Search API
An updated direct-to-consumer (DTC) test that reports selected BRCA1/BRCA2 genetic variants was updated to add 41 BRCA1/BRCA2 variants to the previously authorized test.
This DTC test analyzes DNA from a self-collected saliva sample.
It generates personalized reports describing if the genetic variants detected in that sample are associated with an increased risk of developing breast and ovarian cancer and may be associated with an increased risk for prostate, pancreatic, and potentially other cancers.
On September 1, 2023, the U.S. Food and Drug Administration announced it cleared for marketing the updated 23andMe Personal Genome Service Genetic Health Risk Report for BRCA1/BRCA2.
These reports provide genetic information to inform discussions with a healthcare professional.
Consumers and healthcare providers should not use the test results to substitute for healthcare visits for recommended cancer screenings or appropriate follow-up; results from this test should not be used to determine any treatments.
This report does not represent most of the BRCA1/BRCA2 variants in people of most ethnicities. This means a negative result does not rule out the presence of other variants that increase cancer risk, says the FDA.

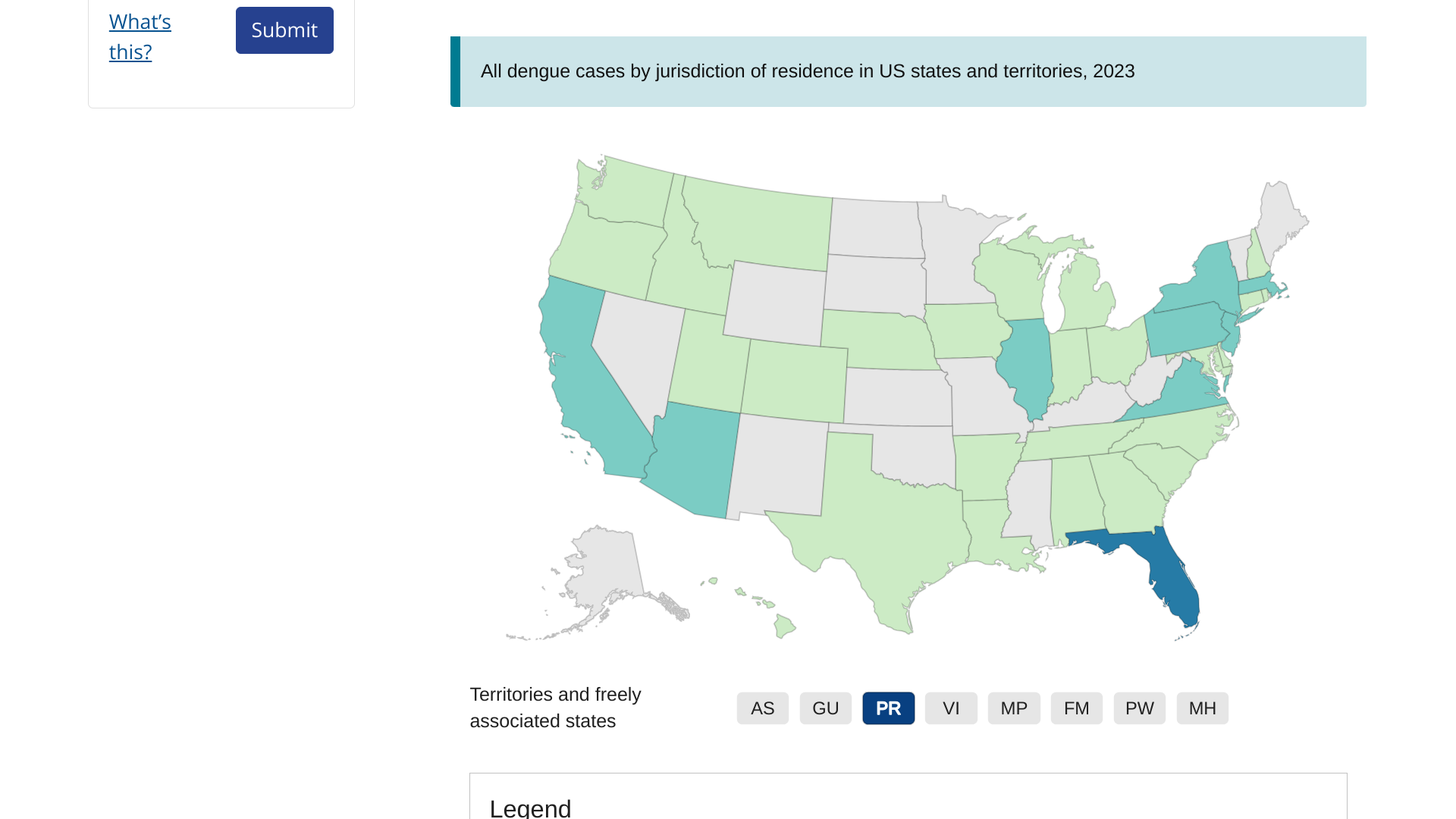
While many in the United States are watching the weekly increase in Dengue virus cases reported in Florida and Puerto Rico, this mosquito-carrying disease is creating havoc in Asia.
