Search API
The Chicago Department of Public Health (CDPH) today declared the recent outbreak of measles in the City of Chicago officially over. Two full incubation periods (42 days) have passed without any new measles cases.
On March 7, 2024, CDPH confirmed the first case of measles in Chicago in five years. In total, 64 individuals tested positive for measles, 57 of whom were associated with a shelter setting.
Over 30,000 measles-mumps-rubella vaccine doses have been administered to Chicago residents.
CDPH Commissioner Dr. Olusimbo Ige said in a press release on May 31, 2024, “Our goal is the elimination of measles in Chicago and everywhere, and with proper vaccination coverage, we know that zero is possible.”
For those who are traveling internationally, additional measles vaccinations may be recommended. Talk with your healthcare provider (doctor, nurse, pharmacist) before traveling about vaccinations you and your family may need, wrote CDPH.
As of May 30, 2024, the U.S. CDC reported a total of 146 measles cases in 21 jurisdictions: Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, New York State, Ohio, Pennsylvania, Vermont, Virginia, Washington, West Virginia, and Wisconsin.
There have been 11 outbreaks (three+ cases) reported in 2024.
Globally, measles cases have been confirmed in 52 countries in the past year by the CDC.

Moderna, Inc. today announced that the U.S. Food and Drug Administration (FDA) has approved mRESVIA® (mRNA-1345), an mRNA respiratory syncytial virus (RSV) vaccine, to protect adults aged 60 years and older from lower respiratory tract disease caused by RSV infection.
Stéphane Bancel, Chief Executive Officer of Moderna, commented in a press release on May 31, 2024, "mRESVIA protects older adults from the severe outcomes of RSV infection, and it is the only RSV vaccine available in a pre-filled syringe designed to maximize ease of administration, saving vaccinators' time and reducing the risk of administrative errors."
RSV is a highly contagious seasonal respiratory virus that is a leading cause of lower respiratory tract infections and pneumonia. It causes a particularly large burden of disease in infants and older adults.
Moderna expects to have mRESVIA available for eligible populations by the 2024/2025 RSV season in the U.S. Additionally, Moderna has filed for mRNA-1345 approval with regulators in multiple markets.
As of June 1, 2024, three RSV vaccines and one monoclonal antibody (Beyfortus™) were approved in the U.S.

