Search API
The Texas Department of State Health Services (DSHS) today reported the measles outbreak now totals 722 cases, with 92 people hospitalized, and two related fatalities.
As of May 20, 2025, DSHS reported 15 additional measles cases, led by Harris County, including Houston.
Similar to the outbreaks in Ontario, Canada, which have resulted in 1,846 measles cases in 2025, the vaccination status of the individuals in West Texas remains unknown.
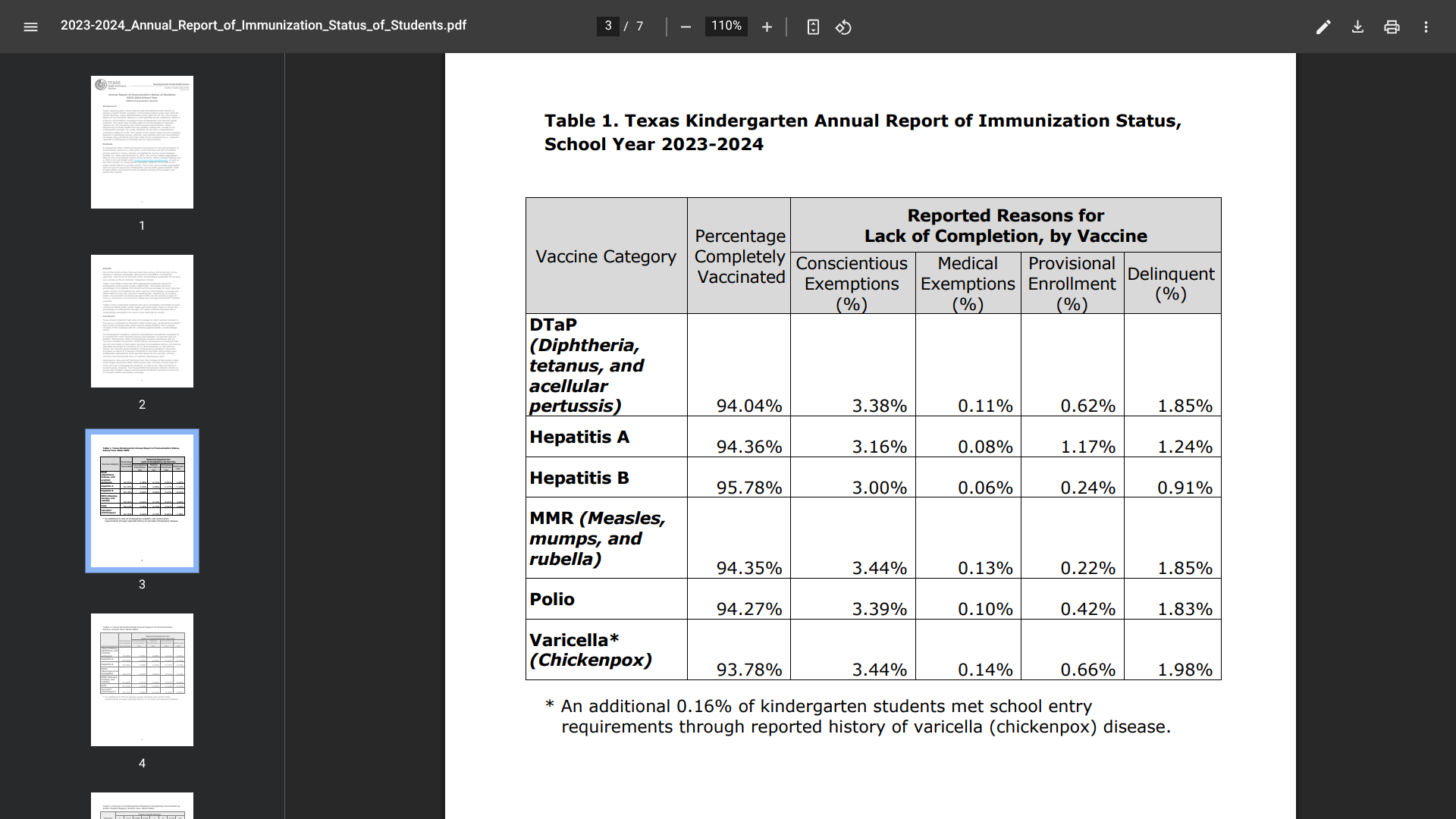
However, Texas also disclosed positive data regarding school-age vaccinations.
