Search API
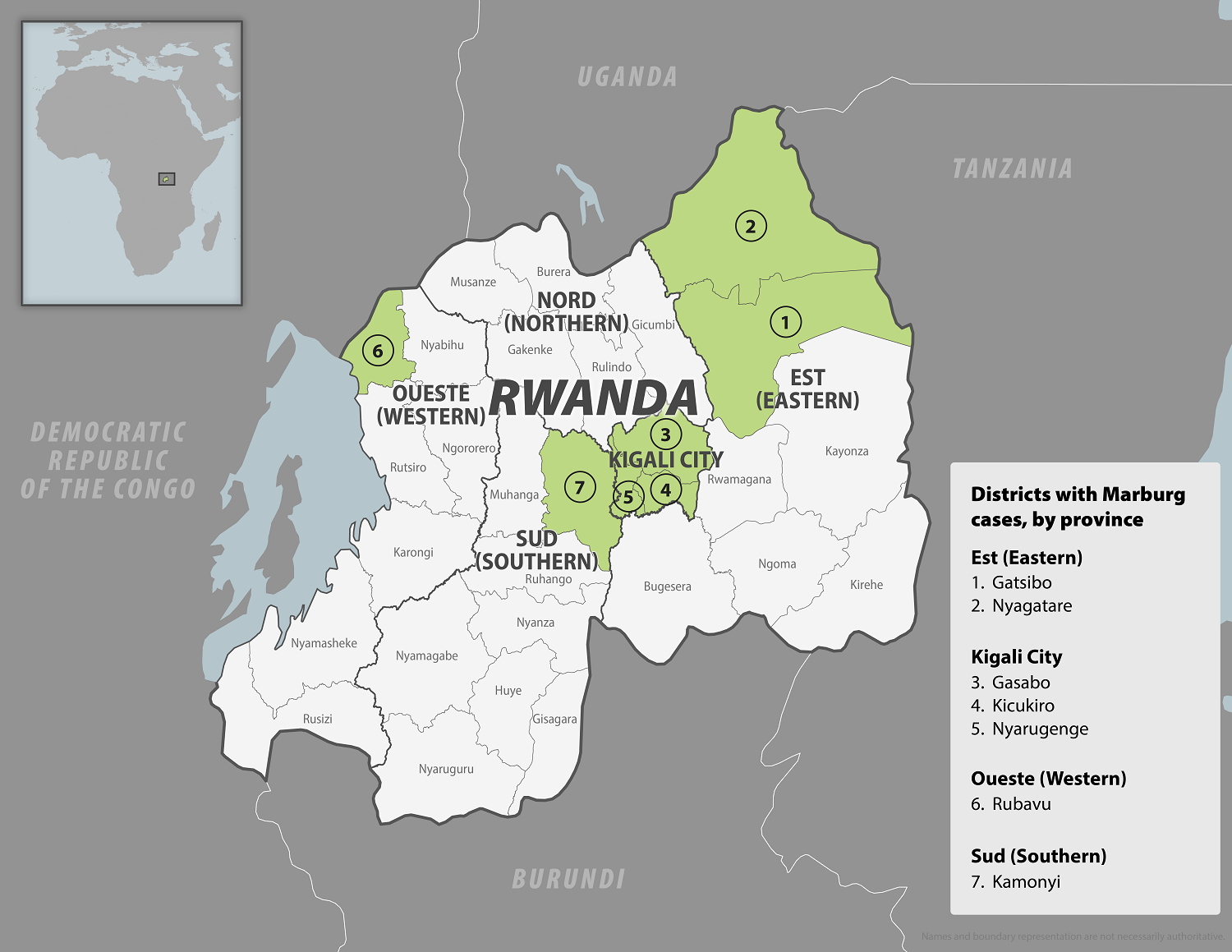
In early October 2024, the Republic of Rwanda began vaccinating frontline health workers in a Phase 2 rapid response open-label clinical trial to combat the reaction to the ongoing Marburg virus disease (MVD) outbreak, which has already claimed 14 lives.
Sabin Vaccine Institute’s single-dose Marburg vaccine candidate was selected to be administered in accordance with the clinical protocol reviewed and approved by Rwandan ethics and regulatory authorities. However, this is not a U.S. FDA-approved vaccine.
As of October 12, 2024, Sabin announced it had delivered approximately 1,700 investigational vaccine doses to Rwanda.
“In an outbreak, every moment counts, and our seamless collaboration with the Rwandan government was key to accelerating the process. On our side, we moved quickly by leveraging our experience with other outbreaks and having vaccine doses and supporting documents ready, thanks to a strong partnership with ReiThera,” says Sabin's CEO Amy Finan in a press release.
