Search API
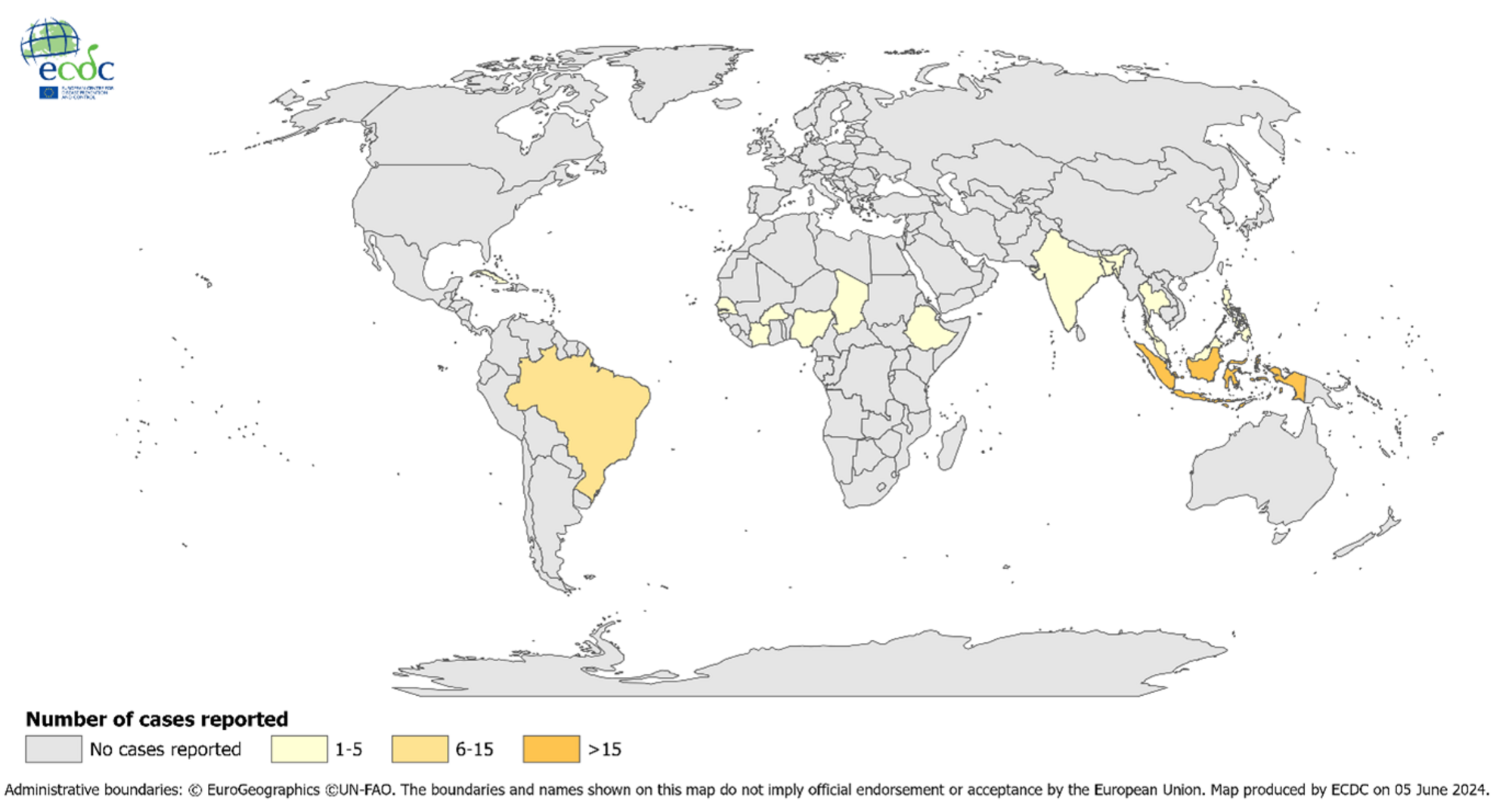
In the WHO Eastern Mediterranean Region, dengue outbreaks continue to be reported in 2024. The Ae. aegypti and some Ae. albopictus dengue virus-carrying mosquitoes have been identified in most of the countries in this region.
