Search API
The Walgreens Flu Index recently identified the top 10 areas in the United States with influenza activity.
As of December 21, 2024, these unfortunate leaders are located in the southern section of the central U.S.:
- Birmingham (Anniston and Tuscaloosa), Ala.,
- Beaumont-Port Arthur, Texas,
- Harlingen-Weslaco-Brownsville-McAllen, Texas,
- Monroe, La.-El Dorado, Ark.,
- Huntsville-Decatur (Florence), Ala.,
- Knoxville, Tenn.,
- New Orleans, La.,
- Jackson, Miss.,
- Nashville, Tenn.
- Shreveport, La.
Walgreens's Flu Index is compiled using retail prescription data for antiviral medications used to treat influenza across Walgreens locations nationwide. The Flu Index illustrates which populations are experiencing the highest incidence of flu.
Seperately, the U.S. CDC published Key Updates for Week 51, ending December 21, 2024.
Nationally, the percentage of influenza positivity, the percentage of emergency department visits for flu, the rate of outpatient visits for respiratory illness, and influenza-associated hospitalizations increased this week compared to last week.
And 5 pediatric deaths associated with seasonal influenza virus infection were reported this week, bringing the 2024-2025 flu season total to nine pediatric deaths. Last flu season, 206 pediatric deaths were related to influenza.
This flu season, there is an ample supply of influenza vaccines at local pharmacies; over 92 million flu shots have been distributed in the U.S., targeting the 2024-2025 flu season.

According to data from the California Department of Public Health, the number of Valley fever cases will set new records in 2024.
As of the end of November, 11,076 valley fever cases had been confirmed statewide, a 20% increase compared to 2023.
Kern County is California's hot spot for the disease again, accounting for 3,768 reported cases.
Home to the city of Bakersfield, Kern County spans the southern end of the Central Valley and is home to less than 1 million people.
Other impacted counties include Los Angeles, Riverside, Fresno, Kings, Merced, San Francisco, San Joaquin, San Luis Obispo, Santa Barbara, and Stanislaus.
Historically, Valley fever has also spread in the states of Arizona, Nevada, and New Mexico.
According to the U.S. CDC, Valley fever, also known as coccidioidomycosis, is a lung infection caused by a fungus found in soil. Usually, people who get sick with Valley fever get better independently, but some people will need antifungal medication.
As of December 28, 2024, scientists continue working on a preventive vaccine, but the CDC has not recommended a Valley fever vaccine.

The Victorian Department of Health recently announced that Australia's surveillance program detected vaccine-derived poliovirus type 2 (VDPV2) in pre-treated sewage from the Western Treatment Plant in Melbourne.
Melbourne has over 5 million residents and is the host city of the Australian Open 2025, which hundreds of thousands of tennis fans attend.
The poliovirus detection (Advisory number: 241224) on December 2, 2024, is likely linked to an individual who received a live polio vaccine and shed the virus in Victoria. Victoria's Chief Health Officer, Dr. Clare Looker, wrote on December 23, 2024, that Australia remains polio-free, as this wastewater detection is not a wild-type poliovirus case.
However, the U.S. CDC says the detection of poliovirus in wastewater cannot be used to determine the total number of infected persons in a community or the portion of the infected population. The minimum number of infected individuals that can be reliably detected through wastewater testing is not known.
To alert the international community, the World Health Organization (WHO) confirmed in December 2024 that the spread of the poliovirus remained a Public Health Emergency of International Concern. In 2022, the United States was added to the WHO's list of polio-identified countries.
Over the past few years, more than 1 billion 'triple-locked' nOPV2 vaccines have been administered to prevent virus mutations.
In the United States, the inactivated polio vaccine is offered.
"Most travelers to Australia don't need many travel vaccines, but with poliovirus detected in sewage in Melbourne, a once-in-a-lifetime booster dose of polio vaccine would be prudent before departure," commented Beverly Schaefer, travel vaccine expert at Katterman's Sand Point Pharmacy, Seattle, WA.
The U.S. CDC suggests that international travelers speak with a travel vaccine expert about Japanese encephalitis, which is mainly a concern in the Murray River and the Outer Torres Strait Islands area. All international travelers should also be vaccinated against measles with the MMR vaccine.

The World Health Organization (WHO) today published an updated Disease Outbreak News regarding an undiagnosed disease in the Democratic Republic of the Congo (DRC), which was published on December 8, 2024.
As of December 27, 2024, the WHO identified this condition as an acute respiratory infection complicated by malaria.
Recent laboratory results from 430 samples indicated positive results for malaria and several common respiratory viruses, including Influenza A (H1N1, pdm09), rhinoviruses, human coronaviruses, parainfluenza viruses, and human adenoviruses.
These findings suggest a combination of common and seasonal viral respiratory infections and falciparum malaria, compounded by acute malnutrition, which has led to a rise in severe infections and deaths, disproportionately affecting young children.
This led to a significant increase in reported cases, with 891 cases documented as of December 16. However, the number of deaths reported weekly (48 deaths during this period) has remained relatively stable.
The DRC's health ministry had reported a fatality rate of 6.2%. Young children represent 64.3% of all reported cases.
The WHO wrote that this event highlights the significant burden of common infectious diseases, such as acute respiratory infections and malaria, particularly in vulnerable populations.
Additionally, the WHO recommends the programmatic use of malaria vaccines for children living in malaria-endemic areas.
The WHO and the European Medicines Agency recommend Mosquirix™ (RTS,S/AS01) and R21 / Matrix-M™ vaccines for travelers visiting malaria-endemic countries.
As of December 27, 2024, seventeen African countries are deploying malaria vaccines unavailable in the U.S.

