Search API
The University of Oxford announced today that it has launched the world's first Phase II clinical trial of a Nipah virus vaccine candidate in Bangladesh in partnership with the International Centre for Diarrhoeal Disease Research.
This study is essential, as a vaccine is urgently needed, as the disease can be fatal in up to 75% of cases.
Funded by the Coalition for Epidemic Preparedness Innovations, this study will assess the safety and immune response of the ChAdOx1 NipahB vaccine in a region where the virus causes recurrent outbreaks.
The ChAdOx NipahB vaccine was manufactured for this clinical trial by the Serum Institute of India Pvt. Ltd., the world's largest vaccine manufacturer.
Professor Brian Angus, Professor of Medical Practice at the Nuffield Department of Medicine, University of Oxford and Chief Investigator of the trial at the Oxford Vaccine Group, commented in a press release on December 9, 2025, "Starting a Phase II trial in a country affected by regular Nipah outbreaks is a critical step in making sure this vaccine is both effective and relevant to the people who need it most."
"It's an essential part of ensuring equitable access to protection against emerging infectious diseases."
Nipah virus is a deadly disease from the same viral family as measles, the paramyxoviruses.
The World Health Organization recognises it as a research priority due to its pandemic potential. Of the 750 cases recorded since 1998, there have been 415 deaths related to this virus.
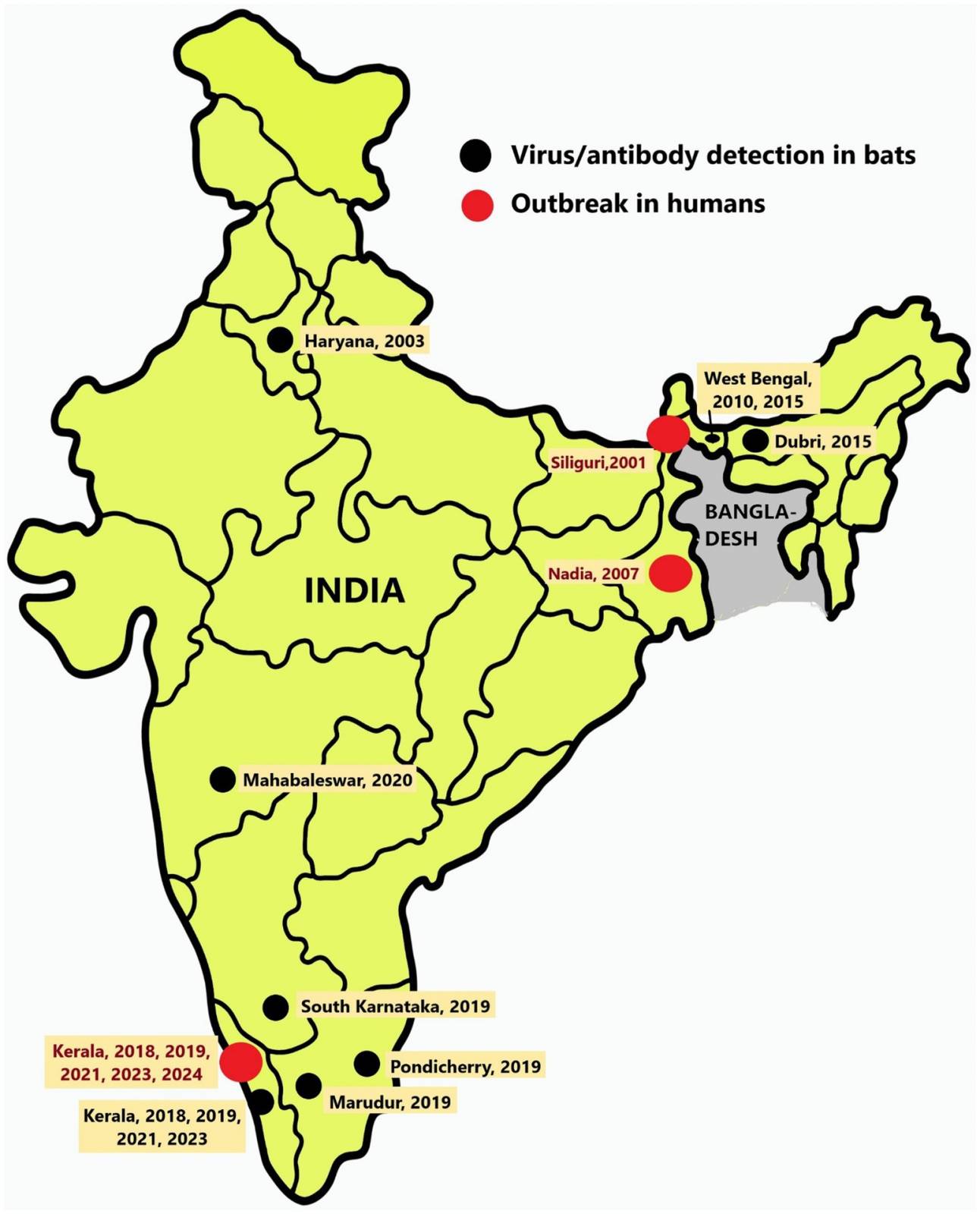
First identified after an outbreak in Malaysia, the Nipah virus causes small outbreaks in Bangladesh almost every year. In India, seven outbreaks of the Nipah virus have occurred since 2001, primarily occurring in the southern and eastern regions, according to a study published by the journal Frontiers.
