Search API
According to recent data from Japan's public health institute, the number of infectious gastroenteritis cases caused by norovirus and other pathogens in Japan has reached the highest level in ten years.
As of mid-March 2025, there were 34,609 norovirus cases reported by the National Institute of Infectious Diseases.
According to Japan's Ministry of Health, Labor and Welfare, most reported cases of infectious gastroenteritis are viral, primarily affecting infants and school-age children.
Like "infectious diarrhea" in Western terminology, norovirus is classified as a causative pathogen and a foodborne infection.
Historically, norovirus cases in Japan are detected in early winter, peak in December due to viruses like RSV, have a smaller peak in spring associated with rotavirus, and continue into early summer.
Bacterial infections, such as Vibrio parahaemolyticus, are more common in summer.
In summary, the Ministry says these infections can be categorized as sporadic or epidemic diseases in the region or as part of foodborne infectious diseases.
The U.S. CDC says norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis and stomach inflammation among people of all ages in the U.S.
Norovirus causes 58% of foodborne illnesses acquired, resulting in about 900 deaths, mostly among adults aged 65 and older, each year.
Furthermore, the CDC has reported 12 norovirus outbreaks on cruise ships. In 2024, 18 norovirus outbreaks were confirmed on U.S.-based cruises.
As of March 28, 2025, the U.S. government has not approved a norovirus vaccine for commercial use.

Even with a vaccination requirement to visit most Yellow fever endemic countries, the Pan American Health Organization (PAHO) has issued a new Epidemiologic Alert regarding increased human cases in 2025.
As of March 26, 2025, the PAHO wrote that health officials have confirmed 131 Yellow fever (YF) cases in four countries, 53 of them fatal, indicating a 40.4% case-fatality rate.
Brazil has 81 confirmed cases, 31 of which have been fatal.
The other YF cases have been reported in the Plurinational State of Bolivia, Colombia, and Peru.
In 2025, YF cases have also been detected in the state of São Paulo in Brazil and the department of Tolima in Colombia, regions outside the Amazon region.
The PAHO/WHO wrote 'It is essential that countries achieve vaccination coverage of at least 95% in populations in at-risk areas, in a homogeneous manner, and that health authorities ensure that they have a strategic reserve inventory that allows them to maintain routine vaccination and, at the same time, respond effectively to possible outbreaks.'
