Search API
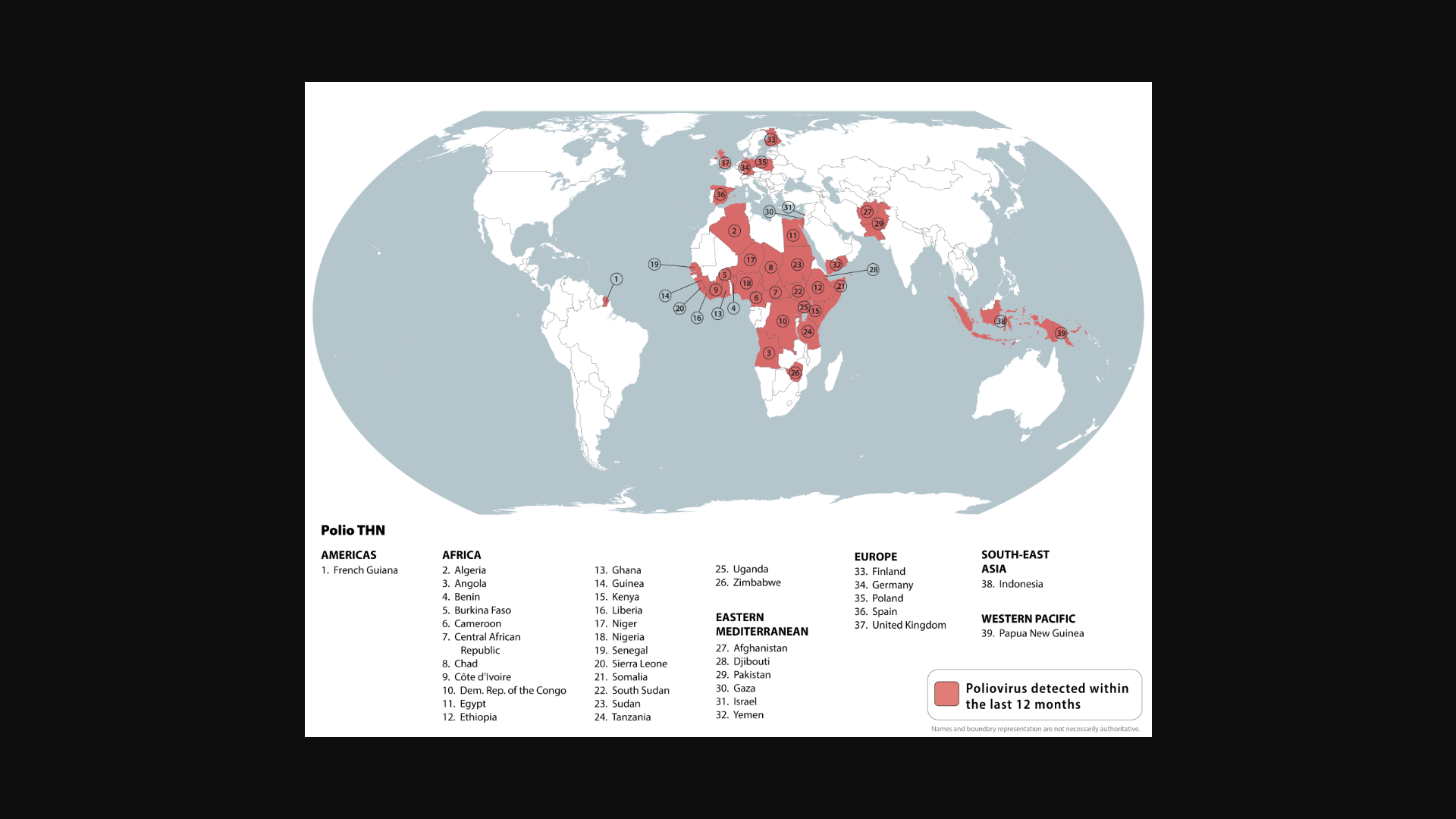
Global health leaders recently discussed the final steps needed to eradicate polio during an event titled "United to Finish the Job: High-Level Side Event on Polio Eradication," which was co-hosted by the Global Polio Eradication Initiative (GPEI).
Leadership from the GPEI emphasized the need for sustained funding to complete the eradication effort, highlighting the Kingdom of Saudi Arabia's pledge of $500 million to the GPEI. This funding, along with that from other critical donors, is enabling the partnership to reach hundreds of millions of children each year with lifesaving polio vaccines and ultimately end the transmission of the virus.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, commented in a press release on September 22, 2025, "Polio eradication is a shared responsibility."
"We can finish the job only through sustained collaboration and commitment from donors such as the Kingdom of Saudi Arabia, which has been an essential supporter through its critical political, social, technical, and financial contributions."
The focus was on the urgent need to end wild polio transmission in Afghanistan and Pakistan, while also addressing outbreaks of variant poliovirus in fragile settings across Africa and Asia.
These countries and others were highlighted in the U.S. CDC's Global Polio Travel Health Notice, Level 2 - Practice Enhanced Precautions. The CDC identified 39 countries where poliovirus remains a health risk.
The CDC list includes the United Kingdom, which has previously reported detections of poliovirus in wastewater samples in London.
The CDC recommends that before any international travel, you ensure you are up to date on your polio vaccines. Adults who have previously completed the entire routine polio vaccine series may receive a single lifetime booster dose of polio vaccine.
While the US and UK governments have previously issued health advisories for ongoing Chikungunya and Measles outbreaks in the Republic of Madagascar in 2025, a Level 3, Reconsider Travel advisory was issued today.
As of September 27, 2025, the US Department of State announced that protests occur throughout the country, and they can turn violent without warning. US citizens should stay in place and avoid areas with protests or demonstrations, as protests may develop quickly, especially after dark.
Furthermore, the State Department recommends enrolling in the Smart Traveler Enrollment Program to receive important updates and digital alerts from the US Embassy.
Enrolling helps the local embassy contact you or your designated emergency contact in the event of an emergency. For local assistance, the Embassy in Madagascar is located at Lot 207 A Andranoro, Antehiroka, 105 Antananarivo.
Moreover, have a plan to leave in an emergency that does not depend on the US government's help.
'We highly recommend purchasing travel insurance before visiting Madagascar, located off the east coast of Africa, and west of France's Mayotte and Reunion,' writes the US Embassy.