The UK Health Security Agency (UKHSA) has identified an increase in the number of Shigella sonnei cases caused by a particular strain of the gastrointestinal pathogen.
Since October 2025, there has been a rise in Shigella infections in people returning to the UK from the Republic of Cape Verde. Of the 137 confirmed UK cases, most (109) reported recent travel to Cape Verde, an island country in the Atlantic Ocean off the coast of West Africa.
As of December 5, 2025, the UKHSA had initiated an outbreak investigation.
An outbreak of Shigella sonnei was also reported in Cape Verde in 2022, with cases among travellers from several European countries, including the UK.
The UKHSA says Shigella sonnei (S. sonnei) is a species of Shigella, a group of gastrointestinal bacteria that can cause severe diarrhoea, fever, and stomach cramps; rarely, it can cause sepsis in the immunocompromised.
S. sonnei is transmitted via contact with contaminated faeces either directly through person-to-person transmission or indirectly from contaminated food or water, or surfaces – infection is often linked to overseas travel to regions where shigellosis is endemic.
In 2023, there were 117 cases in England belonging to the 10 single-nucleotide polymorphism linkage cluster t10.1814.
Globally, most cases of shigellosis are in children younger than five years of age, but all ages can be affected. There is also a risk of sexual transmission among certain people.
In the United States, as of Week 43, the CDC reported about 14,000 Shigellosis cases, a significant decrease from 2024.
As of December 9, 2025, the CDC states there is no vaccine to prevent Shigella infection.
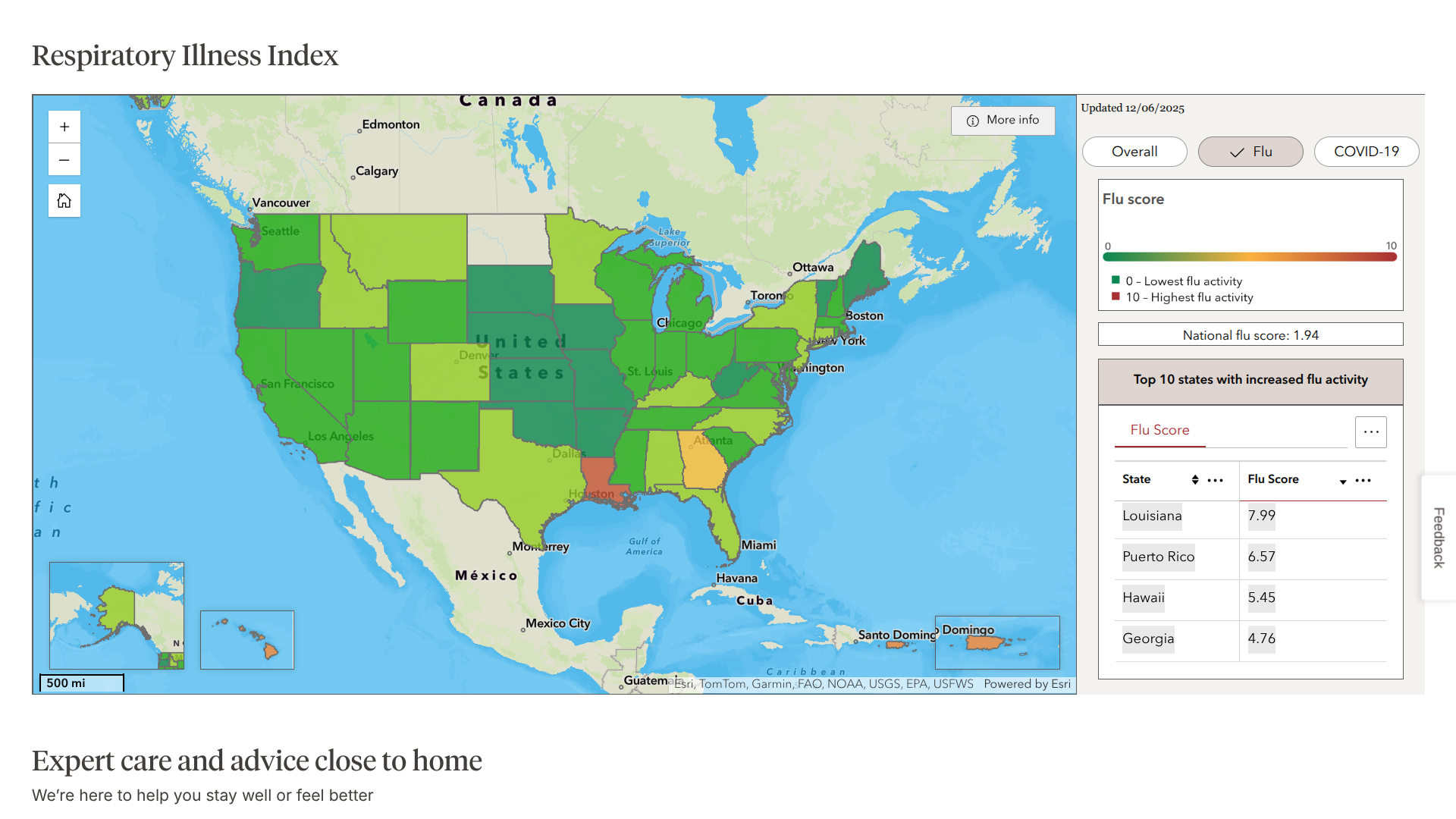
Over the past week, reports of influenza cases have been confirmed across the United States, with a few states reporting outbreaks.
