Search API
The World Health Organization (WHO) is hosting a free webinar today titled: Chikungunya: Experiences from the current response to outbreaks in the Americas.
Chikungunya is a viral disease transmitted to humans through the bites of Aedes mosquitoes infected with the chikungunya virus. It has been identified in nearly 115 countries in all the continents except Antarctica.
There are chikungunya vaccine candidates in development as of May 3, 2023. However, there are no approved vaccines.
On May 3, 2023, the speakers were:
- Dr. Sylvie Briand, Director, Epidemic and Pandemic Preparedness and Prevention (EPP), WHO
- Dr. Maria Van Kerkhove, Unit Head, Emerging Diseases and Zoonoses Unit, WHO
- Dr. Thomas Scott, Distinguished Professor of mosquito-transmitted disease ecology and epidemiology, University of California, USA
- Dr. Diana Rojas Alvarez, Technical Lead - Zika and Chikungunya, WHO
- Ms. Thais dos Santos, Advisor on Surveillance and Control of Arboviral Diseases, WHO PAHO
This session can be watched on YouTude.

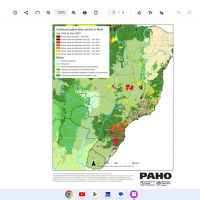
The Pan American Health Organization / World Health Organization (PAHO/WHO) latest Epidemiological Update highlights yellow fever hot spots in the Region of the Americas.
As of April 25, 2023, the PAHO/WHO reported that in 2023, human yellow fever cases have been recorded in Bolivia (two cases) and Brazil (three cases).
In 2022, confirmed cases of yellow fever were reported in three countries in the Americas: Bolivia (5 confirmed cases), Brazil (5 cases, including four deaths), and Peru (7 confirmed cases, including five deaths).
As of May 3, 2023, various countries require proof of yellow fever vaccination at airports upon arrival.
In the U.S., yellow fever vaccine (YF-VAX®) availability is limited to certified clinics and travel pharmacies.
Internationally, the Stamaril® is generally available in 2023.

The U.S. Centers for Disease Control and Prevention (CDC) today announced it issued an Alert - Level 2, Practice Enhanced Precautions regarding the Republic of the Philippines reporting increased diphtheria cases in various regions.
As of May 1, 2023, the CDC says if you are traveling to an affected area, you should be up to date with your diphtheria vaccines.
And before visiting the Philippines, discuss the need for a booster dose with your healthcare professional.
Diphtheria is a severe infection caused by strains of Corynebacterium diphtheriae bacteria that make a toxin.
When the bacteria enter the respiratory system, they can cause sore throat, mild fever, and swollen glands in the neck. In addition, the bacteria make a toxin that kills healthy tissues in the respiratory system and can make it difficult to breathe and swallow.
For some people, respiratory diphtheria can lead to death. Even with treatment, about 1 in 10 patients with respiratory diphtheria die.
Without treatment, up to half of patients can die from the disease, says the CDC.
Additionally, the CDC included the Philippines in a recent dengue outbreak alert.

During the 2022 Mpox outbreak in New York City, a disproportionate number of those infected also lived with HIV. Tecovirimat (TPOXX) was the agent most used for treatment.
SIGA Technologies, Inc. originally developed this medication and was initially approved for the treatment of smallpox,
As of May 2, 2023, no published data compared Mpox virus (MPXV) treatment outcomes between patients with HIV infection and those without.
In this preliminary study, the clinical presentation and treatment outcomes in 154 patients with confirmed MPXV infection were treated with tecovirimat with and without HIV.
This study found no significant differences in clinical presentation or treatment outcomes between the two study groups.
As in other U.S. data, patients in this report were almost exclusively men. However, people with HIV infection were slightly older (mean, 39 vs. 32 years).
They were more likely than HIV-negative patients to identify as Black or Hispanic, which reflects both the disproportionate burden of HIV in these groups and the underlying demographics of patients receiving HIV care at Columbia University Medical Center and Weill Cornell Medical Center.
In this study, people with HIV (PWH) were likelier to report skin lesions, fever, and diarrhea on day 1 of illness.
In contrast, those without HIV were more likely to experience a prodrome and to develop additional symptoms or examination findings, including lymphadenopathy.
This discrepancy in lymphadenopathy was also noted in a large U.S. case series (10) but not in a similar German report (9).
The significance of this difference is unclear, but it may contribute to diagnostic uncertainty in PWH between MPXV and herpesviruses, such as herpes simplex virus and varicella-zoster virus, which do not typically present with enlarged lymph nodes.
Prior reports suggest that PWH are hospitalized with mpox at higher rates than HIV-negative persons.
We found no apparent differences in hospitalization rate, but this may have been affected by the very low proportion of patients in our cohort with a CD4 count less than 0.20 × 109 cells/L.
Additional study is needed comparing disease severity and therapeutic decision-making between PWH with low CD4 cell counts and others with mpox.
As in other reports, tecovirimat was well tolerated in this case series, with no serious adverse events attributed to the medication.
Some symptoms noted as adverse effects (such as fatigue or malaise) are also symptoms of an infection; therefore, attribution to medication alone is difficult.
Finally, persons in this series had similar treatment outcomes regardless of HIV status. As in other reports, almost all patients had complete resolution of pain by the end of treatment.
Additional studies are needed to show the effect of tecovirimat on disease progression and to track the timeline of symptom resolution more closely, wrote these researchers.
Although it remains unclear how the incidence and demographic features of the current mpox outbreak will develop going forward, the present scenario requires a better understanding of both disease and treatment in those who bear the most significant disease burden to date—primarily MSM and PWH.
Tecovirimat is a promising treatment whose efficacy will hopefully be borne out in future rigorous studies.
Regardless, we believe that our study adds substantially to the body of knowledge about patient experience with tecovirimat therapy and can help inform patient counseling during treatment initiation, concluded these researchers.
Notes:
This study had several limitations, such as no control group of patients infected with MPXV who did not receive tecovirimat.
No studies to date compare treatment outcomes of PWH versus those of HIV-negative persons. To what degree HIV acts as an independent risk factor for mpox acquisition is unclear. However, emerging data suggest that uncontrolled HIV infection is a risk factor for developing severe disease.
And a recent report from the U.S. Centers for Disease Control and Prevention noted higher hospitalization rates among persons infected with HIV and MPXV, but data on determinants of the decision for hospitalization were not reported.
This study did not disclose the person's Mpox vaccination status.
The National Institutes of Health funded this study but had no role in the study design; collection, analysis, or interpretation of data; writing of the report; or the decision to submit the manuscript for publication.
Additional Mpox research is posted by Precision Vaccinations.