Valneva SE today announced that the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) has adopted a positive opinion recommending authorization of Valneva's IXCHIQ® single-dose vaccine for the prevention of disease caused by the chikungunya virus in adults.
The European Commission will review the CHMP recommendation, and a decision on the marketing authorization application (MAA) of IXCHIQ in the European Union (EU), Norway, Liechtenstein, and Iceland is expected in the third quarter of 2024.
It will become the first chikungunya vaccine available in the EU under the International Reliance Procedure to address this unmet medical need if approved.
The U.S. Food and Drug Administration approved IXCHIQ in 2023. In February 2024, the U.S. Centers for Disease Control and Prevention (CDC) vaccine committee voted to recommend using IXCHIQ.
Valneva is also preparing an MAA for submission to the U.K. Medicines and Healthcare products Regulatory Agency.
Two additional MAAs are under review by Health Canada and the Brazilian Health Regulatory Agency, with potential approvals in 2024.
Dr. Richard Hatchett, Chief Executive Officer of the Coalition for Epidemic Preparedness Innovations, commented in a press release on May 31, 2024, "Over one billion people live in areas where Chikungunya is endemic, and recent large outbreaks underline the urgent need for safe and effective vaccines against this debilitating disease."
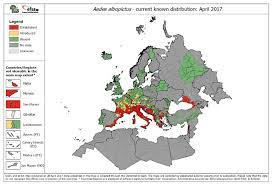
Chikungunya is a mosquito-borne viral disease caused by the chikungunya virus, which is transmitted by Aedes mosquitoes. Infection leads to symptomatic disease in up to 97% of humans four to seven days after the mosquito bite.
According to the U.S. CDC, chikungunya outbreaks have accelerated in 2024.
For example, the CDC recently issued a Level 2 Travel Health Advisory for the Maldives. Local authorities reported elevated chikungunya activity in multiple areas in the Maldives in May 2024.
The Coalition for Epidemic Preparedness Innovations (CEPI) and Bavarian Nordic A/S today announced a partnership to advance the development of Bavarian Nordic's Modified Vaccinia Ankara (MVA-BN®) vaccine (JYNNEOS®, IMVAMUNE®, IMVANEX®) for children in Africa.
On May 30, 3034, CEPI stated it awarded $6.5 million to support a Phase 2 clinical study evaluating the immunogenicity and safety of MVA-BN in children from 2 to less than 12 years of age compared to adults for the prevention of smallpox, mpox, and related orthopoxvirus infections.
This phase 2 clinical trial will be conducted in one or more African countries and is planned to be initiated later in 2024. Notably, the study will also generate evidence on the vaccine in endemic African populations and could potentially support regulatory approval of MVA-BN in endemic countries.
The new trial follows the publication of a continental plan by Africa CDC and African Ministries of Health to strengthen mpox preparedness and response efforts, as well as the World Health Organization's framework for enhancing the prevention and control of mpox.
"We now understand that children suffer disproportionately from mpox, a concerning and neglected disease that has spread rapidly in recent years," said Dr. Richard Hatchett, CEO of CEPI, in a press release.
"To address the risk children face in DR Congo (Clade I) and other areas where the disease is endemic, CEPI is supporting this important trial which will provide key mpox vaccine safety and immunogenicity data in children."
Over 6,500 mpox cases and 345 deaths have been reported in DR Congo in 2024, with children accounting for the majority of infections and deaths. Mpox was initially identified in the DR Congo in 1970.
In 2024, Mpox cases were also confirmed in the Congo, Cameroon, Central African Republic, and Liberia.
The mpox strain behind the current outbreak in Africa, known as Clade I, is estimated to be fatal in around 8-12% of cases. In the U.S., Clade II has been detected since May 2022.
MVA-BN or JYNNEOS is a non-replicating smallpox-mpox vaccine approved in the U.S., and is available at certain clinics and pharmacies in 2024.

CSL Seqirus today announced it was selected by the U.S. Biomedical Advanced Research and Development Authority (BARDA) to complete the fill-and-finish process of the pre-pandemic vaccine for the U.S. government as part of the National Pre-Pandemic Influenza Vaccine Stockpile program.
Under the terms of the agreement revealed on May 30, 2024, CSL Seqirus will deliver approximately 4.8 million doses of a pre-pandemic vaccine well-matched to the H5 of the currently circulating H5N1 strain.
This acquisition of a pre-pandemic vaccine will increase BARDA's vaccine stockpile to support the U.S. government's pre-pandemic response. It is the fourth award CSL Seqirus has received from BARDA in response to sustained highly pathogenic avian influenza activity.
"The U.S. CDC maintains the risk to public health as low. We are closely monitoring the situation because we are acutely aware of the threat that influenza virus strains like H5N1 can pose and take seriously our role in preparedness efforts alongside our government and public health partners," said Marc Lacey, CSL Seqirus, Global Executive Director for Pandemic, in a press release.
"This agreement, building upon prior agreements with BARDA, will help support the U.S. government's ability to respond swiftly if the current avian flu situation changes."
On April 1, 2024, the U.S. Food and Drug Administration (FDA) Dr. Peter Marks informed the media that the U.S. stockpile of avian flu-specific vaccines would work well if deployed.
As of May 2024, FDA-approved avian influenza vaccines are not commercially available in the U.S. The FDA says annual flu shots are unlikely to protect people during avian influenza (bird flu, cow flu) outbreaks.
In Europe, the European Commission (EC) signed a framework contract on July 28, 2022, for the joint procurement of GSK's Adjupanrix, a pandemic influenza vaccine. That contact enables EC Member States to purchase up to 85 million vaccine doses during an influenza pandemic.
BARDA is part of the Administration for Strategic Preparedness and Response within the U.S. Department of Health and Human Services.
CSL Seqirus is a business of Australia-based CSL.

