Search API
Ultimovacs ASA today announced the results from a phase 2 clinical trial for second-line treatment in patients with malignant mesothelioma.
The data presented as a late-breaking abstract at the ESMO Congress shows that Ultimovacs' cancer vaccine UV1, in combination with ipilimumab and nivolumab, demonstrated a statistically significant and clinically meaningful improvement of overall survival versus ipilimumab and nivolumab alone, a key secondary endpoint.
The UV1 cancer vaccination combined with ipilimumab and nivolumab reduced the risk of death by 27%.
"For patients with malignant mesothelioma, few treatment options are available after first-line chemotherapy. The NIPU study showed that patients receiving UV1 vaccination as an add-on to nivolumab and ipilimumab experienced an increased objective response rate and a clinically meaningful prolonged survival."
"These encouraging results provide a foundation for advancing further clinical development with UV1 vaccination in mesothelioma patients," said Principal Investigator of the NIPU clinical trial, Professor Åslaug Helland, MD Ph.D., in a press release on October 18, 2023.
UV1 is a therapeutic cancer vaccine that generates an immune response against the human telomerase enzyme.
The enzyme is essential for the ability of cancer cells to proliferate. Telomerase is present in 85-90% of all cancers across the stages of the disease. The vaccine is manufactured as an off-the-shelf product with a long shelf life. UV1 is easy to use and does not require sophisticated hospital infrastructure.
The results showed that UV1 plus ipilimumab and nivolumab improved overall survival (OS), reducing the risk of death by 27% (HR=0.73 [80% CI, 0.53-1.00]). The median OS was 15.4 months (95% CI, 11.1-22.6) for UV1 plus ipilimumab and nivolumab (treatment arm) versus 11.1 months (95% CI, 8.8-18.1) for ipilimumab and nivolumab alone (control arm), with a median observation time of 17.3 months. This degree of improvement met the protocol's predefined threshold for statistical significance.
The data further demonstrated a benefit in terms of objective response rate, as determined by a blinded independent central review. In the UV1 arm, 31% of the patients experienced an objective response compared to 16% in the control arm (odds ratio 2.44 [80% CI, 1.35-4.49]).
The safety profile of the combination of UV1 plus ipilimumab and nivolumab observed in the trial was consistent with the safety profile of ipilimumab and nivolumab alone, confirming the good safety profile for UV1.
The patients will continue to be monitored for efficacy and safety endpoints over the next years.
Malignant mesothelioma is an aggressive, complex form of cancer with a high mortality rate and few therapeutic options. Patients affected have often been occupationally or environmentally exposed to asbestos. Several efforts have been made in the last decades to improve the survival outcomes of patients with mesothelioma.
There is currently no established standard of care in second-line treatment.
In October 2023, Ultimovacs announced that the U.S. FDA had granted Orphan Drug Designation for UV1 to treat mesothelioma (based on the NIPU data from June 2023).
Ultimovacs is evaluating the universal cancer vaccine UV1 in a broad clinical development program across various cancer indications with different biologies and disease stages, combined with different checkpoint inhibitors.
The title of the late-breaking ESMO abstract is "LBA99 First survival data from the NIPU trial; A randomized, open-label, phase II study evaluating nivolumab and ipilimumab combined with UV1 vaccination as second-line treatment in patients with malignant mesothelioma."
Oslo University Hospital sponsors the NIPU study with support from Bristol-Myers Squibb and Ultimovacs.
An innovator of novel immunotherapies has partnered with one of the largest cancer research in evaluating a CAR T therapy for HIV in an early-stage clinical trial so that one day, more people with Human Immunodeficiency Virus might achieve long-term remission.
Helocyte, Inc. today announced that it executed an exclusive option agreement with the City of Hope for patent rights to use Triplex, a cytomegalovirus (CMV) vaccine, in combination with cytomegalovirus-specific, Anti-Human Immunodeficiency Virus ("HIV") Chimeric Antigen Receptor ("CAR") (collectively, CMV/HIV-CAR) T Cells for the treatment of adults living with HIV.
