Search API
While Lyme borreliosis (LB) is Europe's most common tick-borne disease, the northeastern region has reported the most cases.
According to recent research, among all LB surveillance systems in Europe and considering any case definition for the most recently available years, national LB incidences were highest in Estonia, Lithuania, Slovenia, and Switzerland (>100 cases/100,000 PPY), followed by France, Poland, Finland, and Latvia.
Local media reported that the Baltic region's Republic of Lithuania recorded 15,254 cases of Lyme disease last year, a 500% increase from 2022.
On April 11, 2025, LRT reported that this increase is more likely to be tied to changes in reporting methods and diagnostic practices than to an increase in infected ticks.
"Since last year, we've been receiving disease registration data directly from an electronic system.... not just from health care providers."
Furthermore, previous LB infection does not confer immunity, which means a person can be reinfected multiple times.
Unlike tick-borne encephalitis, no vaccine for Lyme disease is currently available in the United States, where most cases are reported in the northeastern states, such as Pennsylvania.
However, an innovative Lyme disease vaccine candidate is conducting clinical research in 2025.
The Federal Republic of Nigeria is reported to have the highest malaria burden in the world, accounting for 39.3% of global malaria deaths in children under five years in 2023.
According to recent reporting by GAVI, while the country’s annual malaria death toll has declined over the past five years, the case count has risen, with 1.4 million more malaria infections reported in 2023 than in 2022.
Bordering both Benin and Niger in Nigeria’s northwest, the Kebbi state has the highest malaria prevalence in the country at 49% of young children and the highest mortality rate.
The state’s high malaria prevalence has been linked to several factors, including rice cultivation.
Since rice farming requires stagnant water, it is a perfect breeding ground for virus-carrying mosquitoes.
Ahmad Muhammad Sani, a public health expert in Kebbi State, told GAVI on April 7, 2025, that he believes the malaria vaccine will help significantly lower malaria morbidity and mortality, especially when combined with existing preventive measures like the use of insecticide-treated mosquito nets and indoor insecticide spraying.
Sani also encouraged parents to complete the four vaccine doses to protect children against malaria outbreaks.
“Some possible challenges relating to the vaccine effectiveness in this region include factors like high malaria transmission rates. Hence, full vaccination coverage is crucial. Parents should be aware that incomplete vaccine doses offer partial protection,” he said.
As of April 14, 2025, most malaria cases in the United States are travel-related. Two malaria vaccines are offered in Africa but are unavailable in the U.S.
Last summer, the Pan American Health Organization issued several epidemiological alerts about Oropouche cases, including deaths, in the Americas. Unfortunately, these outbreaks continue today.
To notify international travelers, the U.S. Centers for Disease Control and Prevention (CDC) recently updated its Travel Health Advisory for Oropouche fever outbreaks in several countries across the Region of the Americas.
A Level 1, Practice Usual Precautions advisory was reissued on April 9, 2025, for Barbados, Bolivia, Brazil, Colombia, Cuba, Ecuador, Guyana, Panama, Peru, and Venezuela.
Previously, a Level 2 advisory was issued for Oropouche in some regions of Brazil and Panama (Darién Province).
The CDC says Oropouche is a disease caused by the Oropouche virus and is spread primarily through the bites of infected biting midges and infected mosquitoes.
The CDC is working with other international partners to learn more about the potential risks of Oropouche during pregnancy. Additionally, healthcare providers should inform pregnant women considering travel to areas with reported Oropouche virus transmission of the possible risks to the fetus.
Furthermore, a recent publication described a patient with Oropouche who had the virus and viral RNA detected in bodily fluids, including semen.
As of April 12, 2025, no Oropouche vaccine is available.

When the U.S. Centers for Disease Control and Prevention (CDC) issued a Level 2 Travel Health Advisory regarding an outbreak of chikungunya in France's Réunion in February 2025, most public health experts did not expect an overwhelming epidemic.
As of April 12, 2025, Réunion Island has become the leading chikungunya outbreak in the world.
Since the beginning of 2025, 27,521 confirmed cases of this mosquito-transmitted disease have been reported.