Texas requires public school districts and accredited private schools to submit a report of their students’ immunization status every year.
In seventh grade, immunization coverage was above 95% for all vaccines except Tdap and meningococcal MCWY vaccines.
In Texas, people can get vaccinated by going to their healthcare provider or a pharmacy. Vaccines are also available through the Texas Vaccines for Children and Adult Safety Net Providers.
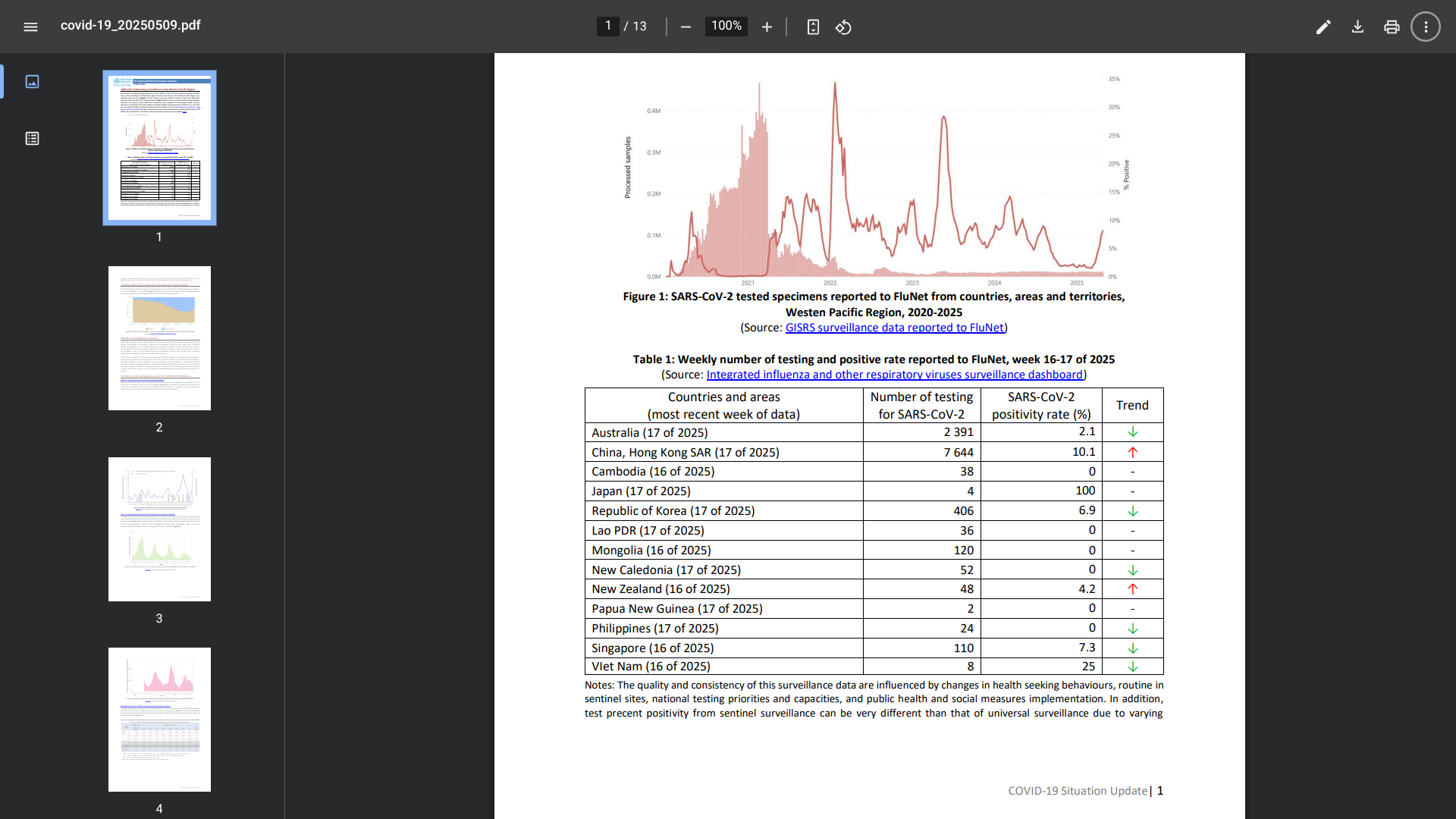
While neighboring countries Singapore and Hong Kong have confirmed surges in COVID-19 cases in May 2025, Malaysia's Health Ministry recently reported that the situation remains below the alert level.
