Search API
Valneva SE today announces the submission of a marketing application with the European Medicines Agency (EMA) for approval of the Company's single-shot chikungunya vaccine candidate, VLA1553.
According to Valneva's press release on October 25, 2023, VLA1553 was also granted accelerated assessment for the application by EMA's Committee for Medicinal Products for Human Use based on the vaccine candidate's "major interest for public health and therapeutic innovation."
If approved in Europe, VLA1553 could become the first licensed chikungunya virus (CHIKV) vaccine to address this unmet medical need.
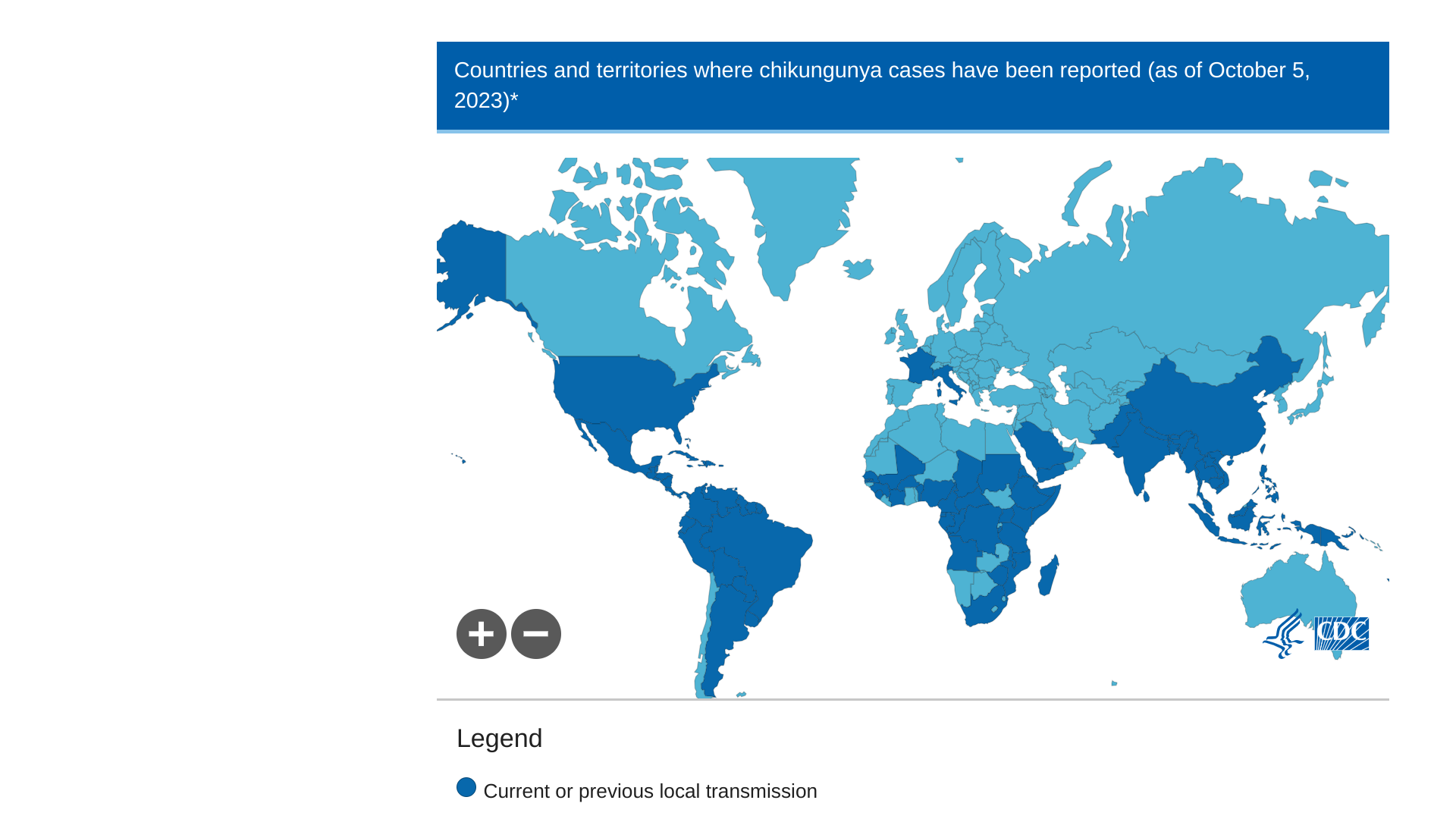
As of August 2023, approximately 320,000 CHIKV cases and over 340 related deaths have been reported worldwide by the European Centre for Disease Prevention and Control (ECDC).
VLA1553 is currently the first and only chikungunya vaccine candidate worldwide for which regulatory review processes are underway.