Sabin has extensive expertise in advancing vaccines for filoviruses, with two programs currently in Phase 2 clinical trials—one for Marburg and the other for Sudan ebolavirus.
The U.S. government has obligated $235 million to Sabin to advance vaccine research and development against Sudan ebolavirus and MVD.
As of October 13, 2024, other MVD vaccine candidates are conducting clinical research.
Previously, the U.S. CDC announced that people should reconsider nonessential travel to the Republic of Rwanda and that those who arrive in the U.S. may be screened for the virus at certain airports.
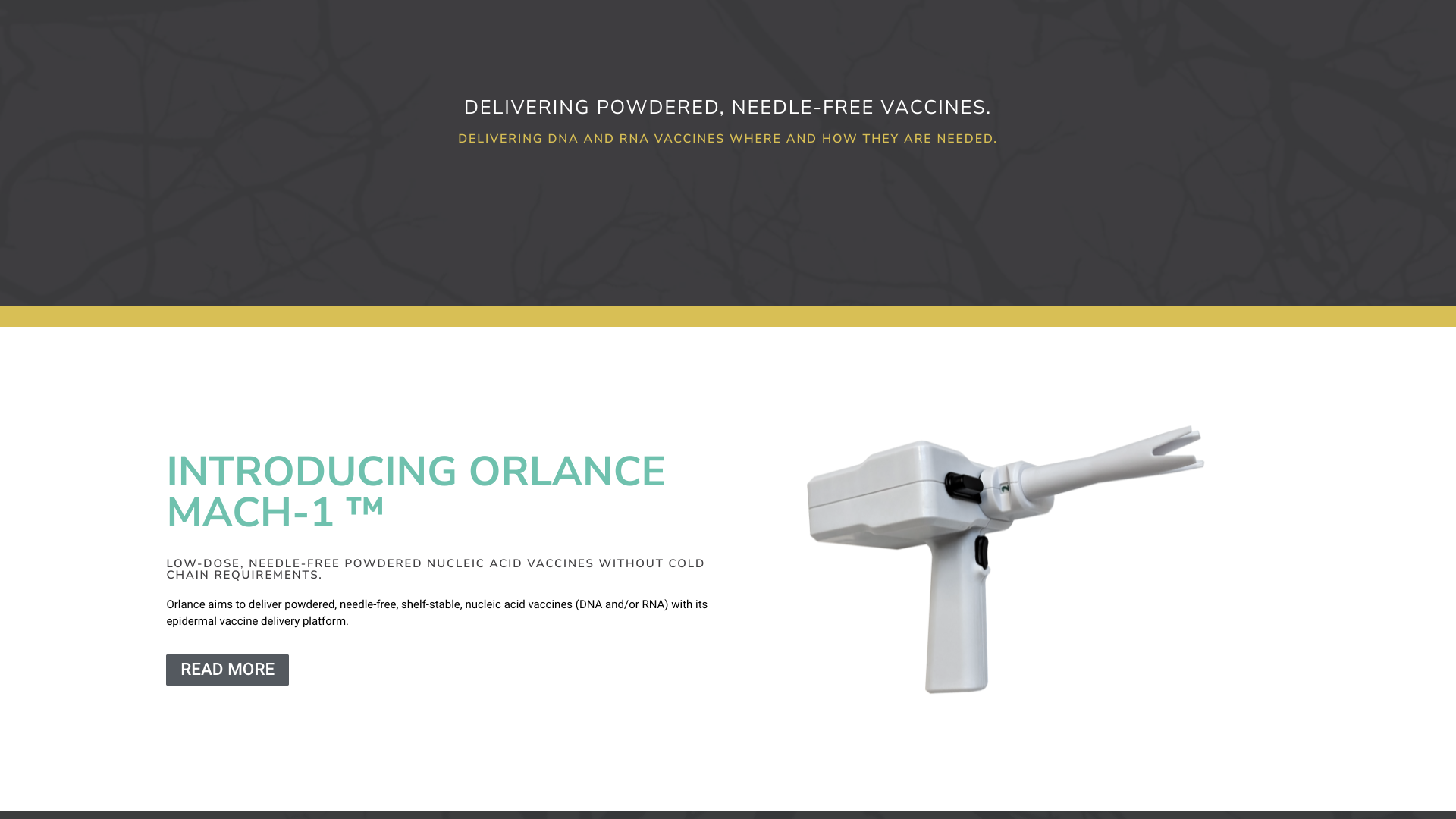
Orlance, Inc. today announced it was awarded the National Institutions of Health (NIH) Fast Track Small Business Innovation Research (SBIR) grant to develop an Enhanced Seasonal Influenza Vaccine.
This vaccine is intended to provide better protection against disease even in years when predicted vs. actual circulating strains are highly mismatched.