As of May 20, 2025, the Health Ministry's website reported that over 11,000 COVID-19-19 cases have been recorded this year, with a continuous downward trend since the start of 2025.
COVID-19-related hospital admissions in Malaysia have decreased in the past few weeks, with a 7-day average of 37 admissions compared to 45 in late April 2025.
This positive news compares with Singapore's 28% increase in COVID-19 cases in early May 2025.
The WHO's Bi-weekly COVID-19 Situation Update, published on May 9, 2025, revealed that eight countries and areas in the Western Pacific Region reported a COVID-19 positivity rate of 8.1%.
And the relative frequency of circulating variants in the Western Pacific Region was JN.1 at 51.3% and B.1.1.529 at 48.3%.
In the United States, the CDC estimates that COVID-19 infections are growing or likely to grow in 2 states, declining or likely declining in 30 states, and not changing in 14 states, as of May 13, 2025.
From a disease prevention perspective, Malaysia, the WHO, and the U.S. CDC recommend that at-risk people speak with a healthcare provider about vaccination options.
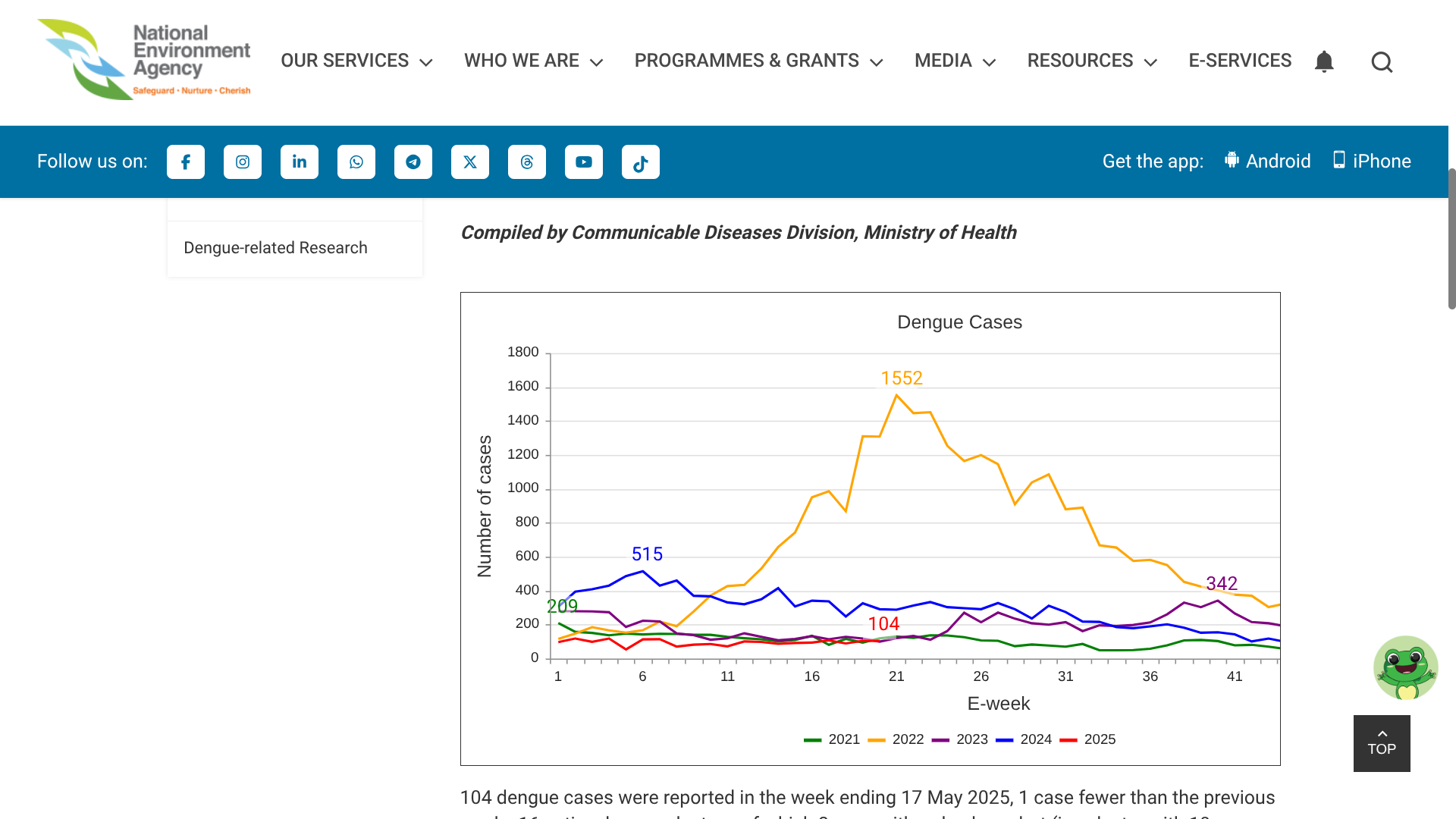
As the global number of Dengue cases began to mount in 2025, several countries in the Pacific Region, such as the Republic of Singapore, are reporting weekly increases.
The island country and city-state of Singapore in Southeast Asia has recorded several recent Dengue outbreaks.
As of May 20, 2025, Singapore's National Environment Agency (NEA) wrote, 'Collective community action and vigilance are critical to help prevent a surge in Dengue cases this year.'
NEA reported 104 Dengue cases in the week ending May 17, 2025, 1 case fewer than the previous week.
Furthermore, there are 16 active Dengue clusters, of which there were with red alerts,
Persistent transmission has been noted in the cluster at Hougang Avenue 1 (106 cases). The large clusters at Begonia Drive/Dedap Road (33 cases) and Woodlands Avenue 1/Woodlands Street 31 (30 cases) have relatively fast transmission rates, with an increase of 10 and 12 cases, respectively, from the previous week.
Among the four Dengue virus serotypes circulating in Singapore, Dengue virus serotype 2 has been predominant in Singapore since September 2023.
Globally, data indicates that over 2.5 million Dengue cases and 1,305 related fatalities have already occurred in 2025, with the U.S. reporting 1,760 travel-related Dengue cases and one local case this year.
While a second-generation Dengue vaccine is available in about 40 countries, it is unavailable in Singapore and the United States in 2025.
The U.S. CDC does recommend various routine and travel vaccinations before visiting Singapore.