According to the World Health Organization (WHO)'s Dengue Situation Report #1, Bangladesh has joined its neighbor India in confirming Dengue has become endemic, with yearly peaks in cases and deaths around the monsoon season.
As of August 27, 2023, the upsurge in Dengue cases started around the last week of April.
This year's total has reached 119,133 cases, and 569 related deaths have been reported from all 64 districts in Bangladesh.
This makes it the largest outbreak of Dengue ever reported in Bangladesh.
Tested samples indicated DENV-2 (62%) and DENV-3 (29%) are the primary circulating serotypes.
The WHO stated it is leading partners to support the national authorities to mount a coordinated response to the outbreak. The government has requested immediate support for test kits, IV fluids, and laboratory equipment for early detection and better case management.
Additionally, the U.S. CDC has deployed one expert from its Dengue Branch in Puerto Rico to provide technical assistance in the field of clinical case management.
This situation report summarizes the status of the outbreak and some of the support being provided.
As of September 4, 2023, there have been no reports of a Dengue vaccination program in Bangladesh. There are two Dengue vaccines in use in certain countries.

The U.S. Transportation Security Administration (TSA) recently announced that since Memorial Day 2023, it has screened an average of more than 2.4 million people per day at more than 430 airports nationwide.
The Memorial Day and Fourth of July holiday weekends set records for the number of people screened, and the Labor Day holiday is shaping up to be busy as well.
TSA Federal Security Director for Washington, Greg Hawko, commented in a press release, “If you are traveling this Labor Day weekend, please take a few minutes to ensure you are prepared for the security screening process.”
Across the country, TSA expects to screen 14.25 million passengers and crew between September 1, 2023, and September 6, 2023, which is an 11% increase over 2022.
Furthermore, travelers enrolled in TSA PreCheck® wait less than 10 minutes during the screening process.
As of September 2, 2023, national airport checkpoint screening statistics are available at www.tsa.gov/travel/passenger-volumes, showing an increase from 2019.

Over the past two years, measles outbreaks have significantly increased in various countries, but not the United States.
However, the Texas Department of State Health Services (DSHS) recently published a Health Alert regarding two measles cases.
On August 29, 2023, DHSH confirmed the first measles case was diagnosed in June in a resident of Hood County.
The second was diagnosed in August in McCulloch County.
Neither adult patient had a history of travel to an area where measles is spreading, and no other risk factors for exposure were identified. At this time, public health officials do not suspect these cases are related.
Both cases had received one dose of the measles-mumps-rubella (MMR) vaccine.
The U.S. CDC says one dose of MMR vaccine is 93% effective against measles, while two doses offer 97% protection.
Before vaccine introduction, annual measles incidence in Texas peaked at 85,862 in 1958. In 2019, Texas experienced a measles outbreak of 23 cases.