On July 17, 2024, the WHO Disease Outbreak News reported 12 autochthonous (local) cases of dengue documented in Iran, all of which were reported in Bandar-Lengheh, Hormozgan Province.
Additionally, there have been 137 travel-related dengue cases in 2024.
Iran reported an average of 20 imported dengue cases annually between 2017 and 2023.
Furthermore, WHO does not recommend any general travel or trade restrictions in Iran based on the available information.
The WHO recommends that vaccination against dengue be part of an integrated strategy to control the disease, including vector control, proper case management, community education, and community engagement.
WHO recommends that countries consider introducing the second-generation QDENGA® (TAK-003) vaccine into their routine immunization programs in locations where high transmission intensity of dengue poses a significant public health problem.
WHO does not currently recommend the programmatic use of TAK-003 in young children.
As of July 22, 2024, the QDENGA vaccine is not authorized for use in the United States.

The U.S. government recently exercised a procurement option to enhance orthopoxvirus preparedness against mpox and smallpox outbreaks.
On July 19, 2024, SIGA Technologies, Inc. announced that the U.S. Department of Health and Human Services (HHS) ordered the delivery of approximately $113 million of oral TPOXX® (tecovirimat) treatment courses.
“Building on the orders received in 2023 from the U.S. government and 15 international customers, this $113 million order from the U.S. government will enhance orthopoxvirus preparedness and support sizable and consistent action when needed to help ensure public health from natural, accidental, or intentional threats,” said Diem Nguyen, Chief Executive Officer, in a press release.
TPOXX is an antiviral medicine approved by the U.S. Food and Drug Administration (July 2018) specifically for treating smallpox disease in adults and pediatric patients weighing at least 13 kg.
Following U.S. approval, Health Canada also authorized TPOXX for the treatment of mpox and smallpox and authorized in Europe and the UK to treat smallpox, mpox, cowpox, and vaccinia complications.
As of July 22, 2024, mpox vaccines were also approved by the U.S. FDA and are available in the United States, Canada, and various countries.

With over 24,600 Zika virus cases already confirmed in the Region of the Americas in 2024, a new study published by the journal eBioMedicine, part of The Lancet, disclosed new, unsettling insights.
The Cleveland Clinic announced that this study revealed that maternal Zika virus infections can reprogram fetal immune development, leading to long-term consequences in children's immunity.
On July 18, 2024, the Clinic stated that these changes may occur in children born without the physical characteristics associated with congenital Zika syndrome, such as microcephaly.
This finding suggests that 95% of babies born from Zika-infected pregnancies who did not exhibit symptoms may have been affected by the virus with long-term immunological repercussions.
Additionally, heightened inflammation was observed in Zika-exposed infants with abnormalities at birth, while children exposed to Zika later maintained a chronic Th1-biased immune profile. The impaired response to Th2-biased vaccines raises concerns about the lasting effects of Zika virus exposure on immune responses.
Suan-Sin (Jolin) Foo, PhD, an expert in maternal-fetal virology and the Zika virus, says babies without symptoms are deemed healthy and do not receive any follow-up medical care or attention.
“Studies have only really focused on what’s happening with the children who were born with visible physical conditions like microcephaly or neurological complications,” Dr. Foo commented in a press release.
“The rest of these kids may not even have a note on their chart mentioning that their mother was infected during pregnancy. Unless they’re part of our study, they’re essentially lost to the medical field.”
Dr. Foo added, “Our study clearly shows there’s much more to this condition than meets the eye. We need to expand diagnostic criteria and conduct more research to ensure these immunologically vulnerable children get the necessary care.”