When departing to South America from the United States in March 2025, YF vaccination services are offered at most travel clinics and pharmacies. Once immunized, a certificate that is essential to enter certain countries will be generated.

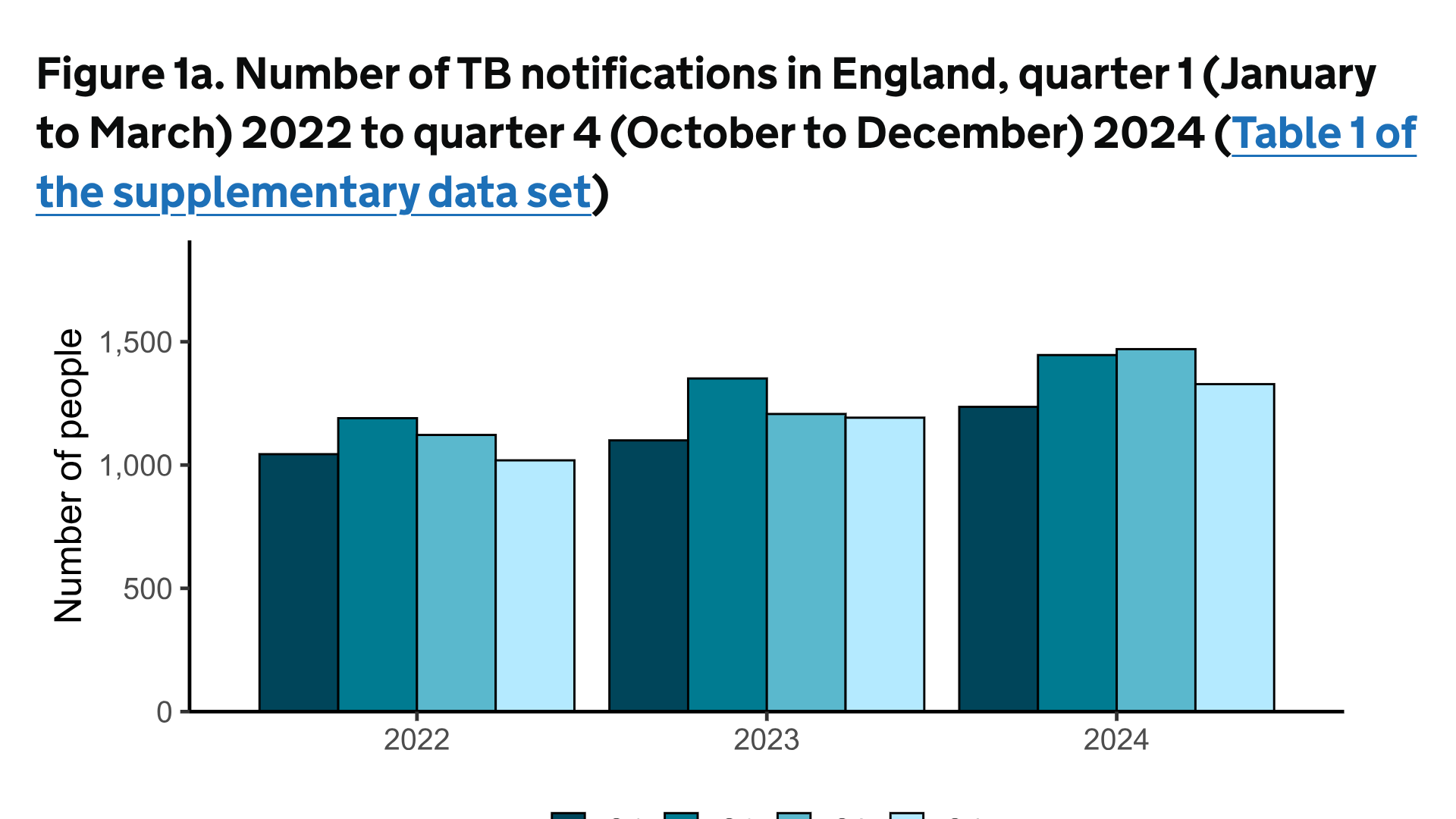
Tuberculosis (TB) is the leading cause of death from a single infectious agent worldwide, including in England.
The UK Health Security Agency (UKHSA) report announced on March 24, 2025, reveals that TB remains a significant public health concern in England.
Data indicates that reported TB notifications increased by 13% in 2024, from 4,850 to 5,480 people, compared with 2023.
The most significant geographic increases were in London and the West Midlands
The UKHSA writes, ' If this rate of increase persists, the UK risks losing its WHO low incidence status of 10 cases per 100,000 population.'
According to the UKHSA, there is a strong association between the increase in TB incidence and the rise in migration, with about 81% of all notifications in 2023 coming from people born outside the UK. Work is underway to identify the optimal and most cost-effective control and prevention strategies to tackle this increase.
One tactic to reduce TB cases in children listed by the UKHSA is to optimize the use of Bacillus Calmette–Guérin (BCG) vaccines provision through commissioning and specification to include vaccinating infants at four weeks of age. While about 50% effective, BCG vaccination is an inexpensive defence against treating TB cases.
The global average cost for BCG vaccination is about $5.00. According to USAID, treating a tuberculosis case in the U.S. costs about $20,000, and a drug-resistant tuberculosis case can cost over $150,000.
The French Republic's overseas department and region of Réunion today reported a serious spike in Chikungunya cases. Over the last week, 4,156 new cases were reported.
This data indicates a 16% increase in Chikungunya cases compared to the previous week.
Furthermore, emergency department activity increased from 78 admissions the previous week to 128 during March 10-16, 2025.
During early March, Réunion health authorities announced two virus-related deaths.
Since this Chikungunya outbreak began in August 2024, 13,594 cases, 15 serious cases (eight adults and seven newborns) have been reported, setting an unfortunate record for a French department or region.