The award includes $300,000 for Phase 1, with the total funding for the Phase 1 and 2 combined program amounting to $3.3 million.
This Fast Track SBIR grant will enable Orlance to leverage its innovative MACH-1 powdered vaccine and immunotherapy platform to address seasonally changing and highly conserved influenza immunogens in ways that are impossible with other platforms.
Specifically, this program builds upon Orlance's universal influenza vaccine, which targets conserved antigens consistent across multiple virus lineages and adds seasonally changing influenza antigens to maximize protection.
The MACH-1 platform is a high-performance microparticle 'gene gun' technology that efficiently and uniquely delivers DNA or RNA vaccine-coated microparticles directly into cells in the uppermost layer of the skin.
MACH-1 delivery harnesses this environment and the natural machinery of its immune cells to deliver DNA and RNA vaccines encoding proteins that trigger potent immunity, including antibodies to block an infection and T cells that can eliminate infected cells.
Unlike currently licensed mRNA vaccines, MACH-1-delivered vaccines are stable at room temperature, painless, and needle-free. Orlance MACH-1 vaccines also trigger protective immunity levels with the smallest doses achieved within the field.
"NIH's continued funding support of the MACH-1 platform, including this enhanced seasonal influenza vaccine, reinforces the potential impact and significant step forward MACH-1 can bring to vaccine technology," adds Kristyn Aalto, Orlance CEO, in a press release on October 10, 2024.
This award brings Orlance's SBIR funding to $16.8M for next-generation generation DNA and RNA vaccines and therapeutics.
The U.S. FDA's Center for Biologics Evaluation and Research is conducting the 187th meeting of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) today.
This committee of vaccine experts will discuss the strain selection for Influenza Virus Vaccines for the 2025 Southern Hemisphere flu season on October 10, 2024. Each year, the VRBPAC discusses how the influenza virus is evolving and if it impacts exciting flu shot efficacy.
On October 3, 2024, the U.S. CDC reported that five Southern Hemisphere countries reported flu shots were about 35% effective during the last flu season.
Previously, on September 27, 2024, the World Health Organization announced its recommendations for the viral composition of influenza vaccines for the 2025 influenza season in the Southern Hemisphere.
Another presentation on the agenda is the 'Highly Pathogenic Avian Influenza A(H5Nx) Virus Surveillance and Characterization' in the U.S. and globally, and review recommendations for candidate vaccine virus development.
Over the past few months, the U.S. government has substantially invested in developing preventive vaccines for a potential avian influenza pandemic.
Instructions on listening to this VRBPAC meeting are found at this FDA link.

Thousands of healthcare professionals, advocates, and public policymakers from over 170 countries are participating in the annual Global TB Summit as the world confronts the resurgence of tuberculosis as the second deadliest infectious disease.
After a decline of about 2% per year between 2020 and 2022, the global tuberculosis incident rate rose by 3.9% in 2022. An estimated 10.6 million people worldwide fell ill with tuberculosis in 2022, leading to 1.3 million deaths.
“Tuberculosis remains a significant global threat, even though it is both preventable and curable. At the Global TB Summit 2024, we focus on the most pressing challenges. Our mission is clear: to harness innovation and foster global collaboration in our fight against this deadly disease. Only by coming together and leveraging our collective expertise can we seek to have a TB-free world,” said Glen Hansen, Chief Medical Officer at QIAGEN, in a press release on October 7, 2024.
After 27 years of declining tuberculosis cases, in 2023, the 50 U.S. states and the District of Columbia provisionally reported 9,615 TB cases, representing an increase of 16% compared with 2022.
Many of the cases were confirmed in children living with adults infected with TB.
The U.S. CDC stated in March 2024, 'Continued progress toward TB elimination will require strong public health systems capable of maintaining essential disease prevention and control activities.'
One of the prevention options is vaccination since TB is a vaccine-preventable disease.
Globally, there are over ten tuberculosis vaccines available in 2024.
In the U.S., the BCG vaccine is not commercially available or integrated into the CDC's vaccination schedule for children.
