Search API
NanoViricides, Inc. today elaborated on its development of a first-in-class, broad-spectrum antiviral agent that could revolutionize the treatment of viral infections, including RSV, Influenza, and other viruses.
Over 90% of human pathogenic viruses are known to use one or more "landing sites" in the Sulfated Proteoglycans ("SPG") family. NanoViricides says a successful host-mimetic nanoviricide drug using SPG as the key feature to attracting viruses could theoretically attack most, if not all, such viruses.
NV-387 is designed to mimic SPG and attack the virus as a cell-mimicking decoy.
For example, in a recent RSV study, extended orally administered NV-387 was compared with a high dose of ribavirin. Two doses were given on the first day of dosing, followed by one daily dose for the next nine days (11 doses). NV-387 given by this dosing regimen led to complete survival of the mice beyond the 21-day study period, with no signs of pathology apparent on the last day of observation.
"An antiviral agent with an extra-ordinary broad spectrum of antiviral activity, coupled with strong safety, is a 'holy grail' of antiviral medicines," said Anil R. Diwan, Ph.D., President and Executive Chairman of the Company, in a press release on May 29, 2024
"Our host-mimetic, direct-acting, nanoviricide™ platform technology capable of destroying virus particles has made this possible, we believe. NV-387 is now ready for Phase II studies towards the goal of regulatory approvals worldwide."
He further commented, "If and when approved, NV-387 could be as revolutionary an antiviral agent as penicillin was as an anti-bacterial agent."

Due to the rise in dengue fever cases in the southern hemisphere this year and the start of the high transmission season in the northern hemisphere, the Pan American Health Organization (PAHO) is urging the Caribbean and Central American countries to enhance preventive measures against this mosquito-borne viral disease.
An Epidemiological Alert announced on May 28, 2024, reported that the Americas region has reported more than 8.1 million suspected dengue cases, a 3.3-fold increase compared to the same period in 2023.
More than 3,600 dengue-related deaths have been reported throughout the region.
Mexico has reported over 65,000 dengue cases, Guatemala over 12,000, Honduras over 20,000, and Panama over 5,800.
Meanwhile, countries and territories in the Caribbean have reported over 21,000 cases, representing a 5.7-fold increase compared to the corresponding period last year.
Previously, the U.S. CDC stated that most dengue cases reported in the 49 continental states occur in travelers infected elsewhere. As of May 2024, travel-related and locally acquired dengue outbreaks were reported in southeast Florida, New York, and Puerto Rico in 2024.
In today's Alert, the PAHO emphasizes the importance of timely clinical diagnosis, early identification of warning signs, and proper patient management to avoid severe cases and deaths.
In most cases, dengue has no symptoms and can present as flu-like. However, when symptoms do occur, they usually include high fever, headache, body aches, nausea and rash.
Although most people recover within one to two weeks, some can develop severe forms that require hospitalization. These can be fatal when not treated promptly and adequately.
Either of the two WHO-listed vaccines can also prevent dengue. Unfortunately, their availability will be limited in 2024.

The U.S. Centers for Disease Control and Prevention (CDC) today announced an outbreak of chikungunya in Malé and Hulhumalé regions of Maldives.
Crisis24 recently reported 389 total cases from March to May 11, 2024.
On May 28, 2024, the CDC Level 2 Travel Health Advisory recommended that adults traveling to a destination with a current chikungunya outbreak be vaccinated.
The U.S. FDA recently approved Valneva SE's IXCHIQ® monovalent, single-dose, live-attenuated chikungunya vaccine.
Furthermore, the CDC says if you are pregnant, reconsider travel to Maldives, particularly if you are close to delivering your baby. Mothers infected around the time of delivery can pass the virus to their baby before or during delivery.
According to the CDC, newborns infected in this way or by a mosquito bite are at risk for severe illness, including poor long-term outcomes.
Additionally, people can protect themselves from chikungunya infection by preventing mosquito bites, including using insect repellent, wearing long-sleeved shirts and pants, staying in places with air conditioning, or using window and door screens.

CureVac N.V. today announced the dosing of the first participant in a Phase 2 study of the multivalent seasonal influenza vaccine candidate developed in collaboration with GSK.
The study will assess targeted optimizations for improved immune responses of the messenger ribonucleic acid (mRNA) vaccine candidate against the relevant influenza B strain.
The design of the multivalent vaccine candidate (FLU SV mRNA) has been changed to address all three World Health Organization (WHO)-recommended influenza strains and to exclude the influenza B/Yamagata lineage. The three remaining influenza strains include two influenza A strains and one influenza B strain.
This new Phase 2 study in the joint CureVac/GSK seasonal influenza program was initiated following interim data from the Phase 2 part of the ongoing combined Phase 1/2 study in seasonal influenza, which was reported on April 4, 2024.
Dr. Myriam Mendila, Chief Scientific Officer of CureVac, commented in a press release on May 28, 2024, "Historically, it's been challenging to target influenza B strains with a potent vaccine strategy. We are making progress in adapting and optimizing our clinical approach to address this challenge and improve performance against the remaining B strain."
The companies did not disclose a potential availability date for this new flu shot.
In response to the WHO's decision, various flu shot manufacturers intend to release modified vaccines in time for the 2024-2025 flu season in the United States. Last season, about 158 million flu shots were distributed, which was a decrease from the 2022-2023 flu season's 173 million.

