Search API
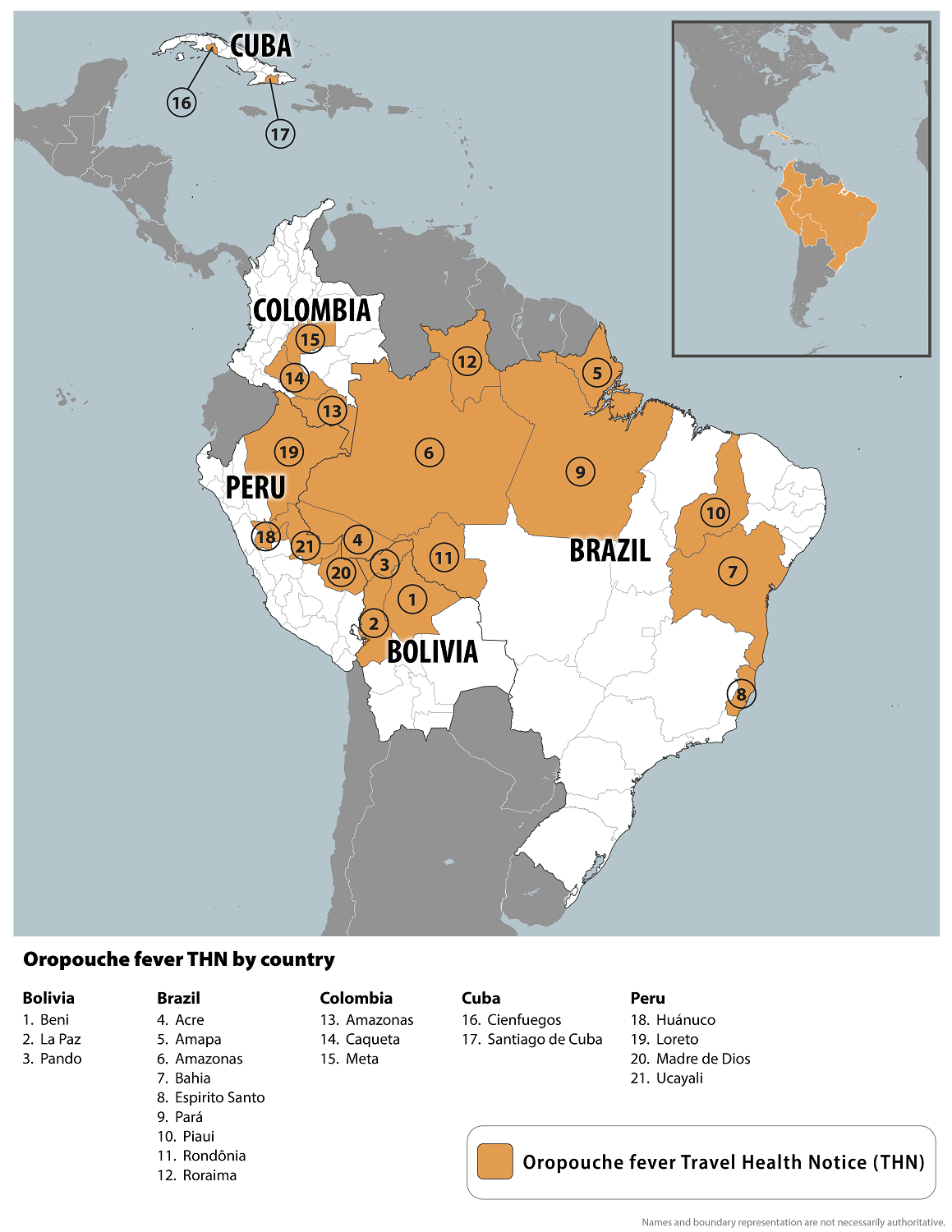
The U.S. Centers for Disease Control and Prevention (CDC) reported today that Oropouche fever outbreaks occur in 21 countries, including parts of Brazil, Bolivia, Colombia, Peru, Cuba, Ecuador, Panama, and Peru.