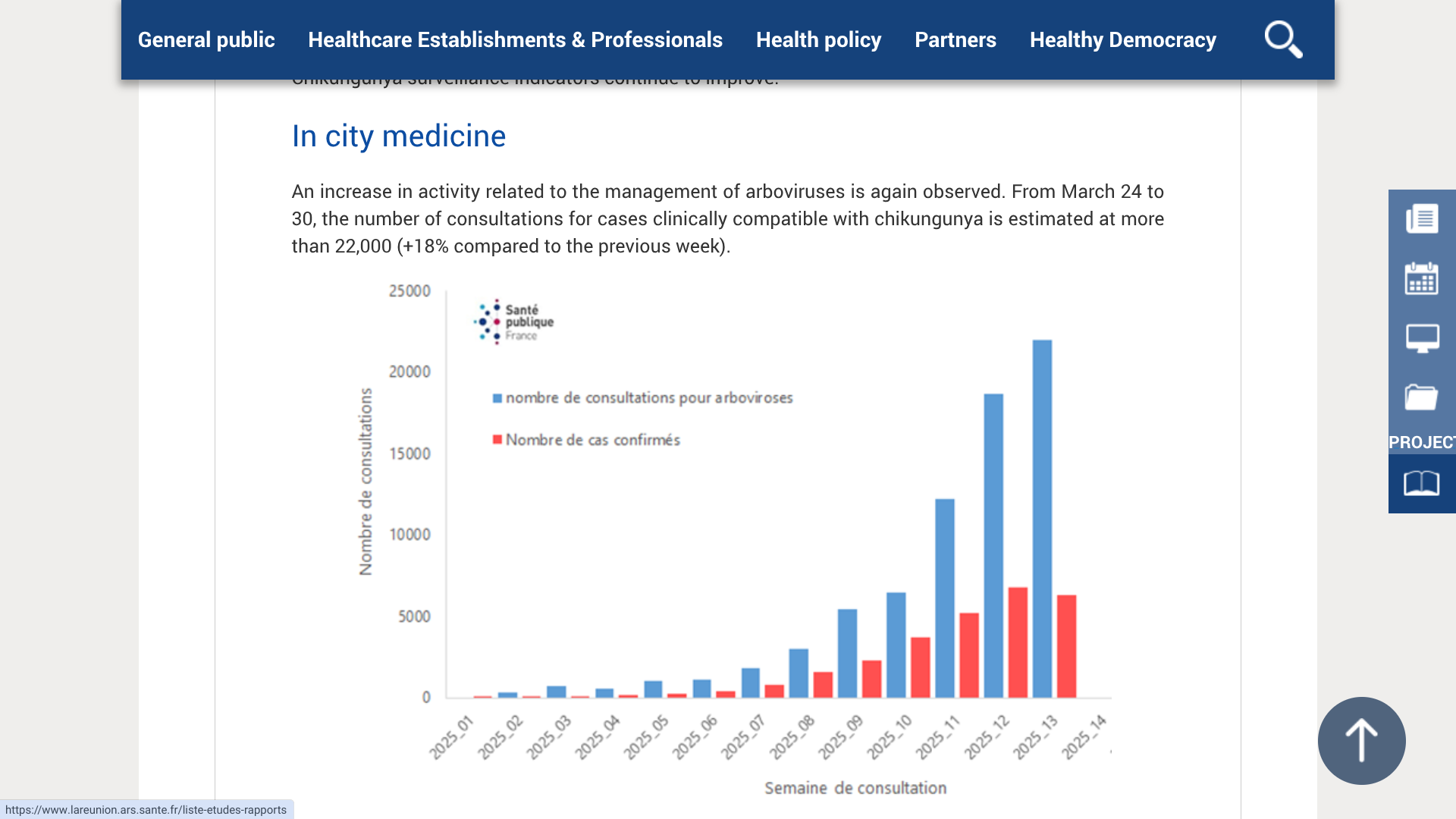
More concerning is data from ARS Réunion last week.
From March 24 to 30, 2025, there were 6,289 confirmed cases and 54 hospitalizations in Le Tampon (800 cases), Saint-Paul (900 cases), Saint-Denis (750 cases), and Saint-Pierre (600 cases).
ARS Réunion says people can protect yourself by preventing mosquito bites, or participating in a free vaccination program.
The first phase of the 40,000 vaccination campaign has been launched with the single-dose IXCHIQ® vaccine. It is available for people aged 65 and over with comorbidities and who have not previously contracted chikungunya.
Over the last few years, most chikungunya cases in the U.S. have been related to returning international travelers from tropical and subtropical regions. Diagnosing chikungunya is challenging, as people may also have been infected with dengue or Zika.