Increased rates of sexually transmitted infections (STIs) are reported globally, and new interventions are needed, wrote researchers in a recent article published by The Lancet Infectious Diseases.
STIs continue to pose significant public health challenges, causing 2.5 million deaths each year, according to a new World Health Organization report.
On May 23, 2024, these France-based researchers wrote, 'We aimed to assess whether post-exposure prophylaxis (PEP) with doxycycline could reduce the incidence of chlamydia or syphilis (or both) and whether the meningococcal group B vaccine (4CMenB) could reduce the incidence of gonorrhea in this population.
Results from the ANRS 174 Doxyvac phase 3 clinical trial concluded Doxycycline PEP strongly reduced the incidence of chlamydia and syphilis.
These researchers said it did not show the efficacy of the 4CmenB vaccine for gonorrhea.
Still, doxycycline PEP should be assessed in other broader populations, and its effect on antimicrobial resistance carefully monitored.

Nationally, outpatient respiratory illness remained stable and is below baseline for the seventh week in a row, according to Key Updates for Week #20 of the 2023-2024 flu season in the United States.
The U.S. Centers for Disease Control and Prevention (CDC) stated on May 24, 2024, that all ten regions are below their region-specific baselines.
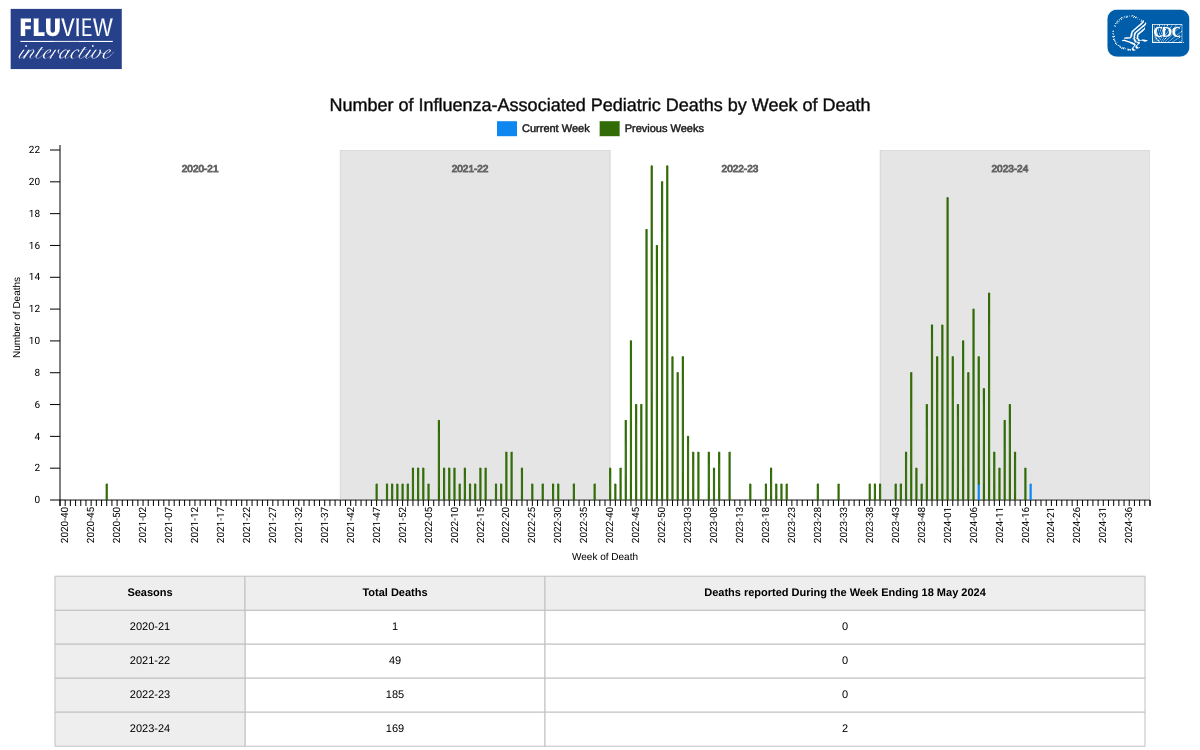
Unfortunately, two influenza-associated pediatric deaths were reported last week, increasing this season's total to 169 pediatric deaths.
Last season, the CDC reported 185 pediatric deaths from influenza infections.
The CDC continues to encourage most children over six months of age to get an annual flu shot, either cell, egg, or nasal, which is offered at most clinics and pharmacies in the U.S.
A new framework was recently released by the World Health Organization (WHO) that will guide health authorities, communities, and other stakeholders in preventing and controlling mpox outbreaks, eliminating human-to-human transmission of the disease, and reducing spillover of the virus from animals to humans.
Mpox is a viral illness caused by the monkeypox virus (MPXV).
There are two different clades of the MPXV: clade I and clade II. Clade I outbreaks are deadlier than clade II outbreaks.
In the United States, clade II cases were reported to have a fatality rate of .002%.
A significant outbreak of the clade I virus in the Democratic Republic of the Congo (DRC) continues today, where cases have been detected for decades. Since the beginning of 2024, over 6,500 cases and 345 deaths have been reported in the DRC.
This data reflects a fatality rate of .05%.
As of May 26, 2024, most U.S. mpox cases continue to be in people who are not vaccinated or have only received one dose of the JYNNEOS® (MVA-BN®, IMVAMUNE®) vaccine. The U.S. CDC recommends that persons at risk for mpox exposure complete the 2-dose vaccination.
In the U.S., the JYNNEOS vaccine is offered at clinics and pharmacies in select cities.