As of June 5, 2024, the CDC's Travel Health Advirosy says travelers should seek medical care if they develop high fever, headache, muscle aches, stiff joints, nausea, vomiting, chills, or sensitivity to light during or after travel.
Since it was first isolated in Trinidad and Tobago in 1955, more than half a million Oropouche cases and at least 30 major outbreaks have been reported. However, these data are difficult to quantify due to the lack of diagnosis.
In 2024, the Pan American Health Organization reported over 5,000 confirmed cases of Oropouche in four countries in the Region of the Americas.
This illness can occur in people of any age and is often mistaken for dengue, which is also impacting these populations.
The CDC says Oropouche fever is spread by the bite of infected midges (small flies) and mosquitoes.
Unfortunately, Oropouche infection treatment is supportive, as no specific medications or vaccines are available.
The U.S. Centers for Disease Control and Prevention (CDC) published clinical guidelines on counseling patients regarding doxycycline post-exposure prophylaxis (doxy PEP) for bacterial sexually transmitted infection (STI) prevention.
Doxycycline, a broad-spectrum tetracycline antimicrobial, is well absorbed and tolerated, with a half-life of approximately 12 hours.
As of June 4, 2024, the CDC says Doxy PEP has proven to reduce the risk of getting bacterial STIs, specifically syphilis, chlamydia, and gonorrhea.
The CDC recommends healthcare providers discuss doxy PEP with all gay, bisexual, and other men who have sex with men and transgender women with a history of at least one bacterial STI in the last 12 months. If offering doxy PEP, healthcare providers should prescribe self-administration of 200 mg of doxycycline within 72 hours of sex.
Laura Bachmann, MD, MPH, FIDSA, FACP, Acting Director, Division of STD Prevention, stated in a media release, 'Doxy PEP represents the first new STI prevention tool in decades, at a time when innovation in the nation's fight nation's STIs is desperately needed."
