Search API
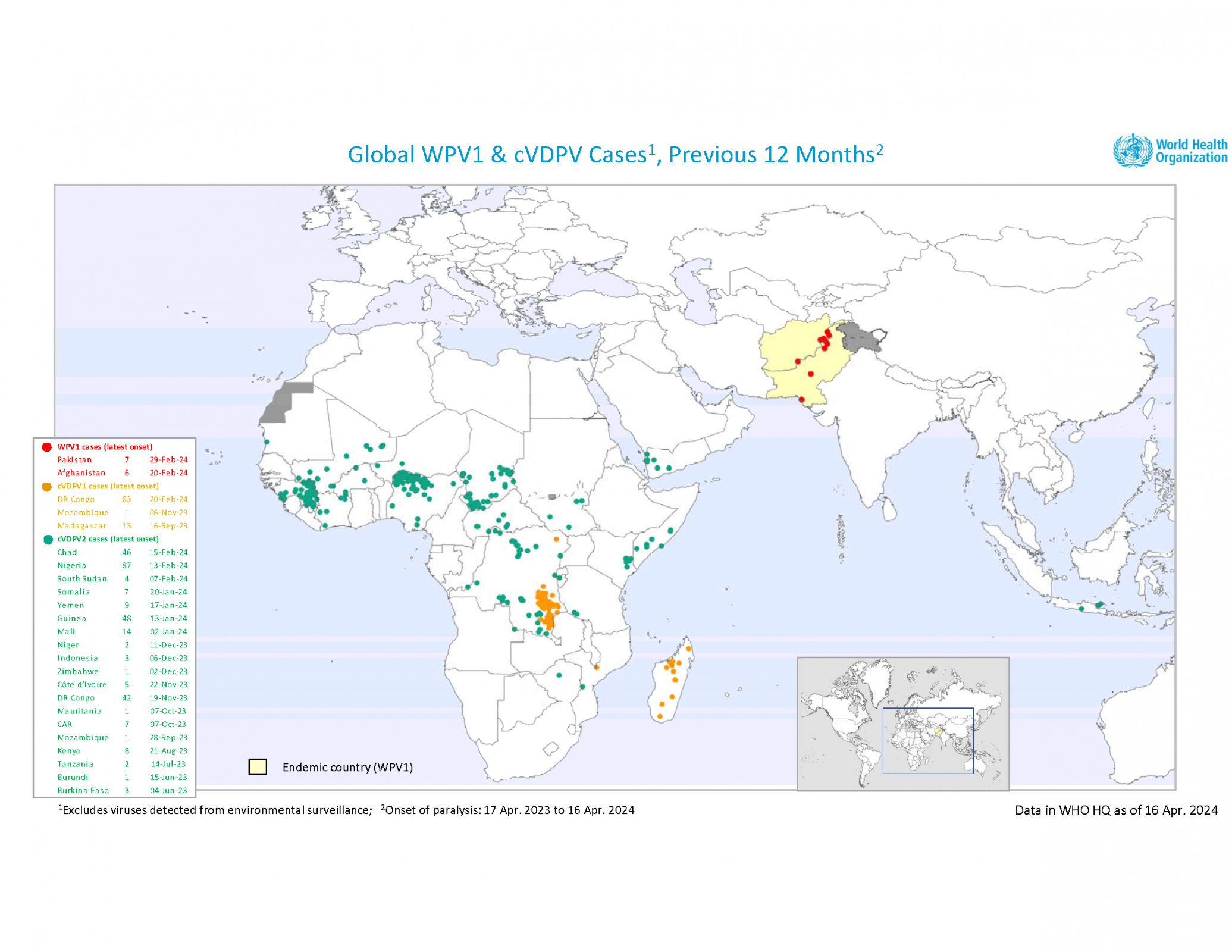
The WHO Director-General convened the thirty-eighth meeting of the Emergency Committee on the international spread of poliovirus in late March 2024.
The Committee unanimously agreed that the risk of the international spread of poliovirus remains a Public Health Emergency of International Concern and recommended the extension of Temporary Recommendations for a further three months until July 2024.
Regarding a weekly update, the Global Polio Eradication Initiative reported on April 17, 2024, that three African countries reported wild poliovirus (WPV1) and circulating vaccine-derived polioviruses (cVDPV) cases last week.
Chad reported one cVDPV2 case in Mandoul, making it the first in 2024. The number of 2023 cases remains 55.
The Democratic Republic of the Congo reported one cVDPV1 case in Haut-Katanga, the first this year. The number of polio cases in 2023 remains at 106, and 117 cases of cVDPV2 in 2023.