Additionally, the California Institute for Regenerative Medicine recently awarded a $11.3 million grant to the City of Hope to fund a Phase 1 clinical trial that is expected to enroll up to 12 healthy individuals living with HIV-1 on stable anti-retroviral therapy ("ART") who have maintained viral suppression for at least 48 weeks.
The study will include three dose-escalating cohorts, along with an expansion cohort. Other cohorts will include further vaccination of subjects with Triplex to drive the continued proliferation of the CAR.
Triplex is a universal (non-HLA-restricted) recombinant Modified Vaccinia Ankara viral vector vaccine engineered to induce a robust and durable virus-specific T cell response to three immuno-dominant proteins [UL83 (pp65), UL123 (IE1), UL122 (IE2)] linked to CMV complications in the post-transplant setting.
Triplex was initially developed by the City of Hope and exclusively licensed to Helocyte in 2015.
"City of Hope made a major advancement when our transplant team helped a patient achieve remission for both HIV and leukemia," commented John A. Zaia, M.D., the Aaron D. Miller and Edith Miller Chair for Gene Therapy at City of Hope, in a press release on October 16, 2023.
The clinical study will build upon preclinical data published in Molecular Therapy - Methods & Clinical Development in April 2022, demonstrating the potential efficacy of combining a CMV vaccine and CMV/HIV CAR T cell therapy to eradicate HIV.
The study illustrated the potential long-term durability of the combination therapy, which induced therapeutic immune cells to take hold in bone marrow.
This approach aims to target and eradicate latent viral T cell reservoirs in immune cells to achieve complete HIV clearance.
To date, the engineering of T cells to express HIV-specific CAR T cells has failed to demonstrate meaningful clinical benefits. This is believed to be partly due to the effectiveness of highly active ART, which reduces HIV viral load to a level that prevents the activation of CAR T cells.
The use of Triplex is believed to stimulate CMV/HIV-CAR T cells to proliferate within patients' bodies.
In the preclinical study, CAR T cells were engineered to target and kill cells tagged with a particular protein called gp120, expressed in all HIV viruses, frequently with mutations that cause the virus to evade natural immunity without affecting healthy cells.
Lindsay A. Rosenwald, M.D., Fortress' Chairman and Chief Executive Officer and Chairman of Helocyte, Inc., added, "We look forward to building upon the data that continue to be generated relating to the use of Triplex in the treatment of HIV, including an ongoing Phase 2 clinical trial evaluating the safety and efficacy of Triplex in eliciting a CMV-specific immune response and reducing CMV replication in adults co-infected with HIV and CMV."
Helocyte, Inc., a subsidiary company of Fortress Biotech, Inc. For additional information regarding the grant, please see https://www.cirm.ca.gov/our-progress/awards/evaluation-safety-and-feasib....
As of October 16, 2023, there are no approved HIV prevention vaccines in the U.S.

The U.S. Department of Health and Human Services (HHS) today confirmed the selection of initial next-generation vaccine candidates and more than $500 million in awards for Project NextGen.
Announced on October 13, 2023, the three next-generation vaccine selections are distinct, targeting stronger, broader, or longer-lasting immune responses.
Intranasal vaccines have the potential to stop viruses at the site of infection, and self-amplifying mRNA and additional antigens may generate a stronger immune response than current vaccine technologies.
The awards announced today will support companies as they prepare their vaccine candidates for Phase 2b clinical evaluation:
$8.5 million to CastleVax for a vector-based intranasal vaccine candidate,
$10 million to Codagenix for a live-attenuated intranasal vaccine candidate,
$10 million to Gritstone Bio for a self-amplifying mRNA vaccine candidate.
“The vaccine selections and funding announced today are important steps forward for Project NextGen – with vaccine and therapeutics candidates moving quickly to clinical trials that will start in the coming months,” said Assistant Secretary for Preparedness and Response Dawn O’Connell in a press release.