In 2019, research revealed three Texas counties, Harris, Tarrant, and Travis, were at risk for measles outbreaks. The study found two main factors: vaccine refusal rates, and the number of travelers from other countries.
As of early August 2023, the CDC reported 19 measles cases in thirteen U.S. jurisdictions. In 2022, there were 121 measles cases and 49 in 2021.
Globally, measles cases increased by about 80% during 2022 compared with 2021.
For example, India has reported about 57,000 measles cases over the past year.
Measles is a highly contagious respiratory illness. The virus is transmitted by direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes. According to the CDC, measles vaccination may prevent disease in exposed people within 72 hours of exposure.
If you think you have measles or have been exposed to someone with measles, isolate yourself from others and call your healthcare provider before arriving to be tested.
The incubation period averages 10-12 days from exposure to the onset of prodromal symptoms. People with confirmed or suspected measles should stay home from school, work, and other group settings until after the fourth day of rash onset.
The CDC says if you plan to travel internationally, ensure you and your loved ones are protected against measles before departure, no matter where you are going.
In the U.S., various measles vaccines are available at health clinics and pharmacies in September 2023.
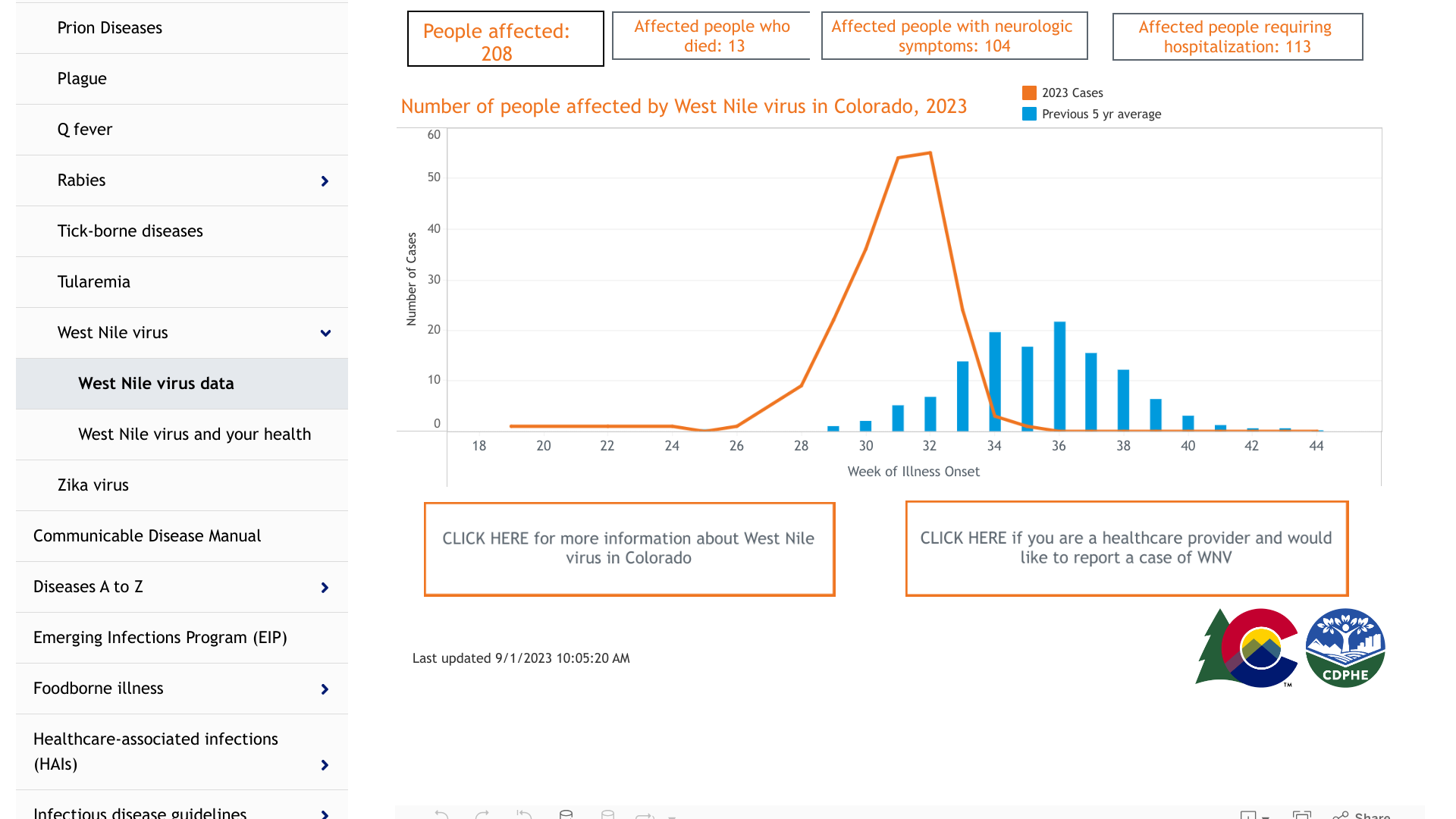
While West Nile Virus (WNV) has been detected in thirty-six states in 2023, Colorado is experiencing its worst outbreak in five years.
As of September 1, 2023, the Colorado Department of Public Health and Environment (CDPHE) reported that 13 people have died this year from WNV infection.
Additionally, 113 people have been hospitalized with WNV.