From a prevention perspective, no Zika vaccine candidate has been approved by the U.S. FDA as of July 2024.

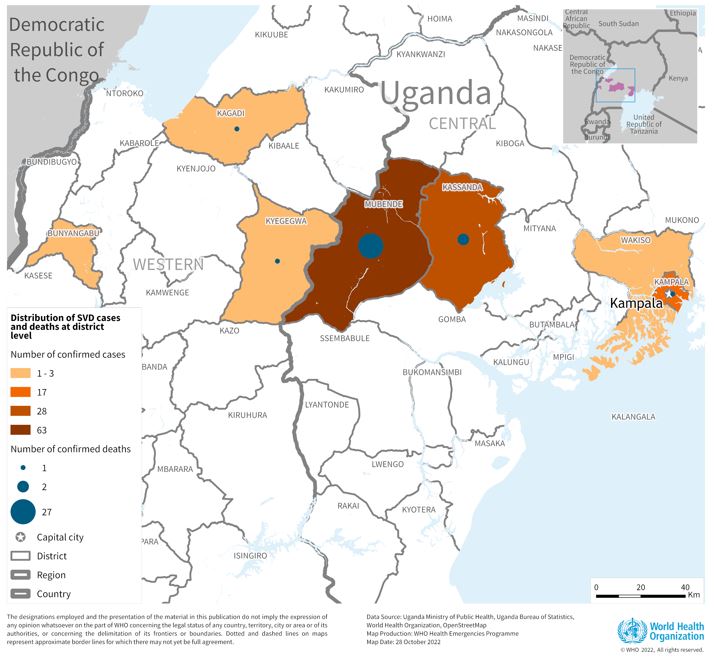
The Sabin Vaccine Institute recently announced the launch of a Phase 2 clinical trial for its vaccine against Sudan ebolavirus at Makerere University Walter Reed Project (MUWRP) in Uganda.
This is a vital development as there are currently no approved vaccines for this strain of ebolavirus.
Based on the cAd3 platform, Sabin’s single-dose investigational Sudan ebolavirus vaccine was found to be promising in Phase 1 clinical and non-clinical studies. Results showed it to be safe while eliciting rapid and robust immune responses that lasted up to 12 months.
“We are delighted to advance a vaccine candidate that can thwart a deadly and devastating disease, especially one that caused a fairly recent outbreak and for which no approved treatments exist,” commented Amy Finan, Sabin’s Chief Executive Officer, in a press release on July 15, 2024.
“Sabin’s vaccine candidate is backed by strong safety and immunogenicity data, and we hope this trial will yield further evidence to move the vaccine closer to licensure.”
This is Sabin’s second Phase 2 clinical trial partnership with MUWRP, based in Uganda’s capital, Kampala. A Phase 2 trial for a Marburg vaccine is already underway, having recently completed enrollment. Initial results from the Marburg trial are expected later this year.
The most recent outbreak of Sudan ebolavirus occurred in Uganda in the fall of 2022. That outbreak ultimately resulted in 55 deaths.
Sabin’s vaccine candidate was the first to arrive in Uganda during that outbreak after the WHO included it as one of three vaccines for possible use in an outbreak trial. The outbreak ended before the vaccine was deployed.
In August 2019, Sabin announced agreements with GSK to advance the development of vaccines against the Zaire and Sudan ebolavirus and Marburg virus. The three candidate vaccines were initially developed collaboratively by the U.S. National Institutes of Health and Okairos, acquired by GSK in 2013.
As of July 20, 2024, the U.S. FDA has approved Zaire Ebolavirus vaccines, which have been offered in Africa since 2019.
According to a post on X, the Ministry of Health of the Republic of Belarus recently joined Bosnia and Herzegovina by authorizing a lung cancer vaccine.