Nigeria confirmed one cVDPV2 case last week in Kebbi, the eighth this year. There have been 87 cases reported in 2023.
The U.S. CDC publishes travel advisories for countries reporting active polio cases and recommends fully vaccinating people before visiting these countries.
To understand polio vaccination options, including booster doses, the CDC suggests speaking with a travel vaccine advisor one month before traveling abroad.
Various media sources reported Merck would only supply 18.8 million HPV vaccine doses to Gavi-supported countries in 2024. Merck had previously promised to supply 29.6 million doses.
According to the Peoples Gazette, on April 19, 2024, Merck spokesman Patrick Ryan said the company "experienced a manufacturing disruption," requiring it to hold and check numerous doses manually.
Ryan disclosed that Burundi, Tajikistan, Mozambique, Sierra Leone, Ivory Coast, and Burkina Faso will not receive HPV vaccines in 2024.
By the end of 2022, 32 countries had successfully launched their HPV vaccine national program with Gavi support, fully immunizing more than 16.3 million girls since 2014.
GAVI says HPV vaccination is critical to reducing cervical cancer, especially in lower-income countries with a high disease burden and less developed cervical cancer screening and treatment programs.
On March 13, 2024, Merck announced plans to initiate clinical development of a new investigational multi-valent HPV vaccine designed to provide broader protection against multiple HPV types.
Separately, the company also plans to conduct clinical trials in both females and males to evaluate the efficacy and safety of a single-dose regimen of the GARDASIL®9 vaccine compared to the approved three-dose regimen.
"Evidence continues to emerge showing the importance of GARDASIL and GARDASIL 9 to public health," said Dr. Eliav Barr, senior vice president, head of global clinical development, and chief medical officer, Merck Research Laboratories, in a press release.
"These significant investments build upon our leadership and, importantly, provide the opportunity to further impact the global burden of certain HPV-related cancers and diseases."
The latest addition to Merck's pipeline employs the company's proprietary virus-like particle (VLP) technology to incorporate additional VLPs for expanded HPV-type coverage.
This includes several types known to have a greater impact on African and Asian populations and individuals of African and Asian descent. First-in-human phase 1 clinical studies are scheduled to start in the fourth quarter of 2024.
In the U.S., HPV vaccines remain available at clinics and pharmacies in 2024.

For many years, oral vaccines have proven to be the quickest intervention for preventing, limiting, and controlling cholera outbreaks.
However, the supply of these vaccines was at an all-time low in 2024, especially in 23 countries, including Comoros, the Democratic Republic of the Congo, Ethiopia, Mozambique, Somalia, Zambia, and Zimbabwe.
To help relieve this inventory shortage, the World Health Organization (WHO) issued a new oral cholera vaccine (OCV) prequalification.
On April 12, 2024, EuBiologicals Co., Ltd.'s inactivated oral vaccine, Euvichol-S, which has similar efficacy to existing vaccines but a simplified formulation, was announced.
This authorization creates new opportunities to increase OCV production capacity rapidly.
"The new vaccine is the third product of the same family of cholera vaccines on our WHO prequalification list," said Dr Rogerio Gaspar, Director of the WHO Department for Regulation and Prequalification, in a press release on April 18, 2024.
The WHO's OCV prequalification list already includes Euvichol, Euvichol-Plus, Vaxchora®, Dukoral®, and Shanchol™.
When visiting countries with cholera outbreaks in 2024, the U.S. Centers for Disease Control and Prevention recommends OCV vaccination one month before traveling.