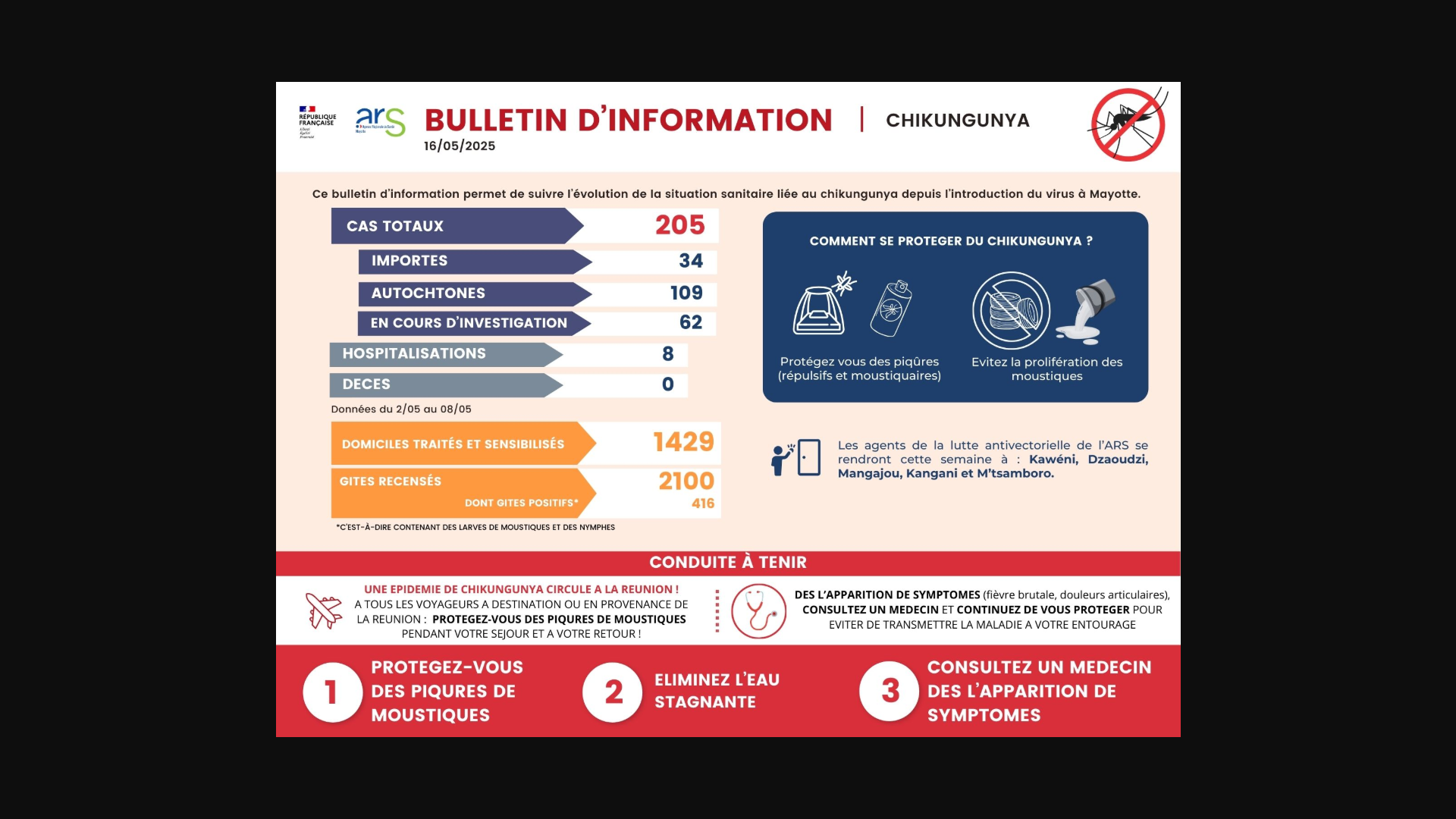
As the Chikungunya virus outbreak continues in the Indian Ocean countries, the French Department of Mayotte has become another hotspot for this mosquito-transmitted, vaccine-preventable disease.