As of June 5, 2024, bacterial STI vaccine candidates are conducting clinical research.
Recently, the Bexsero® meningitis B vaccine (4CMenB) has shown some protection against gonorrhea. Studies have found that people who receive two doses of Bexsero maybe 33–40% less likely to be diagnosed with gonorrhea than those who don't.
In the U.K., meningococcal vaccination is now advised for certain people to prevent STIs.

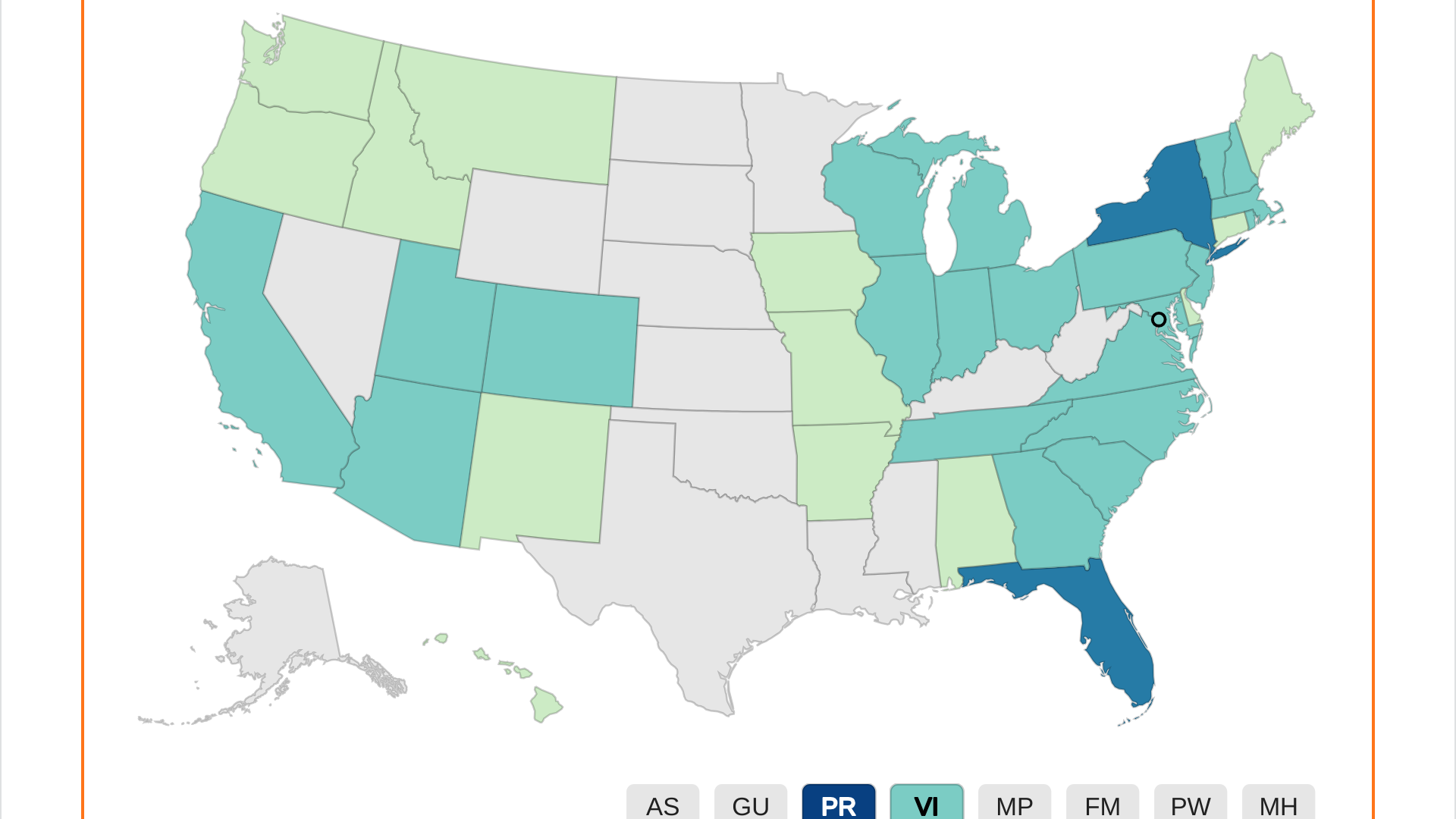
The Centers for Disease Control and Prevention (CDC) says most dengue fever cases in the United States occur in areas where dengue is common, such as U.S. territories and a few states. Dengue virus is found in many tropical parts of the world, including the Caribbean, Central, and South America.
As of June 5, 2024, the CDC has reported over 100 additional dengue cases over the last month, which has increased this year's total to 1,706.
As of week #19 in 2024, Puerto Rico reported the most dengue cases, 1,107, with San Juan reporting 528 of these cases. In 2023, Puerto Rico reported 1,242 dengue cases.
Florida recently confirmed 198 travel-associated dengue cases in 2024, mainly by visitors from Brazil and Cuba. Seven cases of locally acquired dengue were reported from Miami-Dade and Pasco counties.
Additionally, the CDC reported New York's dengue outbreak has reached 119 cases in 2024.
Since the state of Texas has yet to post its dengue cases count for 2024, the CDC's overall total is expected to significantly increase. In 2023, Texas 67 travel-related dengue cases.
Dengue fever is a mosquito-borne, vaccine-preventable disease caused by the dengue virus. However, the WHO-approved dengue vaccines are not commercially offered in the U.S.
NeoImmuneTech, Inc. today announced that the European Medicines Agency (EMA) has granted Orphan Drug Designation (ODD) to NT-I7 for the treatment of Acute Radiation Syndrome (ARS).
This regulatory milestone follows the ODD granted to NT-I7 by the U.S. FDA for the same indication in November 2023.