In 2022, Colorado reported 20 WNV deaths.
The abundance of the disease-carrying Culex mosquitoes in 2023 is likely due to the high level of precipitation last winter and spring.
“The trends we are seeing in our West Nile virus tracking data are unprecedented,” said Dr. Rachel Herlihy, state epidemiologist, CDPHE, in a press release on August 4, 2023.
While most people infected with West Nile virus don’t have symptoms, some can develop a serious, potentially deadly illness. People aged 60 and older and those with certain medical conditions are at greater risk of serious disease.
Dr. Michelle Barron, senior medical director of infection prevention and control for UCHealth, offered messages for people who are spending time outdoors and for those who may be feeling sick.
Protect yourself to avoid getting mosquito bites.
And, if you are feeling sick and suspect you might have West Nile virus, seek help from a doctor immediately.
“If your infection progresses to the point where you are having persistent headaches, confusion, any kind of muscle weakness, numbness or tingling, you need to be seen by a doctor as quickly as possible,” Barron said.
Barron offered answers to questions about WNV on September 1, 2023.
As of August 29, 2023, 455 human WNV cases and 315 Neuroinvasive Human Disease (meningitis or encephalitis) patients have been confirmed by the U.S. CDC. Furthermore, there are no approved West Nile virus vaccines in 2023.
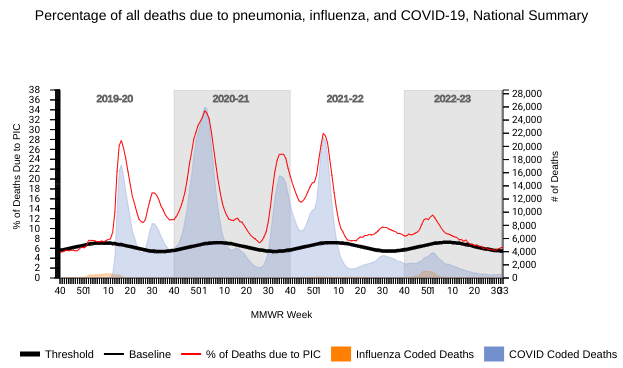
The lingering impact of the 2022-2023 flu season is still being counted at the U.S. Centers for Disease Control and Prevention (CDC).
On September 1, 2023, the CDC's Weekly U.S. Influenza Surveillance Report confirmed that 6.5% of the deaths during the week ending August 26, 2023, were due to pneumonia, influenza, and/or COVID-19.