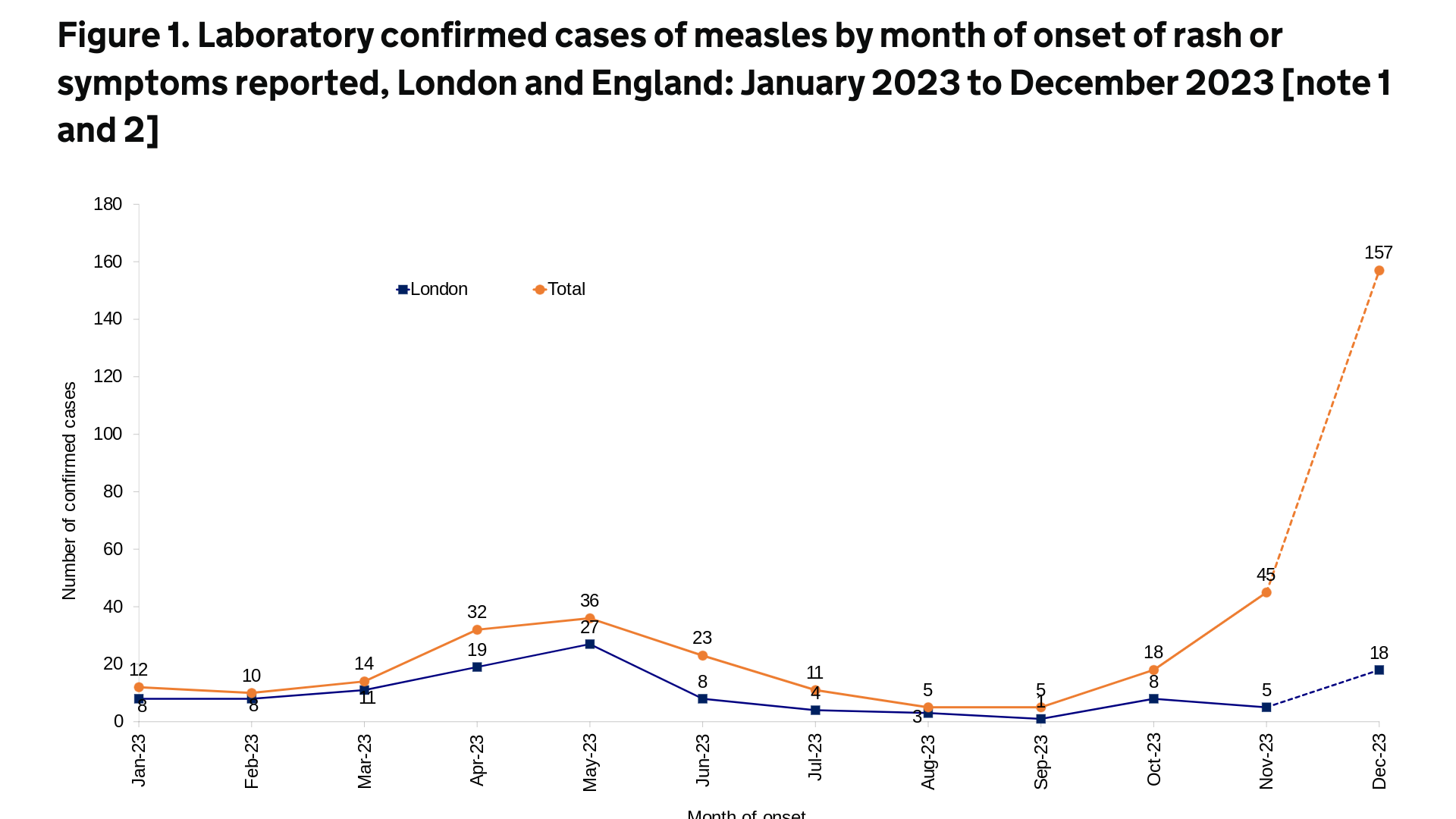
While measles outbreaks have been reported in dozens of countries in 2024, recent attention has focused on the cities of Chicago and London.
The U.K. Health Security Agency (UKHSA) published an updated epidemiological overview on April 18, 2024, stating that an additional 86 cases of measles were confirmed in England last week.
This data brings the total number of confirmed cases since October 2023 to 1,109.
About 39% of the U.K.'s measles cases (76 of 191) were in London during the last four weeks.
In a press release, Dr. Vanessa Saliba, UKHSA Consultant Epidemiologist, commented, "We know some communities in London have very low measles-mumps-rubella (MMR) vaccination rates. The MMR jab offers the best protection against measles."
The effective Priorx MMR vaccine is generally available at clinics and pharmacies in England. However, no measles-only vaccines are offered in England.
In the U.S., the Centers for Disease Control and Prevention (CDC) reported 121 measles cases in eighteen jurisdictions in 2024.
Most of these cases (61) have been reported by the Chicago Department of Public Health over the past two months.
The U.S. CDC republished a global Watch-Level 1, Practice Usual Precautions, Travel Health Notice in March 2024, alerting international travelers of potential health risks and identifying measles outbreaks in 49 countries.
The CDC recommends speaking with a travel vaccine consultant one month before traveling abroad to any outbreak countries.
GSK plc today announced positive data from a long-term follow-up phase III clinical trial. The trial followed participants up to approximately 11 years following initial vaccination with Shingrix®, a non-live, recombinant subunit Herpes Zoster vaccine.