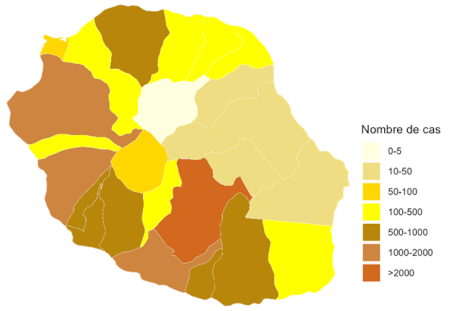
Réunion's southern and western municipalities are the most affected. Le Tampon remains the most affected municipality.
However, this mosquito-transmitted virus has increased sharply in Possession, Saint Andrew, Saint Paul, and Saint Suzanne.
As part of the Mascarene Islands, Réunion is a vacation destination for many travelers. It is located east of Africa, Madagascar, and southwest of Mauritius.
France has issued a Level 4 emergency for Réunion to alert visitors of this health emergency, and the U.S. CDC issued a Level 2 Advisory regarding La Réunion's Chikungunya outbreak.
To reduce the impact of this outbreak, Valneva SE and the Agence Régionale de Santé La Réunion recently announced an agreement to deliver at least 40,000 IXCHIQ® vaccine doses starting in early April 2025. The French government funded this purchase.
In the U.S. and various countries, Chikungunya vaccines are approved and available at travel clinics and pharmacies. They are recommended for international travelers visiting endemic countries such as La Réunion.
As sexually transmitted diseases continue to spread in 2025, a new vaccine candidate may reduce the number of chlamydia cases in the United States. Current programs to prevent infection rates from rising have proven insufficient, highlighting the urgent public health need for a vaccine.
Sanofi announced today that the U.S. Food and Drug Administration has granted a fast-track designation to Sanofi's mRNA vaccine candidate for preventing chlamydia infection.
The chlamydia vaccine candidate has been designed to protect against primary genital tract infection and reinfection by the bacterium Chlamydia trachomatis.
In 2020, there were 129 million worldwide cases of chlamydia among adults and adolescents, with the highest rates of infection among younger people.
Jean-François Toussaint, Global Head of Vaccines R&D, stated in a press release on March 26, 2025, "Millions of people currently live with undiagnosed chlamydia, including asymptomatic infection that can also cause severe long-term health effects if left untreated."
"Antibiotics to treat chlamydia have not been successful in controlling rising infection rates. With our program, we aim to make chlamydia a preventable disease through vaccination."
Following a promising preclinical program, Sanofi is planning a phase 1/2 randomized clinical study to evaluate the immunogenicity and safety of the chlamydia vaccine candidate in adults aged 18 to 29.
This clinical study is due to start in the coming days.
Chlamydia, caused by the bacterium Chlamydia trachomatis, is a common bacterial infection of the reproductive tract with consequences for developing infertility and pregnancy complications.
Although chlamydia can be treated with antibiotics when diagnosed, over 80% of chlamydia cases are asymptomatic, meaning there is a significant risk that infections go unrecognized, leading to untreated cases and unintentional transmission.
A study published by the Annals of Family Medicine on March 24, 2025, indicates that many women are not receiving guideline-adherent treatment in primary care settings. For example, the time to treat chlamydia was longer for patients aged 50-59 years (time ratio relative to those aged 20-29 years = 1.61; 95% CI, 1.12-2.30).
The development of this vaccine candidate is part of the Translational Science Hub, a partnership with the Queensland Government, Griffith University, and the University of Queensland that connects world-class researchers in Queensland, Australia, with Sanofi scientists in France and the U.S.
As of late March 2025, the FDA, the United Kingdom, and the European Medicines Agency have not approved a vaccine to prevent chlamydia infections.

With about 100 different types of pneumococcal bacteria infecting people, innovative vaccines are needed to reduce various illnesses, including pneumonia, meningitis, and bloodstream infections.
For example, in Europe, 17,700 confirmed invasive pneumococcal disease (IPD) cases were reported in the European Union/European Economic Area in 2022.
To address this disease, Merck announced today that the European Commission (EC) has approved CAPVAXIVE® (V116), designed to help protect adults against IPD and pneumococcal pneumonia.
CAPVAXIVE targets the serotypes causing most IPD cases in adults and includes eight unique serotypes not covered by other approved vaccines.