As of May 16, 2025, Regional Health Agency (ARS) Mayotte reported 205 confirmed Chikungunya cases, including 34 imported cases, 109 locally acquired cases, and 62 cases currently under investigation.
From a severity perspective, these infections have led to eight hospital admissions during this year's outbreak.
'Given the evolving situation and the risk of an epidemic in the coming weeks, Mr. Sergio Albarello, Director General of ARS Mayotte, in consultation with Mr. François-Xavier Bieuville, Prefect of Mayotte, has decided to activate today the transition to level 2B of the ORSEC plan,' wrote ARS Mayotte.
Furthermore, ARS says it is also possible to get vaccinated against Chikungunya in Mayotte at various locations. Valneva's IXCHIQ® Chikungunya vaccine is recommended to combat severe forms of the disease for people aged 18 to 64 with comorbidities. The latter is available upon medical prescription and free of charge for these people.
In the United States, the CDC recommends that certain international travelers be vaccinated before visiting Chikungunya outbreak areas in 2025.
Member States of the World Health Organization (WHO) today formally adopted the world's first Pandemic Agreement.
Announced on May 20, 2025, the decision by the 78th World Health Assembly culminated in more than three years of negotiations launched by governments in response to the devastating impacts of the COVID-19 pandemic.
Regarding national sovereignty, Agreementent states that: "Nothing in the WHO Pandemic Agreement shall be interpreted as providing the Secretariat of the World Health Organization, including the Director-General of the World Health Organization, any authority to direct, order, alter or otherwise prescribe the national and/or domestic law, as appropriate, or policies of any Party, or to mandate or otherwise impose any requirements that Parties take specific actions, such as ban or accept travellers, impose vaccination mandates or therapeutic or diagnostic measures or implement lockdowns."
The new Agreement was driven by the goal of making the world safer and more equitable in response to future pandemics, such as Disease X.
According to the WHO, Disease X represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease.