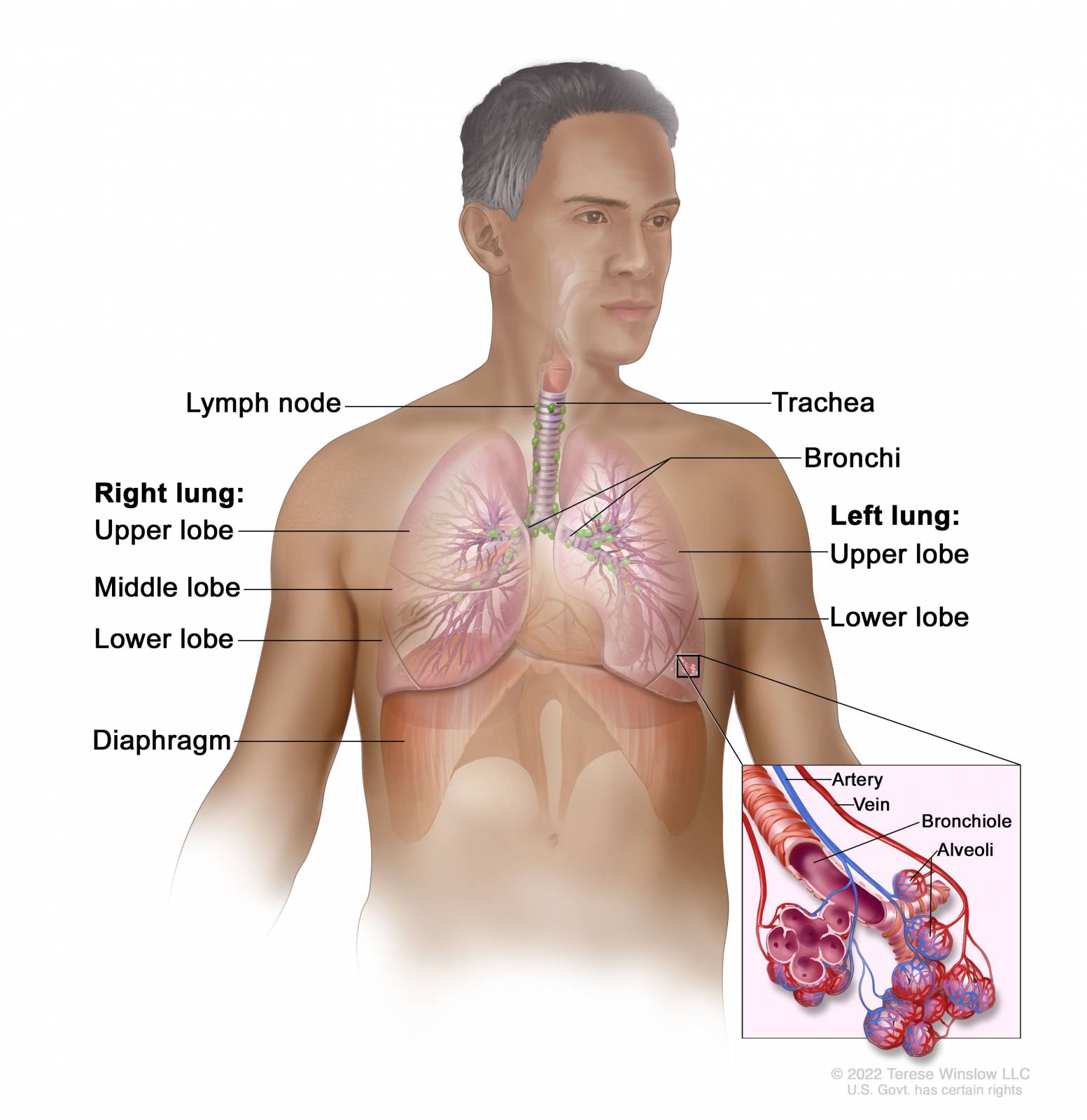
On July 12, 2024, the Prensa Latina news agency reported that the CimaVax-EGF vaccine was the first patented and registered therapeutic vaccine against non-small-cell lung carcinoma (NSCLC).