This EC decision authorizes the approval of CAPVAXIVE (Pneumococcal 21-valent Conjugate Vaccine) in all 27 European Union (EU) member states, including Iceland, Liechtenstein, and Norway.
“By focusing on the serotypes that have been responsible for an increasing proportion of adult invasive pneumococcal disease cases, CAPVAXIVE allows us to offer protection specifically designed for adults,” said Dr. Paula Annunziato, senior vice president, infectious diseases and vaccines, Global Clinical Development, Merck Research Laboratories, in a press release on March 26, 2025.
“We are proud to bring CAPVAXIVE to adults in Europe who may benefit from its broad protection and are eager to continue working with regulatory authorities to expand CAPVAXIVE availability worldwide.”
The EC approval is based on safety and immunogenicity data from the Phase 3 STRIDE clinical program.
As of late March 2025, various pneumococcal vaccines are offered in the United States at clinics and pharmacies.
Note: This VBT news article was updated for trademark on March 27, 2025.

Without a preventive vaccine available in the United States, an innovative treatment for uncomplicated urinary tract infections (uUTIs) has been approved.
New treatments are needed as the number of uUTIs caused by drug-resistant bacteria has increased, which can result in higher treatment failure rates.
GSK plc today announced that the U.S. Food and Drug Administration (FDA) has approved Blujepa, a first-in-class oral antibiotic with a novel mechanism of action that is GSK's infectious diseases portfolio.
Blujepa is approved for the treatment of female adults (≥40 kg) and paediatric patients (≥12 years, ≥40 kilograms) with uUTIs caused by Escherichia coli, Klebsiella pneumoniae, Citrobacter freundii complex, Staphylococcus saprophyticus, and Enterococcus faecalis.
GSK's Chief Scientific Officer, Tony Wood, commented in a press release on March 25, 2025, "The approval of Blujepa is a crucial milestone with uUTIs among the most common infections in women.
"We are proud to have developed Blujepa, the first in a new class of oral antibiotics for uUTIs in nearly three decades."
uUTIs are the most common infection in women, impacting up to 16 million women in the U.S. annually.
Over half of all women are affected by uUTI in their lifetime, with approximately 30% suffering from at least one recurrent episode, which can cause significant patient burden, including discomfort and restriction of daily activities.
Two other products have been approved for use.
Pivya™ (Pivmecillinam) is an extended-spectrum penicillin antibiotic. Pivya targets penicillin-binding protein-2 in the cell wall of gram-negative bacteria, and has been available in Europe.
ORLYNVAH™ is a U.S. FDA-approved novel oral penem antibiotic for treating uUTIs caused by the designated microorganisms Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis in adult women.
While an oral UTI vaccine is available in several countries in 2025, Uromune™ (MV140) is unavailable in the U.S.
However, international travelers can request a vaccine appointment using this Vax-Before-Travel link.

When visiting countries in the Americas in 2025, travelers to areas where the Zika virus is known to be present are at risk of infection.
However, it can be challenging to determine the exact level of risk in each Zika outbreak.
According to the U.K. Travel Health Pro, those who stay for extended periods in regions where the Zika virus is common face a higher risk. Nevertheless, even short-term visitors may be exposed to the virus, such as in the Federative Republic of Brazil.
As of March 25, 2025, about 2,556 Zika cases have been reported in Brazil since the beginning of 2025.
Most of these cases have been reported in Mato Grosso, São Paulo, Acre, and Rio Grande do Norte. Mato Grosso is a mountainous state in west-central Brazil, mainly covered by the Amazon rainforest.
Just to the south, the Argentine Republic has reported 433 Zika cases this year.
Previously, the U.S. CDC removed a Level 2 Travel Advisory in 2021 regarding Argentina's Zika outbreak.
To the north, in the United States, no Zika cases have been confirmed in 2025.
Last year, the U.S. CDC reported 19 non-congenital Zika cases among U.S. residents, primarily in Puerto Rico.
With millions of international travelers expected to visit these areas in 2025, Zika vaccines will not be available. However, several Zika vaccine candidates are conducting clinical research and aspiring for future U.S. FDA approval.