103 reported cases of Oropouche fever among individuals who had traveled to endemic regions, including Cuba.
Cuba is currently included in Oropouche Travel Health Advisories issued by the U.S. CDC.
The CDC recommends that when planning a visit to Cuba, you speak with a travel vaccine advisor regarding routine and travel vaccine options at least one month before departure.

The European Centre for Disease Prevention and Control (ECDC) recently highlighted cases of Oropouche virus disease in Europe that are linked to international travel, as noted in their Communicable Disease Threats Report.
As of July 25, 2025, the ECDC has reported that Germany confirmed one imported case of Oropouche virus disease. This case involved a person who had traveled to Dominica between January 24 and February 7, 2025.
France also reported one imported case in an individual who visited Brazil in March 2025.
Additionally, the United Kingdom recorded three imported cases among travelers returning from Brazil during March and April 2025.
Throughout 2024, there were a total of 44 imported cases of Oropouche reported in EU countries, with Spain accounting for the highest number at 23 cases. Most cases had a travel history to Cuba, and one case was linked to Brazil.
The ECDC assesses the risk of infection for EU/EEA citizens traveling to countries in the Americas affected by the Oropouche as moderate.
They state, "The likelihood of human exposure to Oropouche virus in the EU/EEA is considered very low. This is despite the potential for further cases to be imported, as the competent vectors typically found in the Americas are absent from continental Europe.'
'To date, there has been no reported secondary transmission. Therefore, the risk of locally acquired Oropouche virus disease in the EU/EEA is low.'
In the United States, there were 103 cases of Oropouche fever reported in individuals in Florida who had traveled to an endemic area, such as Cuba, in 2024.
As of July 31, 2025, there are no Oropouche vaccines available.