According to the Walgreens Respiratory Illness Index on December 9, 2025, Louisiana, Puerto Rico, Hawaii, and Georgia are the most recent, unfortunate leaders reporting flu outbreaks.
Previously, the latest FluView published by the Centers for Disease Control and Prevention (CDC) reported that 2.9% of visits to healthcare providers in the prior week were for respiratory illnesses, up from 2.5%.
The best data from the CDC is that no influenza-associated pediatric deaths occurred during the 2025-2026 season. Last flu season, 287 pediatric deaths were reported.
With the peak influenza season fast approaching, the CDC encourages most people to get their annual vaccination as soon as possible.
The South Carolina Department of Public Health (DPH) recently announced that seven of the new measles cases being investigated are centered in Spartanburg County.
As of December 5, 2025, there are currently 281 individuals in quarantine and two in isolation in the center of South Carolina. This county is located north of Columbia, SC, and west of Charlotte, NC.
DPH says that since the outbreak began in early October 2025, some cases are travel-related or due to close contact with known cases. Other cases have no identified source, suggesting that measles is circulating in the community and could spread further.
DPH will continue to prioritize requests for MMR vaccination events, if received, and will also take steps to increase appointment availability for MMR vaccination in health department locations, should demand dictate.
MMR vaccines are also available at many primary care provider offices and pharmacies, as well as DPH Health Departments.
Additionally, the U.S. CDC maintains a Global Travel Health Notice regarding measles outbreaks in numerious countries. The CDC recommends that before traveling abroad in December 2025, you ensure you and your family are fully immunized against the contagious virus.