According to the U.S. CDC, vaccination against chikungunya is recommended for adults and some adolescents traveling to a destination with a current chikungunya outbreak, such as Réunion.
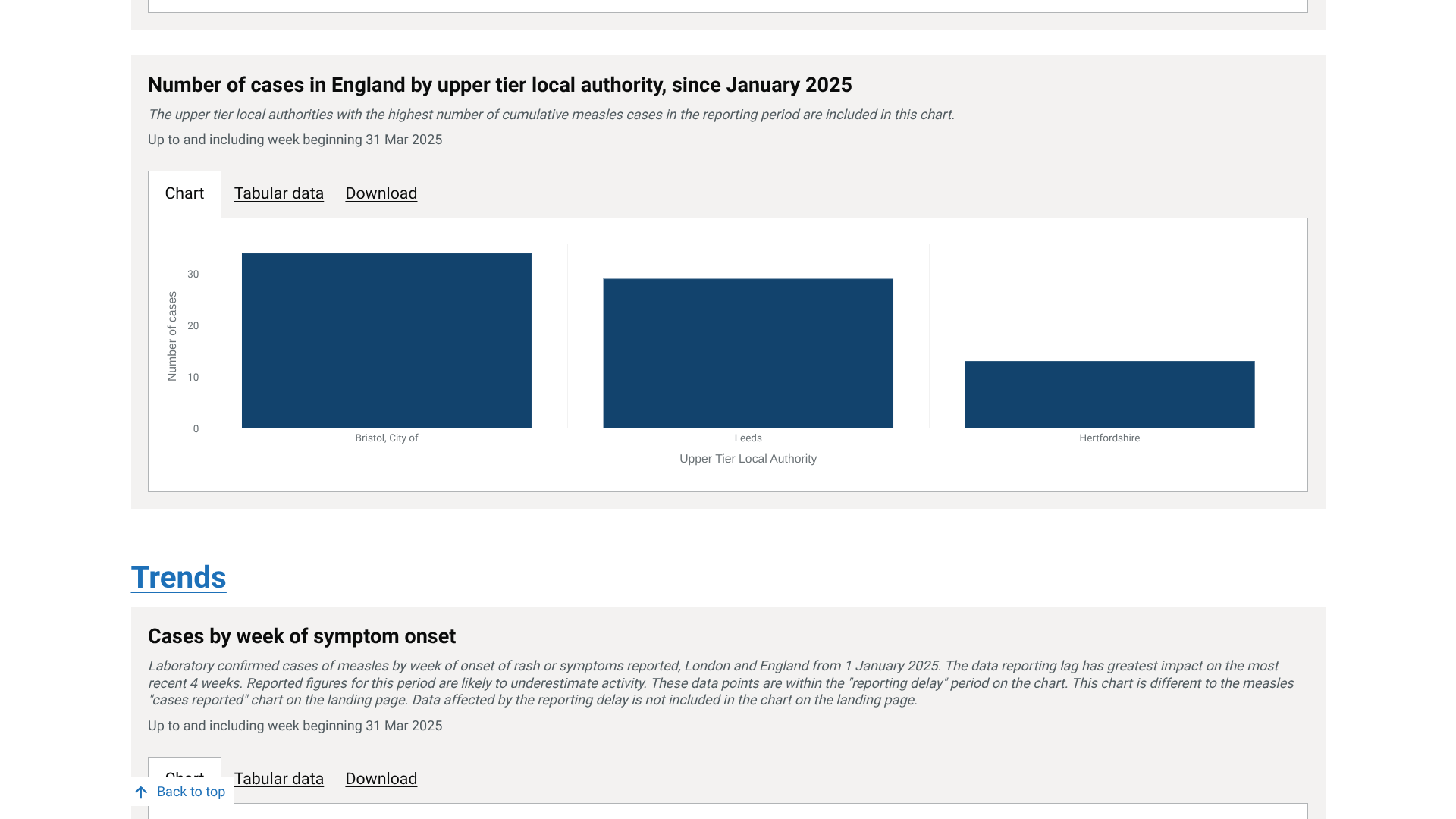
During 2024 and 2025, the UK Health Security Agency (UKHSA) reported measles outbreaks in the greater London area. This year, 213 laboratory-confirmed measles cases have been reported in England.
As of April 11, 2025, in London, 24% (52 of 213) of the measles cases have been reported, 21% in the South West, and 17% in Yorkshire and Humber.
