Search API
The Chicago Department of Public Health (CDPH) today declared the recent outbreak of measles in the City of Chicago officially over. Two full incubation periods (42 days) have passed without any new measles cases.
On March 7, 2024, CDPH confirmed the first case of measles in Chicago in five years. In total, 64 individuals tested positive for measles, 57 of whom were associated with a shelter setting.
Over 30,000 measles-mumps-rubella vaccine doses have been administered to Chicago residents.
CDPH Commissioner Dr. Olusimbo Ige said in a press release on May 31, 2024, “Our goal is the elimination of measles in Chicago and everywhere, and with proper vaccination coverage, we know that zero is possible.”
For those who are traveling internationally, additional measles vaccinations may be recommended. Talk with your healthcare provider (doctor, nurse, pharmacist) before traveling about vaccinations you and your family may need, wrote CDPH.
As of May 30, 2024, the U.S. CDC reported a total of 146 measles cases in 21 jurisdictions: Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, New York State, Ohio, Pennsylvania, Vermont, Virginia, Washington, West Virginia, and Wisconsin.
There have been 11 outbreaks (three+ cases) reported in 2024.
Globally, measles cases have been confirmed in 52 countries in the past year by the CDC.

Due to the rise in dengue fever cases in the southern hemisphere this year and the start of the high transmission season in the northern hemisphere, the Pan American Health Organization (PAHO) is urging the Caribbean and Central American countries to enhance preventive measures against this mosquito-borne viral disease.
An Epidemiological Alert announced on May 28, 2024, reported that the Americas region has reported more than 8.1 million suspected dengue cases, a 3.3-fold increase compared to the same period in 2023.
More than 3,600 dengue-related deaths have been reported throughout the region.
Mexico has reported over 65,000 dengue cases, Guatemala over 12,000, Honduras over 20,000, and Panama over 5,800.
Meanwhile, countries and territories in the Caribbean have reported over 21,000 cases, representing a 5.7-fold increase compared to the corresponding period last year.
Previously, the U.S. CDC stated that most dengue cases reported in the 49 continental states occur in travelers infected elsewhere. As of May 2024, travel-related and locally acquired dengue outbreaks were reported in southeast Florida, New York, and Puerto Rico in 2024.
In today's Alert, the PAHO emphasizes the importance of timely clinical diagnosis, early identification of warning signs, and proper patient management to avoid severe cases and deaths.
In most cases, dengue has no symptoms and can present as flu-like. However, when symptoms do occur, they usually include high fever, headache, body aches, nausea and rash.
Although most people recover within one to two weeks, some can develop severe forms that require hospitalization. These can be fatal when not treated promptly and adequately.
Either of the two WHO-listed vaccines can also prevent dengue. Unfortunately, their availability will be limited in 2024.

The U.S. Centers for Disease Control and Prevention (CDC) recently reported that three additional measles cases were confirmed in 2024.
As of May 23, 2024, the CDC confirmed a total of 142 measles cases were reported by 21 jurisdictions: Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, New York State, Ohio, Pennsylvania, Vermont, Virginia, Washington, West Virginia, and Wisconsin.
Recently, the city of Philadelphia reported another measles case after managing an outbreak earlier in 2024.
About 44% of these cases are in unvaccinated children under five years of age, with 63% hospitalized.
Ten measles outbreaks (3+) were reported in 2024, compared to four outbreaks in 2023.
Globally, about 50 countries have reported measles outbreaks in the past year.
The CDC says it is uncommon for someone fully vaccinated to develop measles. In 2024, the number of breakthrough infections (approximately 5%) was consistent with previous years' reports.
Two doses of MMR vaccine are 97% effective at preventing measles, and one dose is 93% effective. Measles vaccines are available at most clinics and pharmacies in the U.S.

The U.S. Centers for Disease Control and Prevention (CDC) recently highlighted two gateway cities as the unfortunate leaders in this year's dengue outbreaks.
According to New York City Health, travel-related dengue cases have increased among residents in recent years. As of May 21, 2024, the CDC confirmed 114 cases.
And the Florida Department of Health recently confirmed 173 travel-associated dengue cases, mainly by visitors from Brazil and Cuba, and 7 cases of locally acquired dengue were reported from two counties (Miami-Dade, Pasco).
In 2023, Florida reported 609 travel-associated dengue cases, and 186 people locally contracted dengue from the bites of infected mosquitoes.
Throughout the Americas, 7,327,521 suspected cases of dengue (an increase of 243% from 2023) and over 1,700 deaths have been registered in 2024.
While dengue is a vaccine-preventable disease, vaccinations are not generally offered in the U.S.