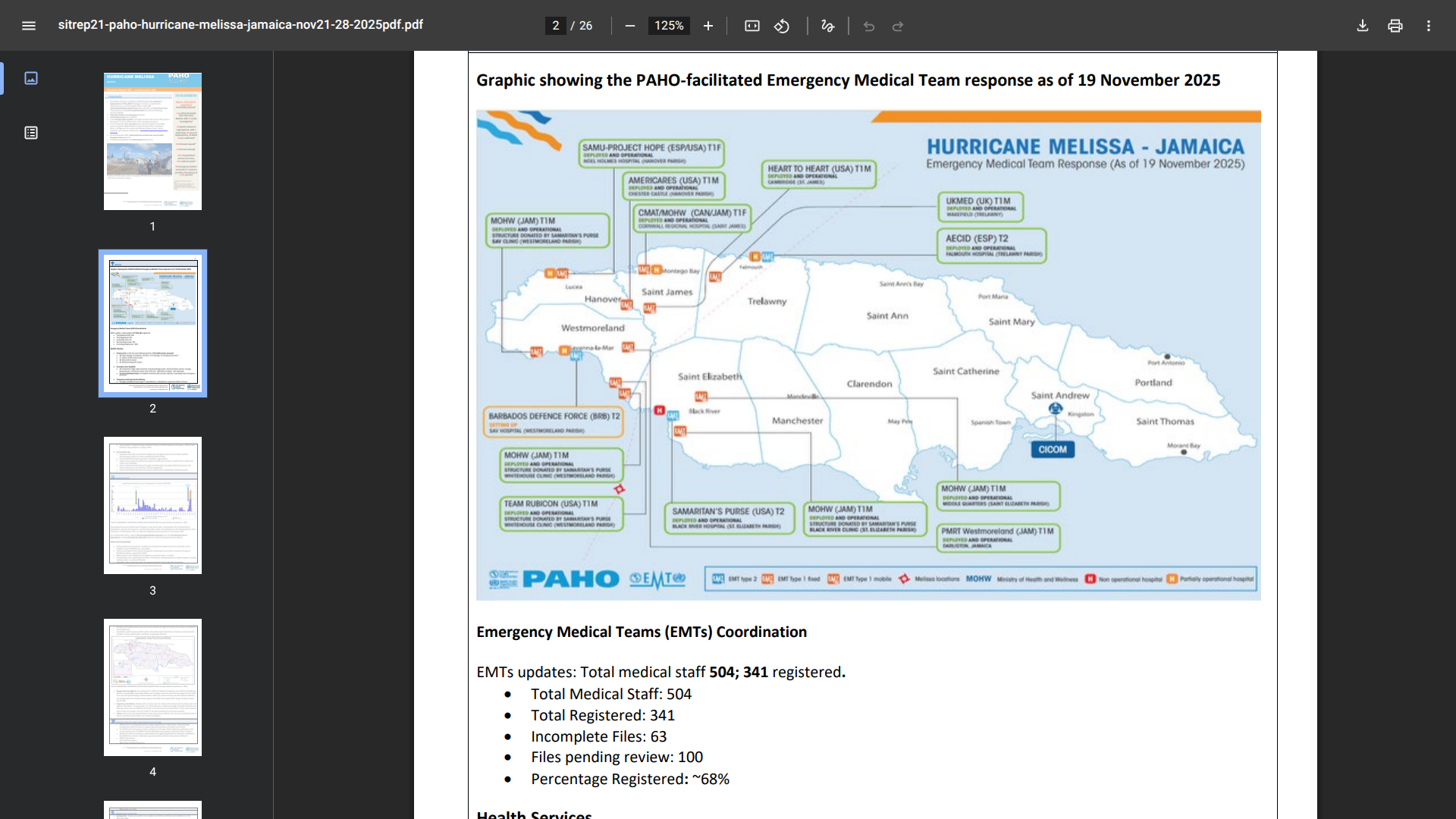
After Hurricane Melissa struck in late October 2025, Jamaica's Ministry of Health declared a health emergency across the island regarding leptospirosis (Weil's disease).
The passage of Hurricane Melissa led to flooding in many communities, increasing the risk of leptospirosis transmission. By early December 2025, the ministry reported (#36) 71 suspected, probable, or confirmed leptospirosis cases following the hurricane.
Among these cases, seven fatalities have been confirmed as related to leptospirosis.