However, recently, 57 out of 152 upper-tier local authorities have reported at least one confirmed case with symptom onset since the start of January 2025, with the highest numbers reported in Bristol, Leeds, and Hertfordshire.
The positive news from the UKHSA is that no acute measles-related deaths have been reported in 2025.
In 2024, there were 2,911 laboratory-confirmed measles cases in England, the highest number of cases recorded annually since 2012. This was initially driven by an outbreak in Birmingham but was soon overtaken by a large outbreak in London, with small clusters in other regions.
Since measles is a vaccine-preventable disease, in the UK, children receive two doses of the combined measles, mumps, and rubella vaccine as part of the routine childhood immunisation schedule.
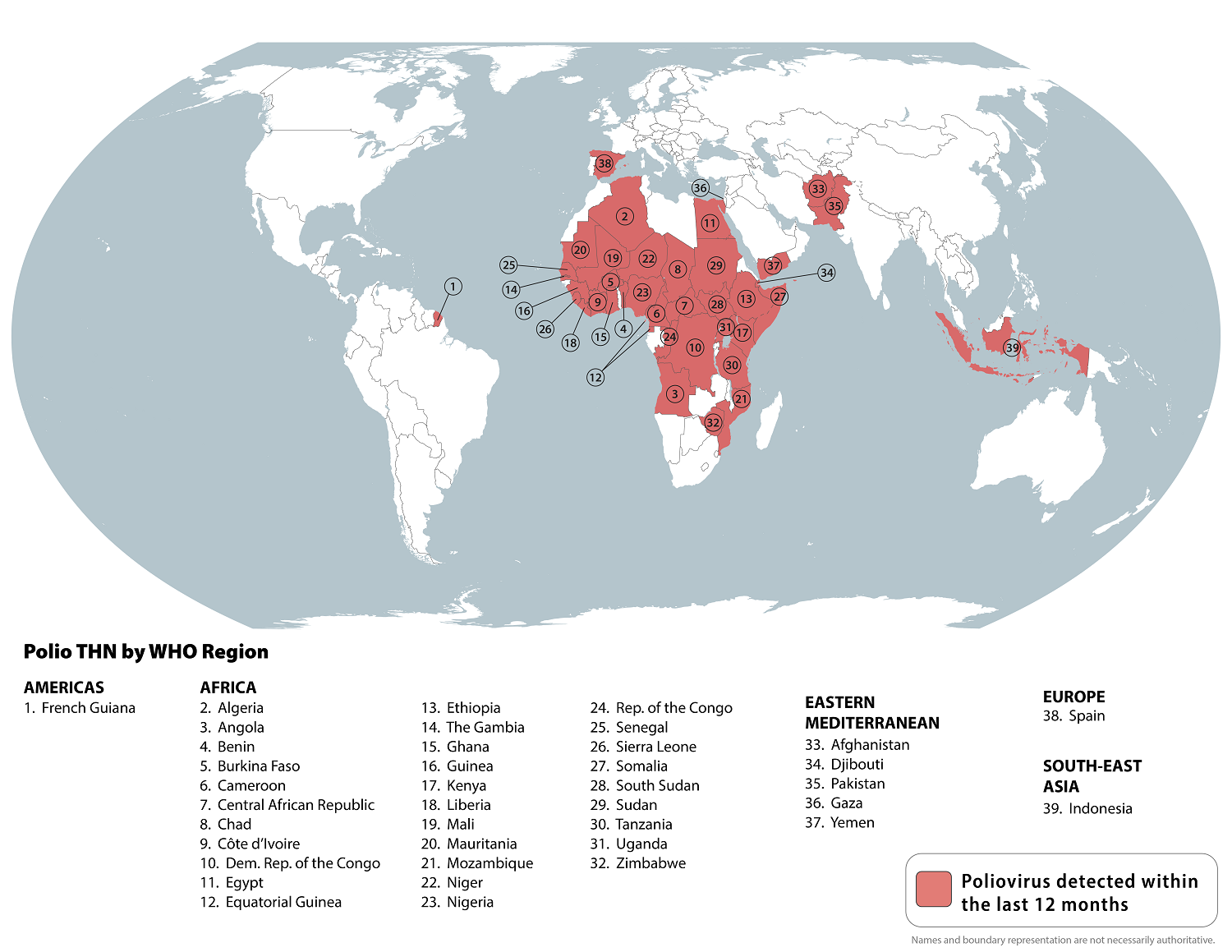
A World Health Organization committee recently agreed that the risk of international spread of poliovirus continues to constitute a Public Health Emergency of International Concern.