On April 4, 2025, the WHO's Global Health Emergency Corps announced a framework designed to strengthen countries' emergency workforce, coordinate the deployment of surge teams and experts, and enhance collaboration between governments, which was tested.
Disease X was first included in the WHO Blueprint for Epidemics in February 2018, aiming to accelerate the development of medical countermeasures. It is expected to be caused by a "pathogen X," likely a zoonotic disease or infection that can be transmitted between humans and animals.
In the United States, the National Institutes of Allergy and Infectious Diseases (NIAID) developed a Pandemic Preparedness Plan to prepare for future public health emergencies caused by infectious diseases.
While it is recognized that pathogens other than viruses could lead to public health emergencies, the NIAID Pandemic Preparedness Plan focuses on viruses that could cause epidemics or pandemics.

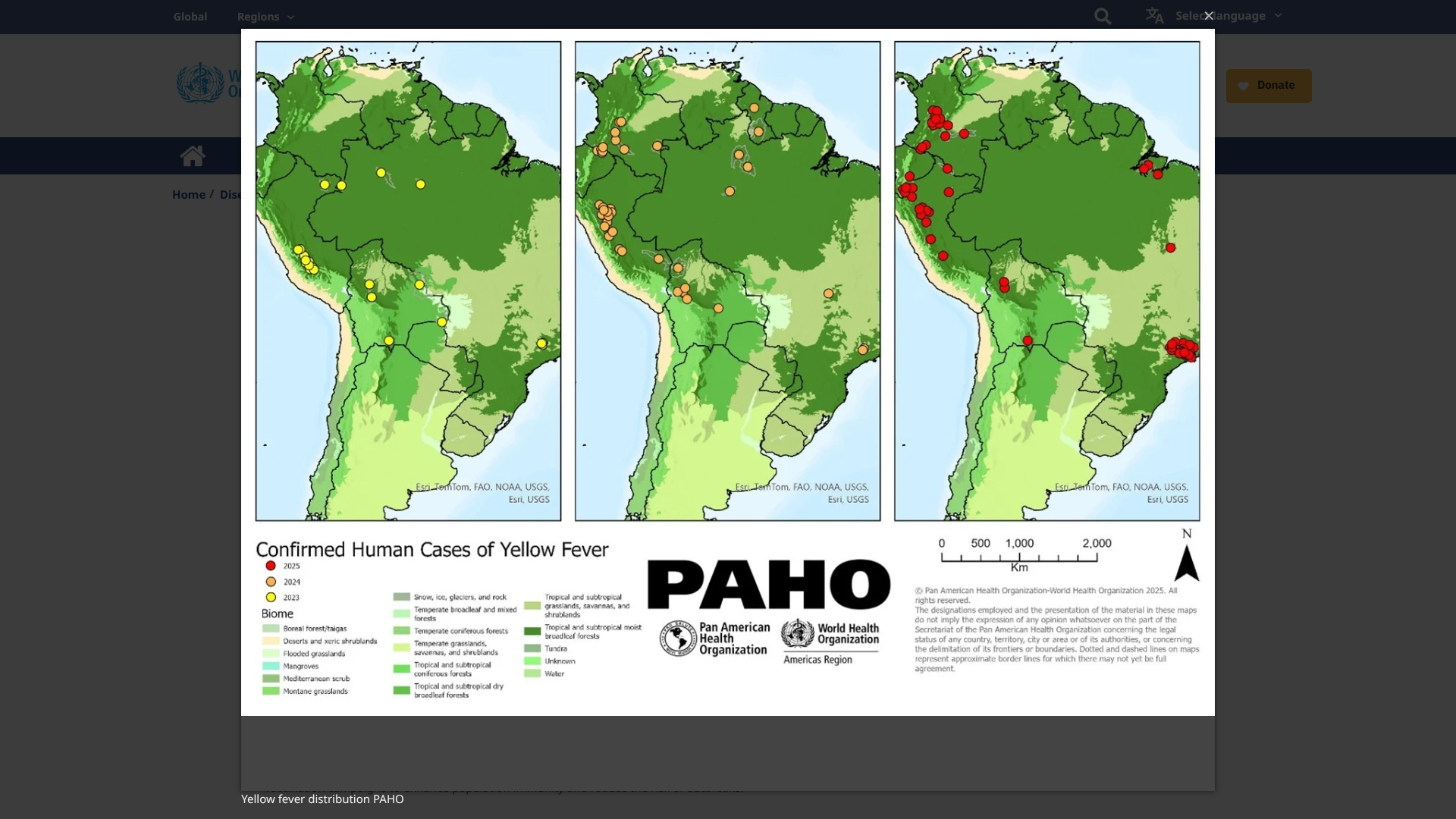
Researchers believe the yellow fever virus has existed in the Region of the Americas since the 17th century and is now considered one of the most dangerous mosquito-transmitted infectious diseases.
According to the World Health Organization (WHO, DON570), as of May 16, 2025, the YF virus has become endemic in tropical areas of 13 countries in the Americas.
During 2025, five countries in the Americas reported 212 confirmed human cases of yellow fever, including 85 deaths (CFR 40%).
The YF cases were reported in the Plurinational States of Bolivia, Brazil, Colombia, Ecuador, and Peru.
The WHO writes that the 'occurrence of yellow fever outside of the Amazon basin contributes to the overall classification of YF risk in the Americas, especially in endemic countries, as high.'
WHO emphasizes that vaccination remains the primary means for preventing and controlling yellow fever.
The WHO continues to support countries in expanding Sanofi Pasteur YF-VAX® vaccination coverage through routine immunization programs and mass vaccination campaigns, enhancing population immunity and reducing the risk of outbreaks.
In the United States, the CDC recommends yellow fever vaccination at least ten days before visiting outbreak areas. YF vaccination appointments are at travel clinics and pharmacies in May 2025.