Local media reported on December 5, 2025, that the ministry is monitoring the ongoing outbreak in St James (15 cases), St Ann (12), and St Elizabeth (8).
Dr. Ciro Ugarte, PAHO Health Emergencies director, recently stated in a press release, "Our priority is to ensure that communities have access to safe, quality health care while remaining vigilant to rapidly detect and respond to health threats that linger in the aftermath of the hurricane."
Additionally, Jamaica's National Surveillance Unit, Ministry of Health and Wellness, had recorded 452 suspected/probable cases of dengue and two suspected dengue-related deaths in 2025.
While the U.S. CDC has not issued a Travel Health Notice as of December 8, 2025, the UK's the Foreign, Commonwealth & Development Office says there is no vaccination or medication to prevent leptospirosis.
And when departing from the U.S., the second-generation dengue vaccine is currently unavailable.

Hong Kong's chikungunya fever (CF) outbreak continues to include both travel-related and locally acquired cases in 2025.
Today, the Hong Kong Centre for Health Protection (CHP) of the Department of Health reported that there have now been 10 local CF cases and 68 cases among travelers.
The CHP wrote on December 7, 2025, that some confirmed CF cases had reportedly been bitten by mosquitoes while hiking along the Tsing Yi Nature Trails, a higher-risk area.
The CHP continued to urge individuals who have recently visited the Tsing Yi North area or hiked along the Tsing Yi Nature Trails to seek medical attention as soon as possible if they develop relevant symptoms and to call the enquiry hotline (Tel: 2125 2373).
The CHP continued to urge the members of the public residing and working at Queen's Road West (near Morrison Street and Hollywood Road) who experienced a fever, rash, or joint pain on or after November 15, 2025, to seek medical advice or contact the CHP immediately.
This area is located northwestern of the inner city and east of Hong Kong Disneyland.