During the 41st meeting of the Emergency Committee under the International Health Regulations, the Committee members unanimously recommended extending the Temporary Recommendations three months into July 2025.
On April 9, 2025, the WHO Director-General accepted the Committee’s assessment.
The Committee also called on national governments to prioritize polio eradication in their domestic funding allocations to ensure sustained progress toward eradication and appreciates the Kingdom of Saudi Arabia’s recent confirmation of its $500 million commitment to global polio eradication.
Over the last three years, the nOPV2 polio vaccine has been administered about 1.1 billion times worldwide in various countries.
As of April 11, 2025, the U.S. CDC maintains a Global Measles Outbreak Travel Health Advisory that identifies 39 countries at risk for the spread of poliovirus.
In 2022, the United States was added to the list of polio-identified countries.
To reduce this significant health risk, the CDC says children and adults should be current on their routine polio vaccines, and that certain adult travelers visiting outbreak areas may get an inactivated polio vaccine (IPV) booster dose.
In the United States, IPV vaccination services are offered at travel clinics and pharmacies in 2025.
Over the years, meningococcal disease has remained a global public health concern, particularly in mass gatherings such as the Hajj and Umrah.
As of March 2025, the Kingdom of Saudi Arabia (KSA) health authorities estimated that only 54% of international Umrah pilgrims had complied with the meningococcal vaccination requirements.
Umrah is a year-round pilgrimage to Mecca in western Saudi Arabia, attended by millions of people.
According to the World Health Organization (WHO) DON563, the International Health Regulations (IHR) National Focal Point (NFP) for the KSA reported 11 cases of invasive meningococcal disease (IMD) as of March 13, 2025.
Additionally, between early February and March 18, 2025, the WHO Eastern Mediterranean Regional IHR contact point received reports of six isolated cases of IMD.
These cases involve individuals who had recently returned from Umrah.
The significant number of pilgrims traveling to KSA from countries with varying levels of meningococcal disease incidence presents a risk of international spread during these gatherings.
Given the recent notification of these cases linked to Umrah, WHO strongly advises all individuals planning to attend mass gatherings such as Hajj and Umrah to receive vaccination against meningococcal disease at least ten days before travel.
The government of Saudi Arabia regularly issues health requirements for the Hajj and Umrah, including vaccination policies. Based on the information available for the current event, the WHO does not recommend any restriction on travel and/or trade to the KSA.