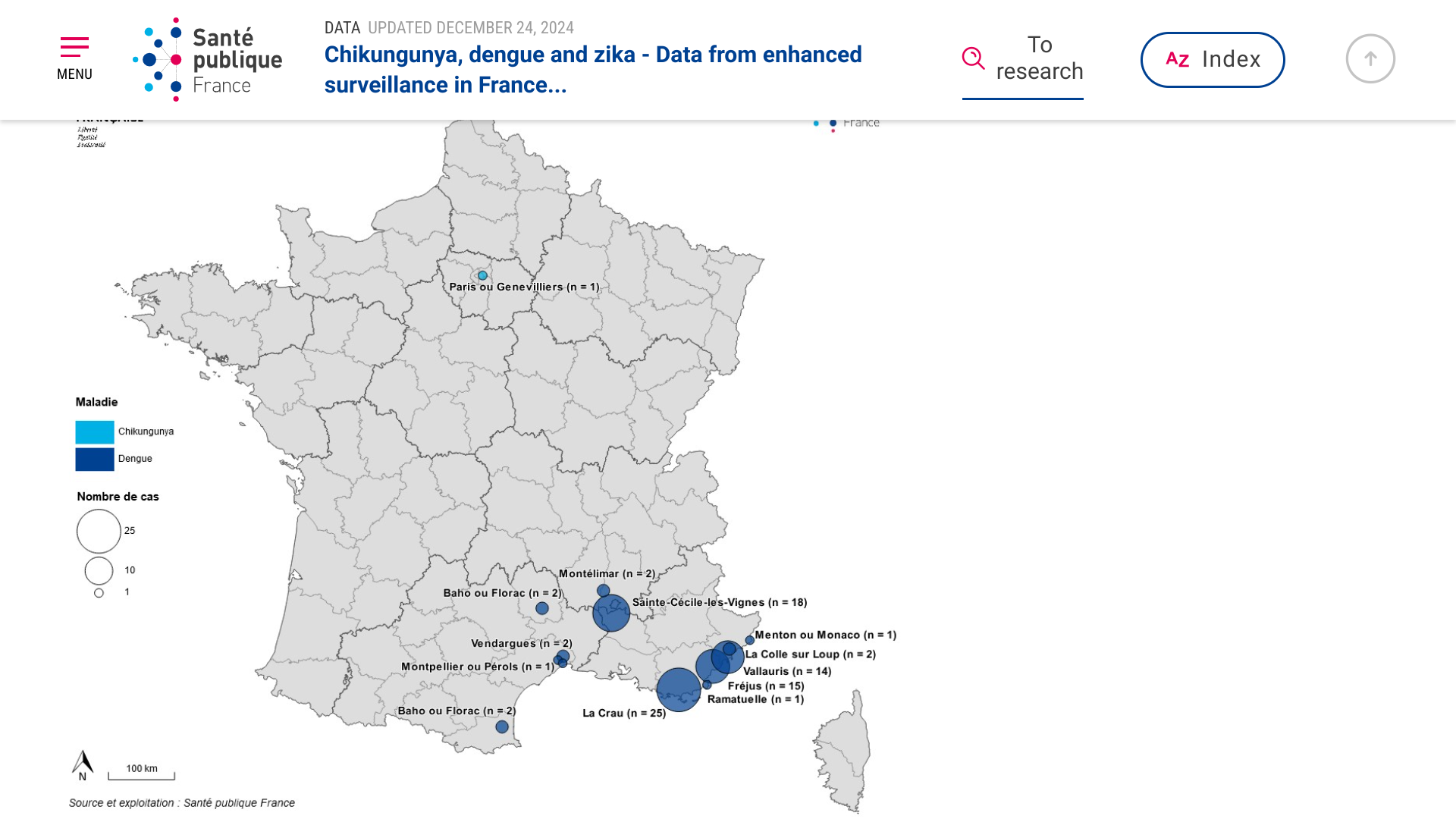
According to Regional Health Agencies (ARS), France has reported the highest number of indigenous (local) dengue cases in 2024 since the implementation of enhanced surveillance in 2006.
As of December 24, 2024, the ARS assessment for this 2024 season shows 11 outbreaks of local dengue transmission totaling 83 cases, mainly occurring in Provence-Alpes-Côte d'Azur (Marseille, 1.9 million pop.) and Occitanie.
As of December 17, 2024, 4,694 imported dengue cases had been reported this year, the highest annual number ever. Epidemiological investigations identified imported dengue cases from travelers returning to France from Guyana, Reunion, and Indonesia.
ARS also reported one Indigenous case of chikungunya for the first time in Ile de France.
Entomological and epidemiological investigations were immediately implemented for each disease outbreak, accompanied by vector control actions.
From a disease prevention perspective, France offers various chikunguna and dengue vaccines.
For travelers departing from the U.S., Valneva SE's IXCHIQ® chikungunya vaccine is offered at numerous travel clinics and pharmacies.