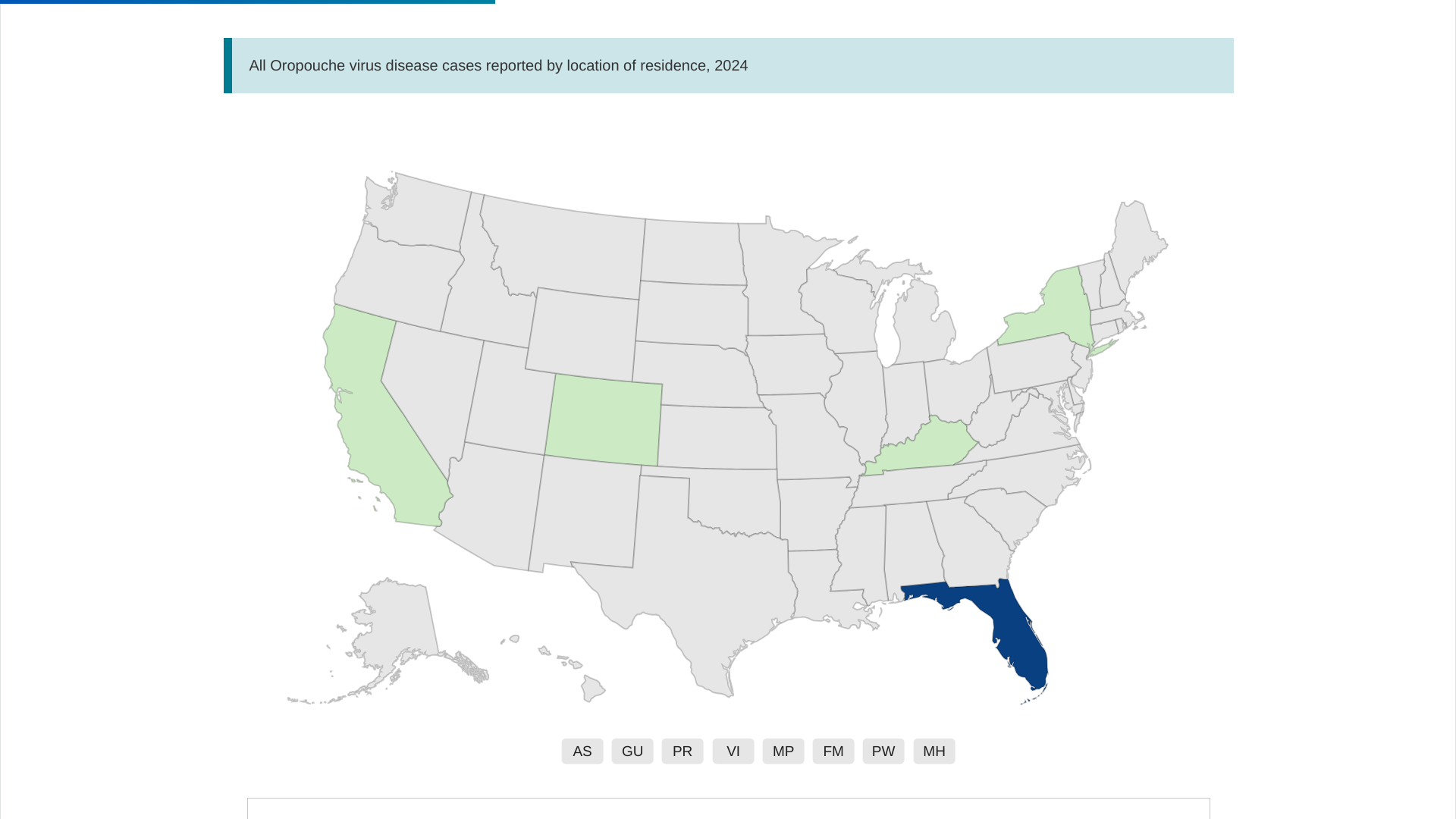
Recent experiences with the introduction of Chikungunya and Zika viruses to the United States could foretell what might occur with the Oropouche virus because all three arboviruses are maintained in an urban cycle between humans and arthropod vectors.
Both Chikungunya and zika viruses are transmitted by Aedes (Stegomyia) mosquitoes, which oviposit and develop in containers in and around homes. This makes persons more susceptible to mosquito exposure and, ultimately, infection.
In contrast, the primary Oropouche vector, the biting midge, is low-abundance in North America and primarily resides in tree holes in the southeast and midwestern U.S., says the U.S. CDC Emerging Infectious Disease, Volume 30, Number 11—November 2024.
As of October 7, 2024, local transmission of the Oropouche virus had not been reported in the United States, although 92 cases have been reported in travelers, primarily arriving from Cuba.
Cuba is in the midst of its peak rainy season, which is associated with increased vector abundance. This suggests that more travel-associated cases might be expected in the U.S., in particular, Puerto Rico.
The U.S. CDC wrote on October 1, 2024, that various factors are likely to affect the risk of the local spread of the virus, including the rate of introduction from travel-associated cases, the presence and distribution of the vectors and potential host reservoirs, and potential virus adaptation.
Should the virus infect wild bird populations in North America, it is possible that the Oropouche virus could become endemic, similar to the progression of the West Nile virus, says the CDC.
While Chikungunya has one approved vaccine and several Zika vaccine candidates are progressing in clinical research, Oropouche vaccine research is in its early stages in 2024.