Announced on April 17, 2024, the final trial data demonstrate that Shingrix maintained efficacy against shingles for over a decade across all age groups.
The results from the ZOSTER-049 study, an extension from two phase III clinical trials in adults aged 50 and over (ZOE-50 and ZOE-70), include:
- 79.7% vaccine efficacy (VE) in adults aged ≥50 cumulatively within the period from year six to year 11 after vaccination,
- 82.0% VE in adults ≥50 at year 11, showing VE remains high each year after vaccination,
- 73.1% VE in adults aged ≥70 cumulatively from six to 11 years after immunization, showing high VE rates.
In a press release, Dr. Javier Díez-Domingo, Principal Investigator, said, "These final data demonstrate continued protection over more than a decade with high efficacy maintained in both the 50+ and 70+ age groups."
"Infectious diseases like shingles pose a significant risk to adults due to the natural decline in our immune system, and these data represent a remarkable advancement in our understanding of what can be achieved long-term for effective protection against shingles."
Globally, shingles will affect about 30% of people in their lifetimes.
Up to 30% of people experience post-herpetic neuralgia following a shingles rash, a long-lasting nerve pain that can last weeks or months and occasionally persist for several years.
In the U.S., Shingrix was approved by the FDA on October 20, 2017, and is offered at most pharmacies.

According to Quebec's National Institute of Excellence in Health and Social Services (INESSS), there will be an increasing demand for emergency services in 2024, which shows the need for all infants to be protected from Respiratory Syncytial Virus (RSV).
As of April 18, 2024, INESSS recommends BEYFORTUS® to prevent RSV lower respiratory tract disease (LRTD) in all neonates and infants aged eight months.
BEYFORTUS (Nirsevimab-alip) is not a vaccine but is the first approved single-dose, extended half-life monoclonal antibody offering passive immunization in children.
Furthermore, the INESSS Standing Committee on Deliberation—Reimbursement and Access unanimously agrees that BEYFORTUS provides significant clinical benefits compared to placebo in reducing lower respiratory tract infections that require medical assistance and hospitalization due to RSV infection in the healthy, full-term, or premature pediatric population during the first RSV season.
The Committee also recognizes the therapeutic value of BEYFORTUS in the population for whom the risk of developing a serious infection persists for a second RSV season.
Sanofi Canada confirmed it is working with Quebec provincial authorities to make BEYFORTUS available to a broad cohort of infants for the 2024-25 RSV season.
Delphine Lansac, General Manager, Vaccines Canada, Sanofi, stated in a press release, "Parents and physicians who experience the impacts of RSV annually have been waiting for a preventative option that can cover the entire infant population and protect our most vulnerable."
"I believe every baby deserves to be protected against RSV and this recommendation for BEYFORTUS marks an important milestone towards achieving that goal in Quebec. Now is the time to protect all infants against this devastating illness."
Health Canada issued a Notice of Compliance for BEYFORTUS in April 2023. Additionally, it was approved by the U.S. FDA, China, Japan, the European Union, and Great Britain.

GSK today announced positive results from the pivotal phase III trial for gepotidacin, a potential first-in-class oral antibiotic with a novel mechanism of action for uncomplicated urogenital gonorrhea in adolescents and adults.
The study's results showed that gepotidacin (oral, two doses of 3,000mg) was non-inferior, with 92.6% success rates, compared to 91.2% success rates for intramuscular (IM) ceftriaxone (500mg) plus oral azithromycin (1,000mg) combined therapy, a leading combination gonorrhea treatment regimen.
Chris Corsico, SVP of Development, GSK, said in a press release on April 17, 2024, "We are committed to working with health regulators globally to introduce this potential new antibiotic, focusing on solutions that meet critical patient needs."
This announcement is important since the U.S. CDC previously reported that approximately half of the gonorrhea cases each year in the US are resistant to one antibiotic.
Gonorrhea is a sexually transmitted infection caused by bacteria called Neisseria gonorrhoeae, which the World Health Organisation has recognized as a priority pathogen. If inadequately treated, it can lead to infertility and other sexual and reproductive health complications.
Additionally, GSK is developing gepotidacin to potentially treat uncomplicated urinary tract infections (uUTs). If approved, Gepotidacin could be the first uUTI oral antibiotic in over twenty years.
The development of gepotidacin has been funded in whole or in part with U.S. federal funds.
From a prevention perspective, there are no approved gonorrhea vaccines., but a repurposed meningococcal vaccine has been reported effective.
And the is an oral spray UTI vaccine (Uromune™, MV140) being evaluated in 26 countries in 2024.