A Biologic License Application (BLA) is currently under priority review by the U.S. Food and Drug Administration, with a Prescription Drug User Fee Act action date planned for the end of 2023.
Additionally, a marketing application is under review by Health Canada.
Juan Carlos Jaramillo, MD, Chief Medical Officer of Valneva, commented, "Chikungunya virus is a serious and debilitating mosquito-borne viral infection that poses a significant unmet need, and the risk of chikungunya spreading in Europe is relatively high due to the possibility of infected travelers."
"No vaccine or specific treatments are currently available for this debilitating disease. We will continue to work diligently to bring VLA1553 to different territories as soon as possible."
Additionally, other CHIKV vaccine candidates are conducting clinical trials in 2023.
During 2023, chikungunya outbreaks were primarily found in Africa, the Americas, Asia, Brazil, and the Indian subcontinent. In January 2023, the U.S. Centers for Disease Control and Prevention reported 81 travel-associated CHIKV cases in the U.S. in 2022.
GSK plc today announced positive preliminary results from its phase III clinical trial evaluating the immune response and safety of the AREXVY™ respiratory syncytial virus (RSV) vaccine in adults aged 50 to 59, including those at increased risk of RSV lower respiratory tract disease (LRTD) due to certain underlying medical conditions.
In this study, the vaccine elicited an immune response in adults aged 50 to 59 at increased risk for RSV disease due to select underlying medical conditions that were non-inferior to that observed in adults aged 60 and above, meeting the trial's primary co-endpoint.
Vaccine efficacy has previously been demonstrated in adults aged 60 and above.
The co-primary endpoint was also met for the broader group of adults aged 50 to 59 also enrolled in the trial. Safety and reactogenicity data were consistent with results from the initial phase III program.
The most common local adverse event was pain, and the most common systematic adverse events were fatigue and headache, most of which were transient and mild in intensity.
These results will be presented at the US Centers for Disease Control and Prevention's Advisory Committee on Immunization Practices meeting on October 25, 2023.
AREXVY is currently approved in the United States, Europe, Japan, and several other countries for active immunization for the prevention of RSV-LRTD in adults 60 years of age and older.
AREXVY recombinant, AS01E adjuvanted, single dose, RSV vaccine contains a recombinant subunit pre-fusion RSV glycoprotein antigen (RSVPreF3) combined with GSK's proprietary ASO1 adjuvant.
Tony Wood, Chief Scientific Officer, GSK, said in a press release on October 25, 2023, "This trial reinforces our confidence in our RSV vaccine's ability to help protect adults aged 50 to 59 at increased risk for RSV-LRTD."
"We will submit these data for regulatory review as quickly as possible with the goal of offering adults in this age group the option of a vaccine for the first time."
There is a substantial burden of RSV-associated illness for adults at increased risk for RSV disease due to advanced age, immunocompromised status, or underlying medical conditions, such as chronic obstructive pulmonary disease, asthma, and chronic heart failure. RSV can exacerbate these conditions and lead to pneumonia, hospitalization, or death.
The final results from this trial will be presented at an upcoming medical conference and submitted for peer-reviewed publication. The data will also be submitted to the US Food and Drug Administration and other regulators to support potential label expansions.

The National Institutes of Health recently awarded a $12.3 million contract to the University of Montana to develop a novel adjuvant for tuberculosis (TB) vaccine.
Adjuvants are integrated into numerous vaccines and are substances that boost their effectiveness.
The current leader in TB prevention is the 100-year-old Bacille Calmette-Guerin (BCG), whose various versions are used globally.
Merck's TICE® BCG vaccine is available in the U.S.
"The development and clinical evaluation of safe and effective adjuvants is urgently needed for the advancement of vaccines to combat the ongoing threat of bacterial and fungal infections, including tuberculosis, pertussis, and others," said Jay Evans, director of the UM center, in a press release on October 23, 2023.
Evans commented vaccine development for TB and other bacterial and fungal pathogens has been hampered by the lack of appropriate adjuvants and effective formulations.
"There is extraordinary research ongoing at UM that could positively impact the lives of countless people," Evans said. "Our Vaccine Research Team is dedicated to nurturing and cultivating an interactive research community at UM, specifically geared toward advancing these technologies to help individuals and communities in Montana and across the globe."
Drs. Evans and Walid Abdelwahab, along with their colleagues, are the co-principal investigators on the contract. The project includes researchers from the University of Chicago (Dr. Shabaana Khadar), the Texas Biomedical Research Institute (Dr. Smriti Mehra), and Missoula-based Inimmune Corp., a corporate development partner.