The U.S. Centers for Disease Control and Prevention (CDC) today issued a Level 2 Travel Health Advisory regarding the ongoing outbreak of Chikungunya Fever in Cuba.
Local media reported on September 26, 2025, that Andrés Lamas Acevedo, provincial director of Hygiene, Epidemiology, and Microbiology, stated the most affected territories are Matanzas, Cárdenas, Colón, Jovellanos, Jagüey Grande, and Pedro Betancourt.
Previously, in late August, the U.S. Embassy in Havana reported an increase in the number of arbovirus cases, including Chikungunya.
Chikungunya is caused by a virus that is transmitted to humans through the bites of infected mosquitoes. The CDC recommends vaccination for travelers before visiting an area with a Chikungunya outbreak.
For example, visitors from Cuba have been diagnosed in Florida with Chikungunya this year.
Additionally, the CDC advises that if you are pregnant, you should reconsider travel to the affected areas, particularly if you are close to delivering your baby. Mothers infected around the time of delivery can pass the virus to their baby before or during delivery.
Newborns infected in this way or by a mosquito bite are at risk for severe illness, including poor long-term outcomes.
In the United States, approved Chikungunya vaccines are commercailly available at travel clinics and pharmacies.

Israel's Ministry of Health today reported that another unvaccinated toddler has died from measles. This is the fifth death since the outbreak began this year, three of which occurred in the past week.
On September 25, 2025, the Ministry's press release confirmed that 21 measles cases were hospitalized, most of them children who had not been vaccinated. Of these, six children are in intensive care.
Additionally, the Ministry recommends an additional dose for infants in outbreak zones or before traveling to areas affected by the outbreak.
Areas currently defined as outbreak zones: Jerusalem, Beit Shemesh, Bnei Brak, Harish, Modi’in Illit, Nof HaGalil, Kiryat Gat, and Ashdod.
In these zones, you can visit family health centers (Tipat Halav), HMOs, and special measles vaccination stations. No appointment is needed.
In addition to measles, Israel is confronting the spread of poliovirus in 2025.
The U.S. CDC's Level 2, Practice Enhanced Precautions, Global Polio Travel Health Advisory issued on August 4, 2025, included Israel.
The CDC warns international travelers to Israel are at increased risk of exposure to poliovirus and has published updated recommendations for polio vaccinations for children and adults, which should be administered before traveling abroad.
The CDC also recommends various routine and travel vaccines before visiting Israel in 2025. These vaccines are offered in the U.S. at travel clinics and pharmacies.

The New Mexico Department of Health (NMDOH) recently declared the state's measles outbreak, which started in February 2025, to be over, as the last case was reported in Santa Fe County in mid-August.
According to the U.S. CDC, measles outbreaks are considered 'over' when 42 days pass without new cases, a timeframe that represents twice the virus's maximum incubation period.
One hundred cases of measles were identified during this outbreak, which was New Mexico's largest in decades. The outbreak began in Lea County, likely from exposures to an outbreak in neighboring Texas.
"We are thankful to the thousands of New Mexicans who received their measles, mumps, and rubella (MMR) vaccine," said Dr. Chad Smelser, NMDOH acting state epidemiologist, in a press release on September 26, 2025.
"Fully vaccinated people and those who got caught up with their vaccines during this outbreak prevented it from spreading further."
New Mexicans received over 56,000 MMR vaccines since February. The MMR vaccine remains widely available in New Mexico clinics and pharmacies for anyone who wishes to receive it.

With numerous travelers returning from African countries infected with malaria, access to treatment has become limited in the United Kingdom.
Neon Healthcare recently advised the UK's NaTHNaC that 250mg mefloquine (Lariam) antimalarial tablets are currently out of stock in the UK and will not be available until January 2026.
As of September 18, 2025, clinics and pharmacies with remaining supplies of mefloquine should prioritise travellers with imminent travel for whom mefloquine is the first choice of antimalarial. This includes pregnant travellers visiting high-risk malaria regions such as Sub-Saharan Africa.
The UK Malaria Expert Advisory Group's Malaria prevention guidelines for travellers from the UK provides detailed advice and guidance for health professionals advising travellers, and is the first port of call for queries.
As of September 26, 2025, this antimalarial shortage has not impacted travel clinics and pharmacies in the United States.