To support these and all future Project NextGen clinical studies, the U.S. Biomedical Advanced Research and Development Authority (BARDA) awarded over $240 million, including investments in cold-chain sample management, genomic sequencing, and increased central laboratory capacity for sample testing.
Finally, BARDA is awarding over $241 million to support new technologies to improve national preparedness for future COVID-19 outbreaks and patient access. These technologies have the potential to enable shorter development timelines for monoclonal antibodies through mRNA, increased efficiency in virus testing, and alternate routes for vaccine administration:
The over $500 million announced today builds on the over $1.4 billion awarded in August – accelerating products toward clinical trials and potential commercial availability.
To view the complete list of awards and learn more about Project NextGen, please visit medicalcountermeasures.gov/nextgen/.

A glioblastoma vaccine therapy candidate has been granted Fast Track Designation (FTD) by the United States Food and Drug Administration (FDA).
Announced on October 12, 2023, MimiVax Inc.'s SurVaxM vaccine (immunotherapy) is being studied to treat newly diagnosed glioblastoma (nGBM).
Glioblastoma is a rare disease with great unmet medical need.
SurVaxM is a first-in-class, patented peptide mimic immunogen that targets survivin, a cell-survival protein present in 95% of glioblastomas and in many other cancers.
SurVaxM stimulates a patient’s immune response to control tumor growth and prevents disease recurrence. Because survivin is present in most cancers, SurVaxM could potentially have applicability in other cancers.
"The receipt of FTD affirms the importance of new clinical developments of novel therapies to improve the treatment and outcomes for patients with newly diagnosed glioblastoma," said Michael Ciesielski, CEO of MimiVax, in a press release.
"This designation is a key component in our journey to help patients with glioblastoma to live longer."
A randomized, blinded, placebo-controlled Phase 2b clinical trial of SurVaxM for nGBM (SURVIVE) [NCT05163080] is now recruiting at 11 cancer centers across the U.S.
Previously, positive Final Data from the previous Phase 2a Study of SurVaxM for nGBM, published in the Journal of Clinical Oncology, found that 51% of patients receiving SurVaxM survived at least two years, and 41% survived at least three years.
The median Overall Survival of 25.9 months with nGBM in this study is considerably higher than expected with standard therapy alone.

LimmaTech Biologics AG announced today the closing of a USD 37 million Series A financing round that will empower its proprietary technology platform and accelerate its preclinical and clinical vaccine candidates against increasingly dangerous bacterial infections, including programs addressing shigellosis and gonorrhea.
Antimicrobial Resistance is responsible for approximately 5 million deaths annually. Infections that were once easily treatable have now become difficult, if not impossible, to cure.
As a leading example of this threat to global health, half of the approximately 700,000 annual gonorrhea infections in the U.S. are already resistant to antibiotics, and there is a real threat of gonorrhea soon becoming untreatable.
While there are no gonorrhea vaccines available, off-label vaccines and treatments are in use.
Later-stage clinical development efforts will focus on the company's Shigella vaccine program, which LimmaTech developed with GSK. The company expects to announce preliminary results from the Shigella program's ongoing Phase 2 clinical trial in the second half of 2023.
Shigella cause an estimated 450,000 infections in the U.S. each year.
According to the U.S. CDC, people can get a Shigella infection (shigellosis) after putting something in their mouth or swallowing something that has come into contact with the stool of someone with a Shigella infection.
"Within the next decade, multiple bacterial infections will become untreatable due to antimicrobial Resistance, which is already a significant burden on global health. By advancing our innovative technology platform, LimmaTech has the potential to simultaneously provide vaccine-induced protection against bacterial infections, mitigate the increasing risk of antibiotic resistance, and move toward the control of several highly transmissible pathogens," commented Dr. Franz-Werner Haas, CEO of LimmaTech, in a press release on October 9, 2023.