ARS is a critical condition resulting from a high dose of radiation exposure, causing severe, sometimes fatal damage to the bone marrow and the immune system. No treatments are available that effectively promote T-cell recovery after such exposure.
NT-I7, a novel long-acting human interleukin-7 (IL-7), has shown promise to accelerate T cell reconstitution and enhance the immune response. It offers a potential solution for this unmet medical need. Clinical studies have shown that NT-I7 significantly boosts T cell counts while maintaining high safety and tolerability.
Luke Oh, Ph.D., President and Chief Executive Officer of NeoImmuneTech, said in a press release on June 4, 2024, "We are thrilled to see the deep interest of the scientific and regulatory community around the potential use of NT-I7 as a medical countermeasure in ARS."
"It is an important acknowledgment of the potential that NT-I7 holds in providing a beacon of hope for the treatment of ARS."
Examples of people who suffered from ARS are individuals exposed during the Hiroshima and Nagasaki atomic bombings and the Chernobyl Nuclear Power Plant incident firefighters.
NeoImmuneTech is actively developing NT-I7 in ARS through partnerships with the National Institute of Allergy and Infectious Diseases (NIAID) and Duke University. Recently, Duke University secured a $6 million grant from NIAID for NT-I7 development in ARS.

The Vaccines and Related Biological Products Advisory Committee (VRBPAC) will meet in an open session on June 5, 2024, to discuss and recommend selecting the 2024- 2025 Formula for COVID-19 vaccines.
VRBPAC has met multiple times since 2022 to discuss the selection of the Formula for COVID-19 vaccines. The U.S. FDA Briefing Document and Agenda for this new meeting were recently posted online.
The FDA has approved two COVID-19 vaccines for active immunization to prevent COVID-19 caused by SARS-CoV-2 in individuals 12 and older. In addition, the FDA currently authorizes three vaccines for use in the U.S. under emergency use authorization.
The U.S. COVID-19 emergency declaration was withdrawn on May 11, 2023.
Available data suggest that the current formula of COVID-19 vaccines should be updated for the anticipated 2024–2025 respiratory virus season in the U.S.
Based on the review of virus epidemiology data indicating the recent dominance of the JN.1 sublineage and data from post-monovalent XBB.1.5 human sera indicating a drop in neutralizing antibody responses against JN.1, the World Health Organization Technical Advisory Group on COVID-19 Vaccine Composition recommended that a monovalent JN.1 lineage component be included in the composition of COVID-19 vaccines (2024-2025 Formula).
This recommendation was made on April 26, 2024, before the dominance of the KP.2 sublineage in the U.S.
Initial neutralization data of various vaccine candidates are now available for both the JN.1 and KP.2 sublineages and will be presented along with current SARS-CoV-2 epidemiologic data for VRBPAC’s consideration.
To digitally attend this meeting, visit this YouTube link tomorrow: https://youtube.com/live/weaKQiFk_98

In a historic step towards mitigating the high incidence of malaria in South Sudan, the first consignment of the R21/Matrix-M™ vaccine malaria vaccine recently arrived in Juba.
The Ministry of Health received over 645,000 doses, which will be distributed to 28 counties.
South Sudan is grappling with one of the highest malaria incidence rates in the African region. In 2022, South Sudan had an estimated 2.8 million cases and 6,680 deaths.
“We are committed to reducing the impact of malaria and improving the health outcomes for our children,” said Honourable Yolanda Awel Deng, Minister of Health, in a UNICEF press release on May 31, 2024,
“The continued use of this vaccine, alongside other preventive measures such as insecticide-treated bed nets and timely access to medical care, will be instrumental in our efforts to eliminate malaria in South Sudan.”
With support from Gavi, UNICEF is working to procure enough malaria vaccines to immunize over 45 million children worldwide in the coming years.
As of June 3, 2024, malaria vaccines are not offered in the United States.