In addition to meningococcal, the U.S. CDC recommends that visitors to the KSA in April 2025 consider routine and travel vaccinations such as measles and yellow fever, available at travel clinics and pharmacies.
The New York State Department of Health recently issued a travel advisory for all New Yorkers, urging them to ensure they are fully vaccinated against measles before international travel or travel to an area in the U.S. experiencing an outbreak.
New York's advisory, published on April 2, 2025, listed Canada among the countries with increased measles cases.
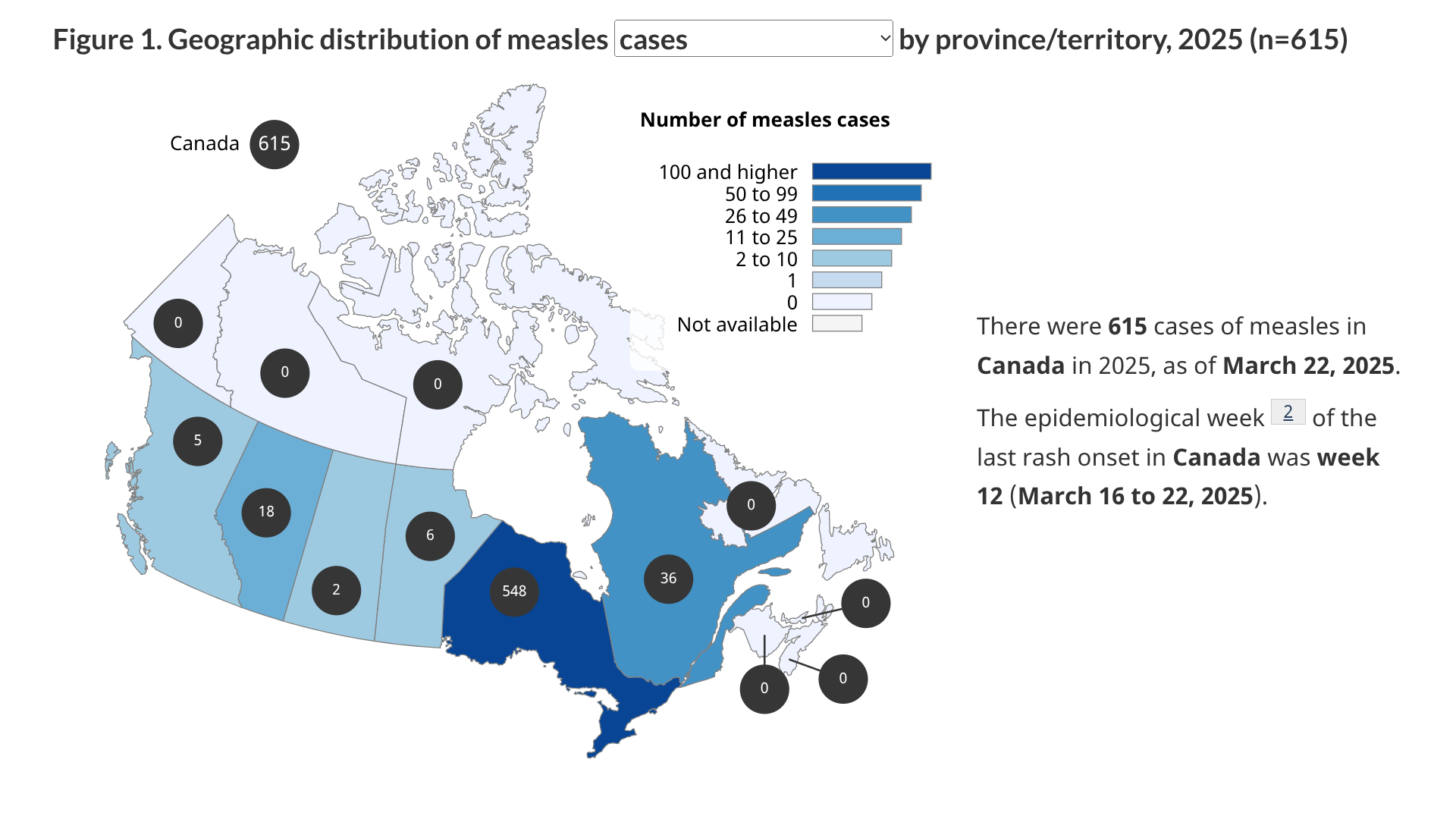
As of March 22, 2025, six jurisdictions (Alberta, British Columbia, Manitoba, Ontario (548), Quebec, Saskatchewan) in Canada had reported 615 measles cases.
"Measles is more common in different places, and exposure during travel is something we need to consider. It's important that New Yorkers ensure they are up-to-date regarding being immunized against measles. In some cases, measles is as close as a car ride away," State Health Commissioner Dr. James McDonald said in a press release.
"Measles can be a serious disease. It is not just a rash; it can cause pneumonia, hospitalization, and even death. Protect yourself and your family against measles and ensure you are up-to-date on immunization with the measles, mumps, and rubella (MMR) vaccine."
Currently, MMR vaccines are offered at clinics and pharmacies in the United States.
As of April 11, 2025, the U.S. CDC maintains a global Travel Health Advisory that lists various countries impacted by the ongoing measles outbreak.
While the South Indian Ocean chikungunya outbreak has been focused on France's Réunion Island, the Republic of Mauritius has also reported imported and local cases in 2025.
According to the Mauritius health services, most mosquito-transmitted chikungunya cases were imported from Asia and Africa.
On March 17, 2025, Mauritius, located east of Africa and Madagascar, reported the first local case in the country since 2009.
Then, on April 8, 2025, the World Health Organization (WHO) reported 17 local chikungunya cases in Mauritius.
The WHO says virus transmission persists in populations with low prior exposure, making vaccines essential to a comprehensive chikungunya outbreak response.
As of April 10, 2025, the U.S. CDC has not issued a Travel Health Notice regarding this chikungunya outbreak.
For travelers departing from the United States, the United Kingdom, or Europe, effective chikungunya vaccines, such as IXCHIQ®, have been approved by government agencies and are commercially available at most travel clinics and pharmacies.