CHP officers continued to reach out to individuals in the locations above, reminding them to be aware of relevant symptoms and to maintain good household hygiene.
To alert international travelers to at-risk areas, the U.S. CDC issued Travel Health Notices in 2025.
As of December 5, 2025, the CDC added Bangladesh and Sri Lanka to the Level 2 notice list.
In the Region of the Americas, over 289,000 CF cases and 141 related fatalities have been reported this year. The majority of these cases have been confirmed in Bolivia, Brazil, and Cuba.
The CDC writes 'You can protect yourself by preventing mosquito bites, which includes using insect repellent. Vaccination is recommended for travelers visiting any area with a CF outbreak in 2025.'
In the United States, chikungunya vaccination services are offered at travel clinics and pharmacies.
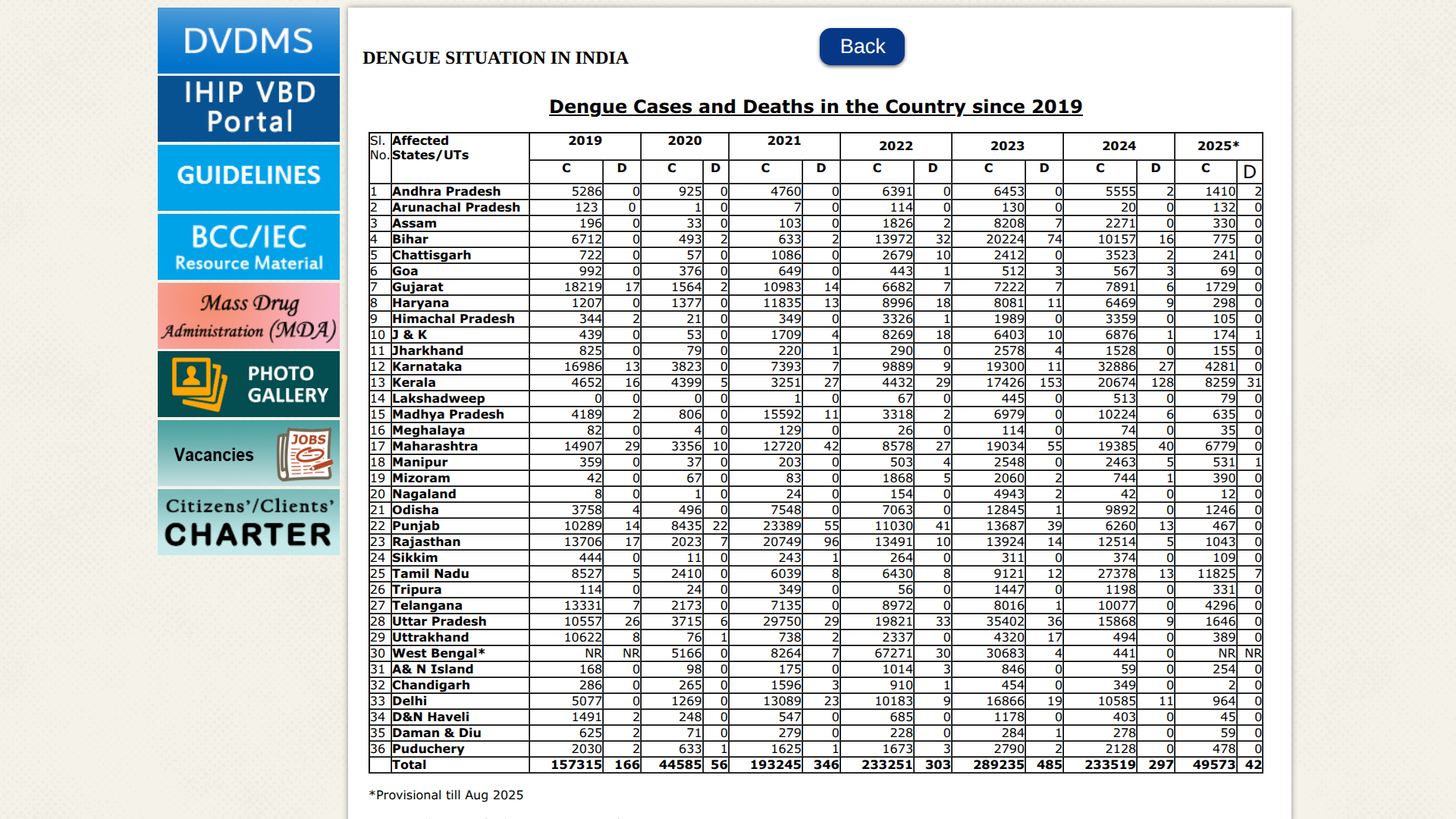
Throughout 2025, India has reported an increase in dengue cases across most regions. With the new year fast approaching, the National Centre for Vector Borne Disease Control (NCVBDC) data indicates a difficult season for this mosquito-transmitted disease in 2026.
The NCVBDC data indicate that, in October 2025, a total of 22,659 dengue cases were reported in India, a 21% increase compared to September 2025 (18,803). Tamil Nadu is the unfortunate leader in 2025.
And as of December 2025, over 49,000 dengue cases had been reported.
When the U.S. CDC last updated its Level 1 - Practice Usual Precautions, the Global Travel Health Notice focused on dengue outbreaks; it did not include a warning for India. However, the CDC says Travelers visiting dengue outbreak countries may be at increased risk in 2025.
Furthermore, the CDC has identified a higher-than-expected number of dengue cases among U.S. travelers returning from those countries, including those arriving in Florida.
While the CDC does not recommend the second-generation dengue vaccine known as Qdenga, various countries do offer it in December 2025.