Among the 1,484 deaths reported for this week by the National Center for Health Statistics Mortality Surveillance, nine listed influenza as an underlying or contributing cause of death on the death certificate.
The CDC's Week #34 report did disclose some good news regarding pediatric fatalities.
No influenza-associated pediatric deaths were reported to the CDC last week.
A total of 172 influenza-associated pediatric deaths that occurred during the 2022-2023 season have been reported, more significant than the last flu season when 49 flu-related deaths were confirmed.
This unfortunate increase may be related to decreased non-adults getting an annual flu shot.
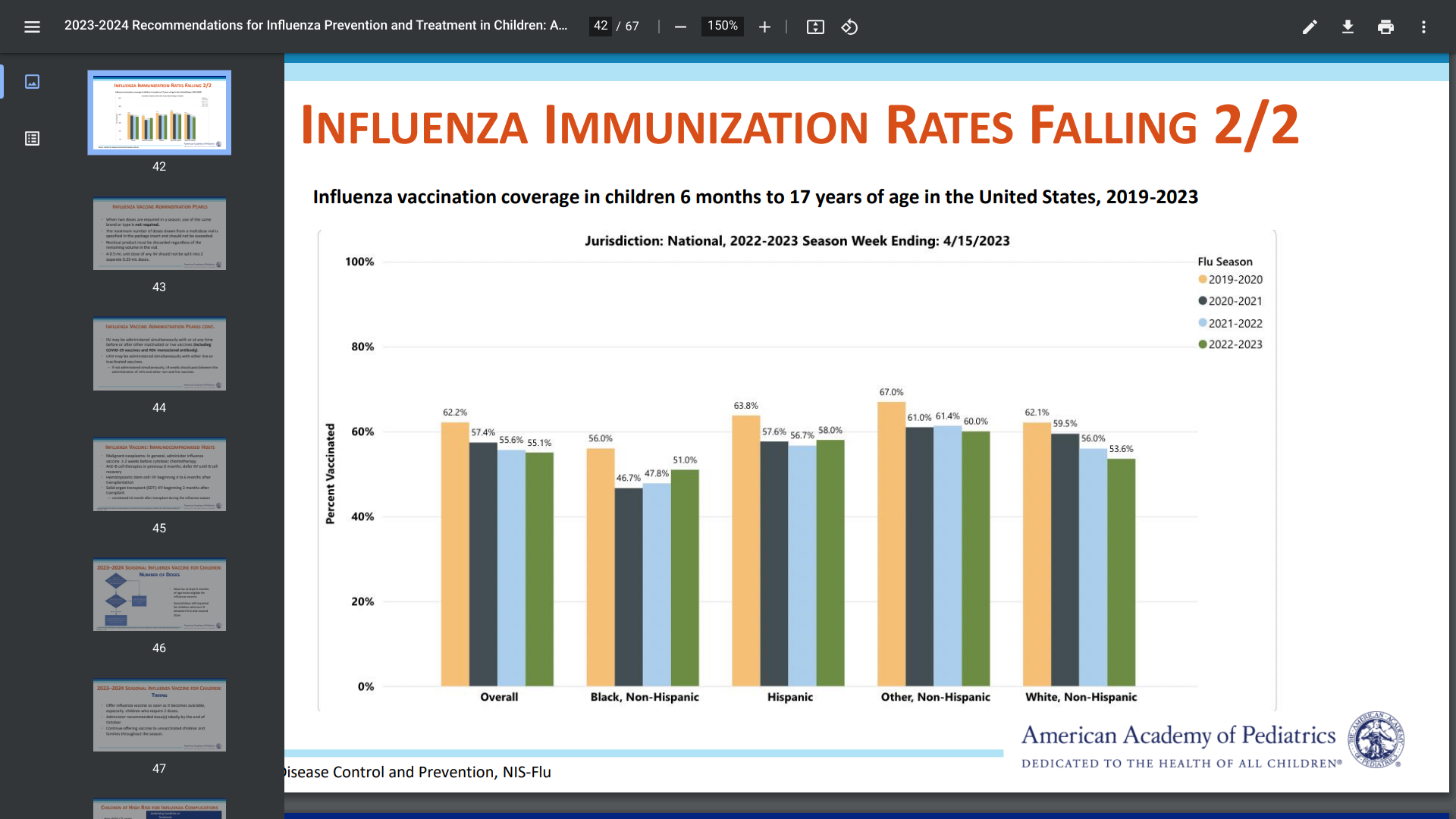
The CDC's Clinician Outreach and Communication Activity webinar on August 31, 2023, revealed that during the 2022-2023 flu season, only 55.1% of children received an annual flu shot.