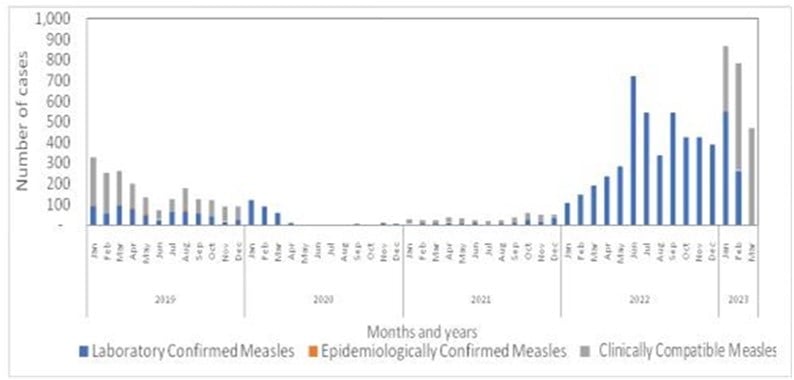
The World Health Organization (WHO) recently reported, based on the current data and available information from the Indonesia Ministry of Health, the overall risk of measles at the national level is assessed as high.
And the WHO reconfirmed measles is endemic in Indonesia and is an ongoing risk around the world.
On April 28, 2023, the WHO reported a total of 2,161 measles cases had been reported across 18 of 38 provinces in Indonesia, primarily from the provinces of West Java (796 cases) and Central Papua (770 cases) from January thru April 3, 2023.
In 2022, a total of 4,845 laboratory-confirmed measles cases and six deaths were reported across 32 of the 38 provinces.
To alert international visitors, the U.S. CDC issued a Watch - Level 1, Practice Usual Precautions regarding the global measles outbreak, which included Indonesia.
Recently, American Samoa's government declared a measles outbreak.
Measles is caused by a highly contagious virus that spreads through the air by direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes. The measles virus can live for up to two hours in airspace after an infected person leaves an area.
Furthermore, the CDC says that measles can be severe in all age groups and can lead to serious complications, such as pneumonia.
And all international travelers, including infants and children, should be fully vaccinated against measles.
Measles vaccines are generally available at clinics and community pharmacies in the U.S.
Despite the U.S. government's plan to end the public health emergency in May 2023, the National Council on Aging (NCOA) today announced it is distributing about $50 million in Department of Health and Human Services (HHS) grants to improve COVID-19 vaccine access and education.
"Those living at home are less likely to have access to the pharmacy," commented Josh Hodges, Chief Customer Officer at NCOA, as McKnight's Home Care Daily Pulse reported on May 1, 2023.
"They're less likely to be able to interact with their community as a whole, so bringing the vaccine into the home is part of what many of our organizations are doing."
"It's not only important for the individual themselves, but the caregivers, the family members, and those surrounding the older adult," added Hodges.
With $50 million in federal funding from the HHS' U.S. Administration for Community Living, the largest grant in its history reported NCOA.
Previously, LeadingAge confirmed on April 17, 2023, it would distribute $270,000 in grants among 20 member organizations to boost vaccinations.
LeadingAge's partnership with HHS' We Can Do This campaign is the latest pandemic-related collaboration between the two organizations.
Note: Pharmacies in the U.S. have distributed over 50% of all COVID-19 vaccines in 2023.