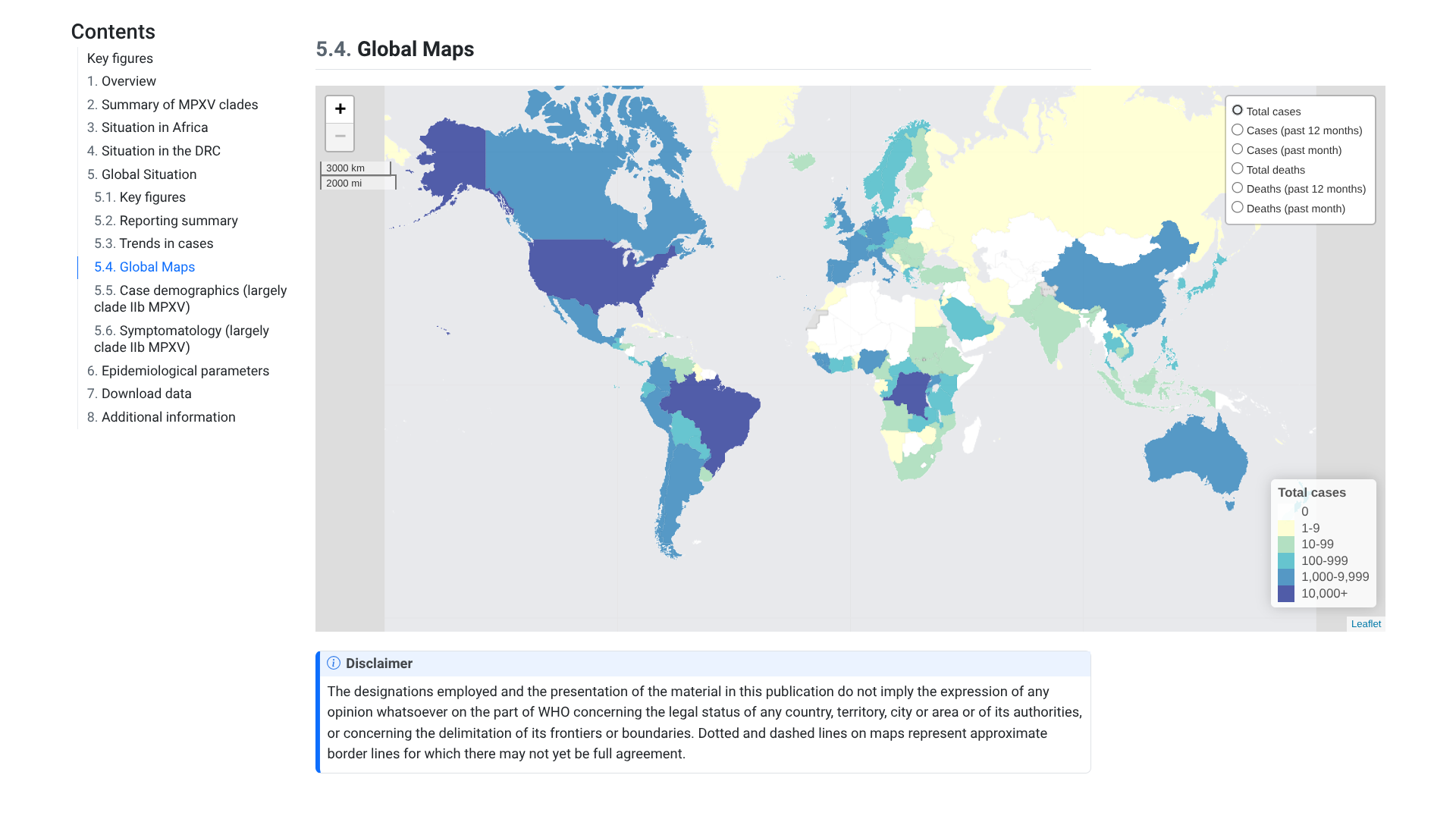
The World Health Organization (WHO) has published its 60th situation report on the multi-country mpox outbreak. Since May 2022, when the mpox outbreak was first recorded, the WHO's report offers insights into the global epidemiological situation and includes updated data on this severe disease.
As of December 8, 2025, the WHO stated that all clades of the monkeypox virus (MPXV) continue to circulate. When mpox outbreaks are not rapidly contained, and human-to-human transmission is not interrupted, there is a risk of sustained community transmission.
For example, in October 2025, 44 countries across all WHO regions reported 2,501 new confirmed mpox cases, including 12 related deaths, for a case fatality ratio of 0.5%. About 75% of these cases were reported in the African Region.
Outside Africa, local transmission of clade Ib MPXV has been occurring in Italy, the Netherlands, Portugal and Spain, the United States of America, and Malaysia.
New imported mpox cases due to clade Ib MPXV have been detected among travellers in Belgium, Germany, Greece, and the United Kingdom of Great Britain and Northern Ireland.
According to the U.S. CDC, mpox is a vaccine-preventable disease and is recommended for those at risk.
Getting both recommended JYNNEOS doses provides the best protection against monkeypox.
The CDC says that whether or not you've been vaccinated, you can continue to reduce your risk of getting monkeypox.