CimaVax-EGF is a recombinant human EGF-rP64K/montanide ISA 51 vaccine that completed a phase 4 clinical trial for NSCLC in 2017 and is approved as a "maintenance treatment for patients with stage IIIB/IV NSCLC.
Developed by Cuba's Center of Molecular Immunology in 2011, the CimaVax-EGF vaccine has been deployed in Cuba and the South American countries of Colombia, Peru, and Paraguay.
This vaccine is not U.S. FDA-approved nor available to U.S. citizens.
However, a Phase 1/2 clinical trial sponsored by Roswell Park Cancer Institute is ongoing. This study says CIMAvax, combined with nivolumab or pembrolizumab, may better treat patients with NSCLC or squamous head and neck cancer.
The U.S. National Cancer Institute says each type of non-small cell lung cancer has different kinds of cancer cells. The cancer cells of each type grow and spread in various ways. The types of non-small cell lung cancer are named for the kinds of cells found in the cancer and how the cells look under a microscope.
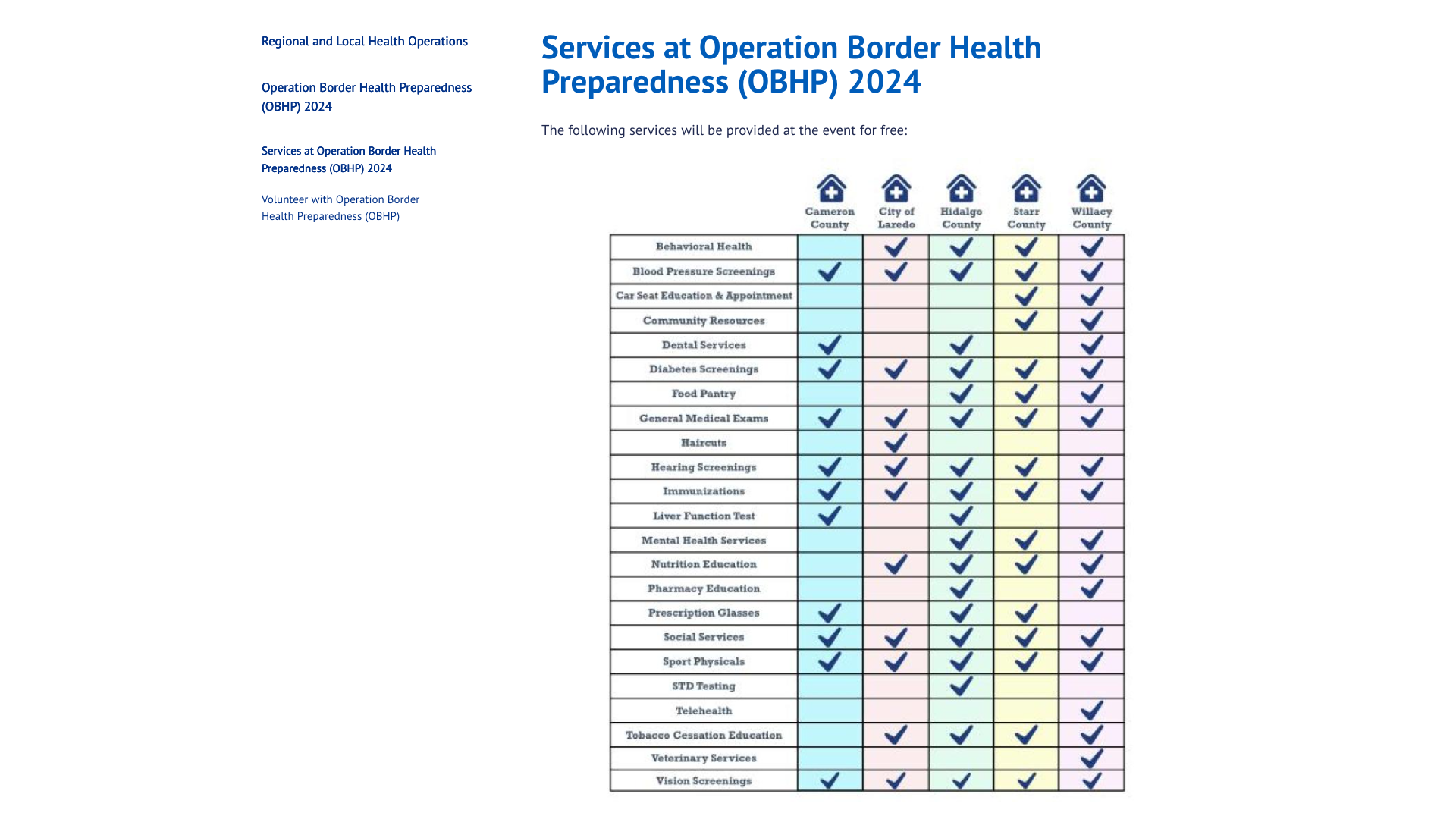
The Texas Department of State Health Services today announced it celebrates the 25th anniversary this month of the Operation Border Health Preparedness (OBHP) exercise, with no-cost health clinics planned at five different locations for South Texas residents to utilize.
These are essential services as Texas is currently reporting increases in diseases such as Dengue (16).
Services vary from location to location, so visit Services at OBHP 2024 or call 2-1-1 to confirm which services are offered in each specific area.
In 2023, OBHP provided 27,427 health services to 6,641 patients, including about 4,000 immunizations during the exercise.
“DSHS is extremely proud to celebrate this milestone with our partners and the communities that have embraced this exercise for a quarter of a century,” said DSHS Commissioner Jennifer Shuford, MD, MPH, in a press release on July 18, 2024.
“Services available to residents are extensive, and the experience gained by communities and emergency planners will help with disaster preparation and response in the future.”