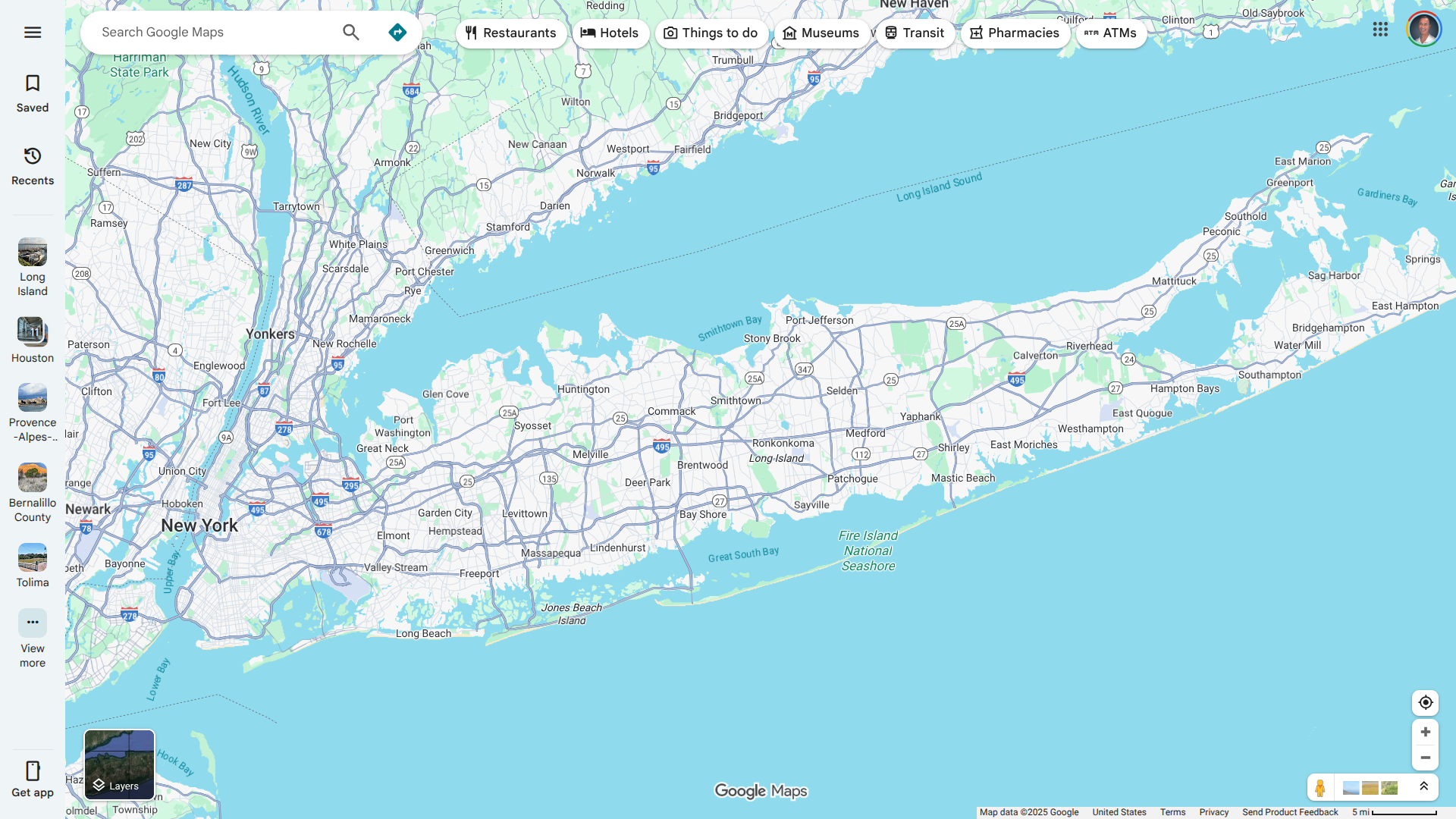
In August 2025, the New York State Health Department reported a small number of travel-associated Chikungunya Fever cases diagnosed in international travelers to countries such as France, with no identified local mosquito-borne transmission.
New York advised healthcare providers on procedures for testing and reporting suspected cases of Chikungunya.
In related news, a Long Island resident recently tested positive for Chikungunya, marking what could be the first locally acquired case ever reported in New York state.
NY residents are encouraged to take preventive measures, such as avoiding mosquito bites, and to consult their healthcare provider before traveling to areas with a high risk of mosquito-borne diseases, which include dengue, malaria, and Zika.
On September 25, 2025, local media reported that Aedes aegypti mosquitoes, the primary ones responsible for Chikungunya virus transmission, are not naturally found in New York.
Currently, approved Chikungunya vaccination services are offered at travel clinics and pharmacies in New York.