".....With this support and our team of proven experts in bacterial vaccine development and manufacturing, we look forward to providing life-changing vaccines to address a major global medical need."
The Company is conducting a Phase I/II clinical trial in the Republic of Kenya of a 4-valent candidate vaccine to help prevent diarrheal disease caused by the Shigella bacteria in children and infants in low and middle-income regions. The Shigella study is conducted in collaboration with GSK and the Wellcome Trust.
LimmaTech is committed to translating novel scientific concepts into highly effective vaccines that benefit humanity. For more information, please visit www.lmtbio.com.

Two world-class pharmaceutical companies announced an agreement for a potential first-in-class vaccine against extraintestinal pathogenic E. coli.
On October 3, 2023, France-based Sanofi confirmed it has agreed with Janssen Pharmaceuticals, Inc., a Johnson & Johnson company, to develop and commercialize a 9-valent vaccine candidate for extraintestinal pathogenic E. coli currently in Phase 3 study.
The agreement combines Janssen's robust science behind this potential first-in-class product, Sanofi's worldwide manufacturing footprint, and the recognized world-class expertise of these companies in launching innovative vaccines.
This is important news since Extraintestinal pathogenic E. coli is a leading cause of sepsis, particularly in older adults, with an approved vaccine available in 2023.
Sepsis is a life-threatening bloodstream infection accompanied by severe illness and widespread organ damage generated by the body's self-destructive response to the infection.
Thomas Triomphe, Executive Vice President, Vaccines, at Sanofi, commented in a press release, "E. coli is a significant cause of sepsis, mortality, and antimicrobial resistance in older adults, and the number of cases is rising as the population ages."
"In line with our commitment to design and deliver first- or best-in-class medicines and vaccines, this agreement with Janssen aims to positively impact public health by reducing hospitalization costs and the burden on health systems associated with ExPEC and help older adults around the world to live longer healthier lives."
The ongoing Phase 3 E.mbrace clinical trial is designed to evaluate the efficacy of the 9-valent extraintestinal pathogenic E. coli vaccine (ExPEC9V) compared to placebo in preventing invasive E. coli disease caused by ExPEC9V O-serotypes.
The study was started in 2021 by Janssen and continues to enroll patients. To learn more, visit https://classic.clinicaltrials.gov/ct2/show/NCT04899336.
Under the terms of the new agreement, both companies will co-fund current and future research and development costs.
Sanofi will pay USD 175M upfront to Janssen, followed by development and commercial milestones. A profit-share arrangement will exist in the U.S., EU4 (France, Germany, Italy, Spain), and the U.K. In the rest of the world, Janssen will receive tiered royalties and sales milestones.

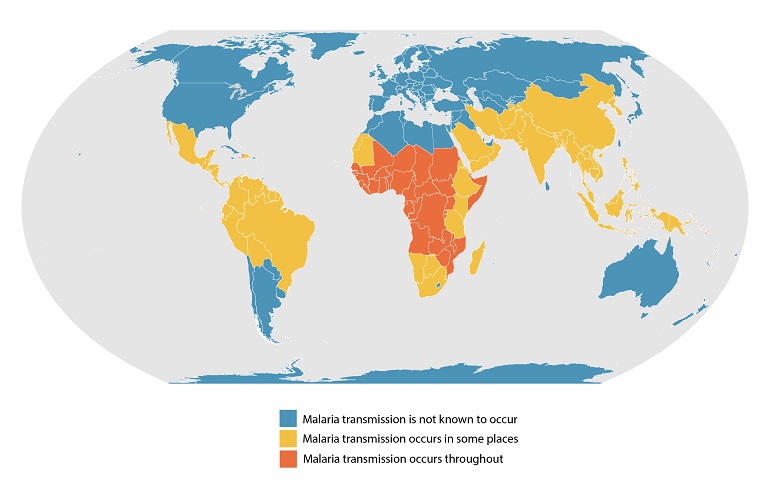
Malaria vaccines have been in development since the 1960s, with substantial progress in the last decade, says the World Health Organization (WHO). Today, the WHO announced it has recommended a second vaccine, R21/Matrix-M, for preventing malaria in children.