DSHS is partnering with OBHP in 2024 with Hidalgo County Health and Human Services, Cameron County Public Health, Willacy County, Starr County, Laredo Public Health, Texas Military Department, Texas State Guard, Texas A&M University, local nursing schools, and other nonprofit groups.
As the global Chikungunya outbreak continues in July 2024, a second vaccine may soon become available.
This is essential news since the World Health Organization recently confirmed the mosquito-borne viral Chikungunya virus was identified in nearly 115 countries in 2024, primarily in the Region of the Americas.
Bavarian Nordic A/S today announced that the European Medicines Agency (EMA) has validated the marketing authorization application (MAA) submitted in June 2024 for CHIKV VLP, the Company’s vaccine candidate for immunization to prevent disease caused by chikungunya virus infection in individuals 12 years of age and older.
Validation of the MAA begins the EMA’s centralized review procedure under accelerated assessment.
The accelerated assessment, granted by EMA’s Committee for Medicinal Products for Human Use in February 2024, aims to reduce the timeframe for the CHMP to review an MAA. This could support the European Commission's vaccine approval in the first half of 2025.
Bavarian Nordic also completed the submission of a Biologics License Application for the CHIKV VLP vaccine to the U.S. Food and Drug Administration (FDA) in June 2024, potentially also supporting the approval of the vaccine in the first half of 2025.
CHIKV VLP is an adjuvanted VLP-based vaccine candidate for active immunization to prevent disease caused by CHIKV infection.
“The MAA submission and review marks a pivotal milestone for Bavarian Nordic in 2024....,” said Paul Chaplin, President and CEO of Bavarian Nordic, in a press release on July 18, 2024.
In November 2023, the U.S. FDA approved Valneva SE's monovalent, single-dose, live-attenuated IXCHIQ® Chikungunya vaccine. It has been available in the U.S. since the beginning of 2024.