This new contract builds upon a recently completed $13 million NIH Adjuvant Discovery Contract, which identified the lead candidate being advanced toward human clinical trials in the current award.
According to the World Health Organization (WHO), 1.6 million people died from TB in 2021. Worldwide, TB outbreaks are the 13th leading cause of death.
In 2020, almost two-thirds of TB cases in children worldwide were either not reported or went undiagnosed and untreated, according to the WHO.
Certain cities have recently reported increases in TB cases in the United States.
The U.S. CDC reported in March 2023 that TB cases increased by 5% in 2022, with 60 U.S. states, the District of Columbia, and territories provisionally reporting 8,300 TB cases.
The Federal Republic of Nigeria today announced the introduction of the human papillomavirus (HPV) vaccine into its routine immunization system.
The west African country of Nigeria aims to reach 7.7 million girls aged 9–14 in a vaccination drive against HPV types 16 and 18 that cause most cervical cancer cases.
As of October 24, 2023, this is the most significant number in a single round of HPV vaccination in the African region.
The second phase of the vaccination introduction is set to start in May 2024.
"The loss of about 8,000 Nigerian women yearly from a preventable (sexually transmitted) disease is completely unacceptable," says Muhammad Ali Pate, the Coordinating Minister of Health & Social Welfare, in a related press release.
A five-day mass vaccination campaign in schools and communities will be carried out during the inaugural rollout in 16 Nigerian states and the Federal Capital Territory.
The Federal Ministry of Health provides the vaccine for free through the National Primary Health Care Development Agency with support from Gavi, the Vaccine Alliance, United Nations Children's Fund (UNICEF), World Health Organization (WHO), and other partners.
WHO recommends that HPV vaccination be included in the national immunization programs of countries where cervical cancer is a public health priority and its cost-effective and sustainable implementation is feasible.
The Lancet Oncology reported in September 2023 that African countries are home to 19 of 20 countries with the highest burden of cervical cancer.
However, global supply shortages have slowed Gavi-supported HPV vaccine introductions.
These supply issues are now easing thanks to years of market-shaping efforts to develop a more robust HPV vaccine market and the single dose recommendation.
The Gavi board recently approved revitalizing its HPV vaccine program with an investment of over US$ 600 million by the end of 2025. With the additional funding, Gavi and its partners have set an ambitious goal to reach over 86 million girls by 2025, aiming to avert over 1.4 million future deaths from cervical cancer.
The WHO currently supports a one-dose regimen of the HPV vaccine for certain people.
The WHO's vaccine advisors recommend updating HPV dose schedules as follows: one or two-dose program for the primary target of girls aged 9-14, one or two-dose plan for young women aged 15-20, two doses with a 6-month interval for women older than 21, and immunocompromised individuals, including those with HIV, should receive three doses if feasible.
As of October 2023, there are effective HPV vaccines that protect men and women against cancers caused by HPV. These approved vaccines include 9vHPV, 4vHPV, and/or 2vHPV.

While two approved dengue vaccines are in use today, an innovative vaccine candidate was awarded $5.88 million to support activities to advance it into the clinic.
Codagenix Inc. announced on October 24, 2023, that the U.S. Department of Defense (DoD) awarded the Company $5,880,000 to advance the development of its CodaVax-DENV, a tetravalent live-attenuated dengue vaccine program.
The funds will support good manufacturing practices of drug substances and tetravalent drug product for a Phase 1 study, as well as a first-in-human Phase 1 safety and immunogenicity clinical trial.
This new award complements a $4.4 million DoD grant issued in 2022.
Codagenix's rational vaccine design platform is well-positioned to create a safe and effective dengue vaccine since its codon deoptimization process has the potential to provide immunity against all four dengue serotypes in a tetravalent formulation without the use of a backbone virus.
In addition to CodaVax-DENV, several dengue vaccine candidates are conducting clinical trials in 2023.
"We are honored to be selected for this award and would like to thank the DoD for their continued support, which is a recognition of the advantages of CodaVax-DENV, including codon deoptimization, homologous DENV 1, 2, 3, 4 strains, and the ability to titrate attenuation to develop balanced immunity," commented Jeffrey Fu, Ph.D., Chief Business Officer of Codagenix, in a related press release.
"These qualities uniquely position CodaVax-DENV to address the unmet needs in dengue prevention."
Dengue is a mosquito-borne viral infection, with over 2.4 billion people living in dengue-endemic areas worldwide; it is a leading cause of serious illness in several Latin American and Asian countries in 2023.
To alert international travelers of this health risk, the U.S. CDC recently issued Travel Health Notices regarding dengue outbreaks in the Americas (September 25, 2023), Africa/Middle East (October 18, 2023), Costa Rica, and Asia/Pacific Islands (July 25, 2023).