The U.S. Centers for Disease Control and Prevention (CDC) today confirmed that imported malaria in three U.S. southern border jurisdictions increased in 2023, particularly among new arrivals with recent complex transit through at least one country with endemic malaria.
The median travel duration was 29 days, and 73% reported traversing land borders.
On May 9, 2024, the CDC's Notes from the Field revealed that during 2023, 68 imported malaria cases were identified in Pima, Arizona (18), San Diego, California (27), and El Paso, Texas (23).
According to this Morbidity and Mortality Weekly Report, his data compares with 28 cases in 2022 (three in Pima, 12 in San Diego, and 13 in El Paso).
Overall, 63 (91%) patients with malaria in 2023 were hospitalized; no deaths were reported. Severe malaria was more common among other newly arrived migrants (37%) than among U.S. residents (7%).
These new arrivals were non–U.S.-born persons who had arrived in the United States within the preceding six months.
This CDC report is in addition to May 8, 2024, when the CDC reported ten Plasmodium vivax malaria cases in Los Angeles, California.
Seperately the states of Florida and Texas have reported imported malaria cases in 2024, 2023, and 2022.
Infected people who meet the criteria for uncomplicated malaria are generally treated with either hydroxychloroquine, chloroquine, or atovaquone/proguanil, followed by anti-relapse treatment with primaquine.
While malaria is now a vaccine-preventable disease, the two approved vaccines (Mosquirix™, R21/Matrix-M™) are not currently offered in the U.S.

In an essential step forward for malaria prevention in Africa, Benin, Liberia, and Sierra Leone today announced the launching of large-scale malaria vaccinations targeting millions of children across the three West African nations.
Today's launch confirms eight countries on the African continent have the opportunity to offer malaria vaccinations.
As of April 25, 2024, more than 30 countries in the African region are scheduled to roll out malaria vaccinations over the next year through support from Gavi, the Vaccine Alliance.
The World Health Organization (WHO) has recommended Mosquirix™ (RTS,S/AS01) and R21 / Matrix-M™ malaria vaccines.
A pilot malaria vaccine program in Ghana, Kenya, and Malawi reached over two million children from 2019 to 2023, showing a significant reduction in malaria illness, a 13% drop in overall child mortality, and substantial reductions in hospitalizations.
Aurelia Nguyen, Chief Programme Officer at Gavi, the Vaccine Alliance, commented in a press release, "Today we celebrate more children gaining access to a new lifesaving tool to fight one of Africa's deadliest diseases."
"Introducing malaria vaccines into routine programs in Benin, Liberia, and Sierra Leone alongside other proven interventions will help save lives and offer relief to families, communities, and hard-pressed health systems."
As of April 2024, neither malaria vaccine is available in the United States.
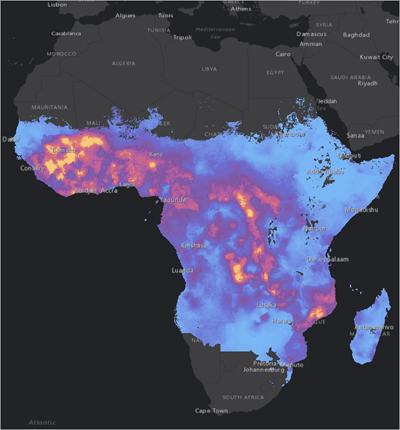
Malaria outbreaks remain a considerable health challenge in the African region, which is home to 11 countries that carry approximately 70% of the global burden of malaria.
According to the World Malaria Report 2023, the region accounted for 94% of global malaria cases and 95% of all malaria deaths in 2022.
In the U.S., about 2,000 travel-related malaria cases are reported annually. In the State of Florida, travel-related and locally acquired malaria cases have been reported over the past year.
To receive local travel vaccine recommendations, PassportHealth Tampa offers pre-departure advice.