As of October 2023, the R21 vaccine is the second malaria vaccine recommended by WHO, following the Mosquirix™ (RTS,S/AS01) vaccine, which received a WHO recommendation in 2021.
Demand for malaria vaccines is unprecedented in 2023. However, the available supply of RTS,S is limited.
The addition of R21 to the WHO's recommended malaria vaccine list is expected to result in sufficient vaccine supply in various countries.
The following steps for R21/Matrix-M, include completing the ongoing WHO prequalification and enabling international vaccine procurement for a broader rollout in malaria outbreak countries.
The WHO's Director-General endorsed the recommendation following its regular biannual meeting on 25-29 September 2023.
"As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria. Now we have two," commented Dr Tedros Adhanom Ghebreyesus, WHO Director-General, in a press release on October 2, 2023.
"Demand for the RTS,S vaccine far exceeds supply, so this second vaccine is a vital additional tool to protect more children faster and to bring us closer to our vision of a malaria-free future."
The R21 vaccine has been shown to reduce symptomatic malaria cases by 75% during the 12 months following a 3-dose series. A fourth dose given a year after the third maintained efficacy.
This efficacy is similar to that demonstrated when RTS,S is given seasonally.
The WHO says that at US $2 – US $4 per dose, the cost-effectiveness of the R21 vaccine would be comparable with other recommended malaria interventions and other childhood vaccines.
Malaria is a disease caused by four species of protozoan parasites of the genus Plasmodium and is transmitted to people by Anopheles mosquitoes.
According to the WHO's recent World Malaria Report, the global number of malaria cases reached about 240 million, with over 600,000 related fatalities.
As of October 2023, neither malaria vaccine is available in the United States.
Without an approved Alzheimer's disease vaccine available, several bipolar disorder (BD) candidates are following U.S. Food and Drug Administration (FDA) policies to accelerate clinical research.
In the U.S., about 2.8% of the population is estimated to be affected by BD during the past year, says the U.S. NIH.
For example, Alzamend Neuro, Inc. today announced receipt of a “Study May Proceed” letter from the U.S. FDA for the initiation of study AL001-BD01, a Phase IIA clinical study of AL001 for BD type 1.
AL001 is a novel lithium-delivery system that has the potential to deliver benefits of marketed lithium salts while mitigating or avoiding currently experienced toxicities associated with lithium, a chemical entity well known for efficacy in BD type 1.
Alzamend’s goal is to revive the utility of lithium treatment by importantly improving the benefit-to-risk relationship of lithium treatment in clinical practice.
“Lithium was the first mood stabilizer approved by the FDA and is still a first-line treatment option for BD type 1,” said Stephan Jackman, Chief Executive Officer of Alzamend, in a press release on Octobe 2, 2023.
“If we are able to develop a next-generation lithium product (AL001) that would not routinely require therapeutic drug monitoring, it would constitute a major improvement over current lithium-based treatments and positively impact the seven million Americans afflicted with BD."
"We are advancing the process and expect that the first patient will be dosed in the first quarter of 2024"
Based on the favorable safety profile observed in the recently completed study and extensive safety data on the drug’s constituent components, the AL001 development program may qualify for a Section 505(b)(2) New Drug Application pathway for FDA approval, which is available to new formulations of an approved drug.
BD is a mood disorder characterized by periods of depression and periods of abnormally elevated happiness.
The condition is classified as BD Type 1 if there has been at least one manic episode, with or without depressive episodes.
And can be classified as BD Type 2 if there has been at least one hypomanic episode (but no full manic episodes) and one major depressive episode.
As of October 2023, there are several Alzheimer's disease vaccines and therapies conducting clinical trials which are seeking participants.