In the United States, Puerto Rico and Florida have reported the most dengue outbreaks in 2023.

The number of new HIV infections remains unacceptably high, and urgent new approaches are needed to advance HIV vaccine science. However, developing a preventive HIV vaccine has proven to be an intractable scientific challenge, wrote Prof Alexandra Trkola, PhD, and Prof Penny L Moore, PhD, in an article published by The Lancet Infectious Diseases.
This view was published on October 23, 2023, and stated, 'Recent advances in HIV immunogen design have taken the field closer to triggering the rare precursors of broadly neutralizing antibodies, which are widely assumed to be necessary for a vaccine.
Nonetheless, these same studies and previous studies in people living with HIV have also highlighted the significant hurdles that must be overcome to boost the cross-reactivity and potency of these responses to sufficient levels.
Here, we describe an opportunity for fast-tracking the evaluation of candidate preventive and therapeutic vaccines by immunizing people with HIV who are antiretroviral therapy suppressed.
We argue that such studies, unlike traditional studies of vaccines in participants not infected with HIV, will be faster and more informative and will allow the vaccine field to bypass multiple hurdles.
This approach will accelerate the process of defining the capacity of immunogens to trigger relevant antibodies, currently an extremely slow and expensive pathway, and provide a quick path to creating an HIV vaccine.'
The full, unedited article is posted at this link.
Following the discovery of HIV as a causative agent of AIDS, multiple HIV vaccine clinical trials have been conducted globally over the past 35 years. As of October 24, 2923, there are several HIV vaccine candidates conducting research.
According to the U.S. National Institutes of Health, HIV vaccine candidates can not cause an HIV infection.

The U.S. Centers for Disease Control and Prevention (CDC) today announced the Health Alert Network Health Advisory (CDCHAN-00499) that offers options for clinicians to protect infants from respiratory syncytial virus (RSV) in the context of a limited supply of Beyfortus™ (nirsevimab), a single-dose, long-acting monoclonal antibody product.
In July 2023, the U.S. Food and Drug Administration (FDA) approved Beyfortus for passive immunization to prevent RSV-associated lower respiratory tract disease among infants and young children.
For the 2023–2024 RSV season, the manufacturer reports a limited supply of Beyfortus, particularly the 100mg dose prefilled syringes used for infants weighing ≥5 kg.
Based on manufacturing capacity and currently available stock, the CDC says there are insufficient 100mg dose prefilled syringes of Beyfortus to protect all eligible infants weighing ≥5 kg during the current RSV season.
In the context of limited supply during the 2023–2024 RSV season, CDC recommends prioritizing available Beyfortus 100mg doses for infants at the highest risk for severe RSV disease: young infants (age <6 months) and infants with underlying conditions that place them at highest risk for severe RSV disease.
As of October 23, 2023, the CDC's recommendations for using 50mg doses remain unchanged.
Avoid using two 50mg doses for infants weighing ≥5 kilograms (≥11 pounds) to preserve supply of 50mg doses for infants weighing <5 kilograms (<11 pounds).
The CDC further recommends that providers suspend using the single-dose Beyfortus in the multidose Synagis® (palivizumab)-eligible children aged 8–19 months for the 2023–2024 RSV season.
These children should receive the multidose Synagis per the American Academy of Pediatrics recommendations.
Synagis was initially approved by the U.S. FDA in 1998.
However, Beyfortus should continue to be offered to American Indian and Alaska Native children aged 8–19 months who are not palivizumab-eligible and who live in remote regions, where transporting children with severe RSV for escalation of medical care is more challenging or in communities with known high rates of RSV among older infants and toddlers.
RSV is a common cause of respiratory infection in U.S. infants, most of whom are infected with RSV during their first year of life. RSV is the leading cause of hospitalization among U.S. infants.
The highest incidence of RSV-associated hospitalization occurs in infants aged <3 months and then decreases with time.
The Journal of Infectious Diseases published a meta-analysis in October 2023 that found among 8,126 pregnant women, the proportion with respiratory infections that tested positive for RSV ranged from 0.9% to 10.7%, with a meta-estimate of 3.4% (95% CI: 1.9; 54).
As of October 9, 2023, RSV activity was found to be generally low, according to the WHO's Influenza Update N° 455.
Current reports to the National Respiratory and Enteric Virus Surveillance System indicate RSV transmission has increased to seasonal epidemic levels in the Southern regions, such as in Florida, and is expected to continue to increase in the rest of the country within the next few months.
The CDC's RSV detection graphs display the 5-week moving average in U.S. states as of October 19, 2023.
These interim recommendations by the CDC are subject to change as new evidence becomes available.