This data compares with 2019-2022 when 62.2% of children got an annual flu shot.
As of September 2023, the CDC encourages most people six months and older to get at least one flu shot ahead of the 2023-2024 flu season.
The World Health Organization recently published Influenza Update N° 452, indicating influenza detections remained low globally, with activity in many countries in the southern hemisphere and Oceania decreasing after having peaked in recent weeks.
In the U.S., over 100 million influenza vaccines have been distributed to health clinics and pharmacies.
Last year’s flu season began earlier than expected in the United States, and many children were not protected from influenza.
To better understand this health risk, the U.S. Centers for Disease Control and Prevention (CDC) Clinician Outreach and Communication Activity webinar on August 31, 2023, presented an update on 2023-2024 influenza recommendations for non-adults.
This digital presentation revealed on slide #42 that influenza vaccination coverage in children six months to 17 steadily decreased during 2019-2023.
During 2019-2022, 62.2% of children got an annual flu shot.
In 2022-2023, only 55.1% of children received an annual flu shot.
Furthermore, the CDC reported that influenza-associated pediatric deaths during the 2022-2023 season have reached 172, a three-year high.
The CDC says annual flu shots for most people over six months of age are the most effective way to prevent influenza illness and associated complications.
From a protection perspective, the CDC says over 65% of influenza-vaccinated children were protected from flu-related hospitalization during 2023.
A clarification for this flu season is people with egg allergy may receive any influenza vaccine (egg-based or non-egg-based) that is otherwise appropriate for their age and health status; additional safety measures are no longer recommended.
And multiple vaccines can be administered along with a flu shot.
Additionally, coincident with National Immunization Awareness Month in August, the American Academy of Pediatrics released an updated policy statement and technical report on August 29, 2023, with recommendations for preventing and controlling influenza in children for the 2023-’24 influenza season.
As the summer of 2023 comes to a close, disease-carrying mosquitoes in Florida are not taking a break.
According to the Florida Department of Health's week #34 report, 21 new dengue virus cases were reported last week.
On August 28, 2023, twenty new dengue cases were reported this week in persons who had international travel. There are now 244 travel-associated dengue cases reported in Florida this year.
These dengue-infected visitors primarily came from Cuba (165) and Brazil (13).
Additionally, and more concerning, one new locally acquired dengue was reported last week in Miami-Dade County. In 2023, 16 cases of locally acquired dengue have been reported this year, with Miami-Dade confirmed 12 patients.
This data is positive news compared to 2022 when 68 locally acquired dengue cases were reported.
Furthermore, it appears the malaria outbreak in the Sarasota area has subsided. No cases of locally acquired malaria were reported last week.
In 2023, seven cases of locally acquired malaria have been reported.
While the U.S. CDC has not issued a travel advisory for these mosquito-carry diseases, various alerts have been issued by Escambia, Jefferson, Nassau, Orange, Polk, St. Johns, Walton, Broward, Manatee, Miami-Dade, and Sarasota counties.
In total, the CDC has confirmed 642 dengue cases in 38 jurisdictions this year, including San Juan, Puerto Rico with 41 cases.
From a disease prevention perspective, one dengue vaccine is approved for use in the U.S. The Dengvaxia® live attenuated tetravalent chimeric vaccine requires pre-admission testing.