The Coalition for Epidemic Preparedness Innovations (CEPI) and BioNTech SE today announced they are expanding their strategic partnership to contribute to building a sustainable and resilient end-to-end African vaccine ecosystem.
CEPI is committing up to $145 million to support BioNTech's establishment of mRNA vaccine R&D, clinical, and commercial-scale manufacturing capabilities at the Company's facility in Rwanda.
BioNTech and CEPI intend to work jointly to rapidly respond to outbreaks on the African continent caused by known viral threats or an as-yet-unknown pathogen with epidemic or pandemic potential.
Under the terms of the agreement, BioNTech intends to provide affordable access to its prophylactic vaccines, such as those against malaria, mpox, and tuberculosis, manufactured at the Kigali facility.
"Africa still has to import 99% of all the vaccines it needs to protect its people from potentially deadly diseases, meaning many are left waiting far too long to get the life-saving doses they need. This must change ...... said Dr. Richard Hatchett, CEO of CEPI, in a press release on May 30, 2024.
BioNTech and CEPI first announced their strategic partnership in September 2023.

NanoViricides, Inc. today elaborated on its development of a first-in-class, broad-spectrum antiviral agent that could revolutionize the treatment of viral infections, including RSV, Influenza, and other viruses.
Over 90% of human pathogenic viruses are known to use one or more "landing sites" in the Sulfated Proteoglycans ("SPG") family. NanoViricides says a successful host-mimetic nanoviricide drug using SPG as the key feature to attracting viruses could theoretically attack most, if not all, such viruses.
NV-387 is designed to mimic SPG and attack the virus as a cell-mimicking decoy.
For example, in a recent RSV study, extended orally administered NV-387 was compared with a high dose of ribavirin. Two doses were given on the first day of dosing, followed by one daily dose for the next nine days (11 doses). NV-387 given by this dosing regimen led to complete survival of the mice beyond the 21-day study period, with no signs of pathology apparent on the last day of observation.
"An antiviral agent with an extra-ordinary broad spectrum of antiviral activity, coupled with strong safety, is a 'holy grail' of antiviral medicines," said Anil R. Diwan, Ph.D., President and Executive Chairman of the Company, in a press release on May 29, 2024
"Our host-mimetic, direct-acting, nanoviricide™ platform technology capable of destroying virus particles has made this possible, we believe. NV-387 is now ready for Phase II studies towards the goal of regulatory approvals worldwide."
He further commented, "If and when approved, NV-387 could be as revolutionary an antiviral agent as penicillin was as an anti-bacterial agent."

Due to the rise in dengue fever cases in the southern hemisphere this year and the start of the high transmission season in the northern hemisphere, the Pan American Health Organization (PAHO) is urging the Caribbean and Central American countries to enhance preventive measures against this mosquito-borne viral disease.
An Epidemiological Alert announced on May 28, 2024, reported that the Americas region has reported more than 8.1 million suspected dengue cases, a 3.3-fold increase compared to the same period in 2023.
More than 3,600 dengue-related deaths have been reported throughout the region.
Mexico has reported over 65,000 dengue cases, Guatemala over 12,000, Honduras over 20,000, and Panama over 5,800.
Meanwhile, countries and territories in the Caribbean have reported over 21,000 cases, representing a 5.7-fold increase compared to the corresponding period last year.
Previously, the U.S. CDC stated that most dengue cases reported in the 49 continental states occur in travelers infected elsewhere. As of May 2024, travel-related and locally acquired dengue outbreaks were reported in southeast Florida, New York, and Puerto Rico in 2024.
In today's Alert, the PAHO emphasizes the importance of timely clinical diagnosis, early identification of warning signs, and proper patient management to avoid severe cases and deaths.
In most cases, dengue has no symptoms and can present as flu-like. However, when symptoms do occur, they usually include high fever, headache, body aches, nausea and rash.
Although most people recover within one to two weeks, some can develop severe forms that require hospitalization. These can be fatal when not treated promptly and adequately.
Either of the two WHO-listed vaccines can also prevent dengue. Unfortunately, their availability will be limited in 2024.