Search API
Throughout 2024, the Florida Department of Health has reported various mosquito-transmitted diseases infecting people. Florida has confirmed that 14 species of Anopheles mosquitoes transmit diseases to humans.
While Dengue fever gets most of the media headlines, diseases such as Chikungunya, Malaria, and West Nile virus have also been detected this year.
For example, on August 5, 2024, a locally acquired case of West Nile Virus was confirmed in Broward County.
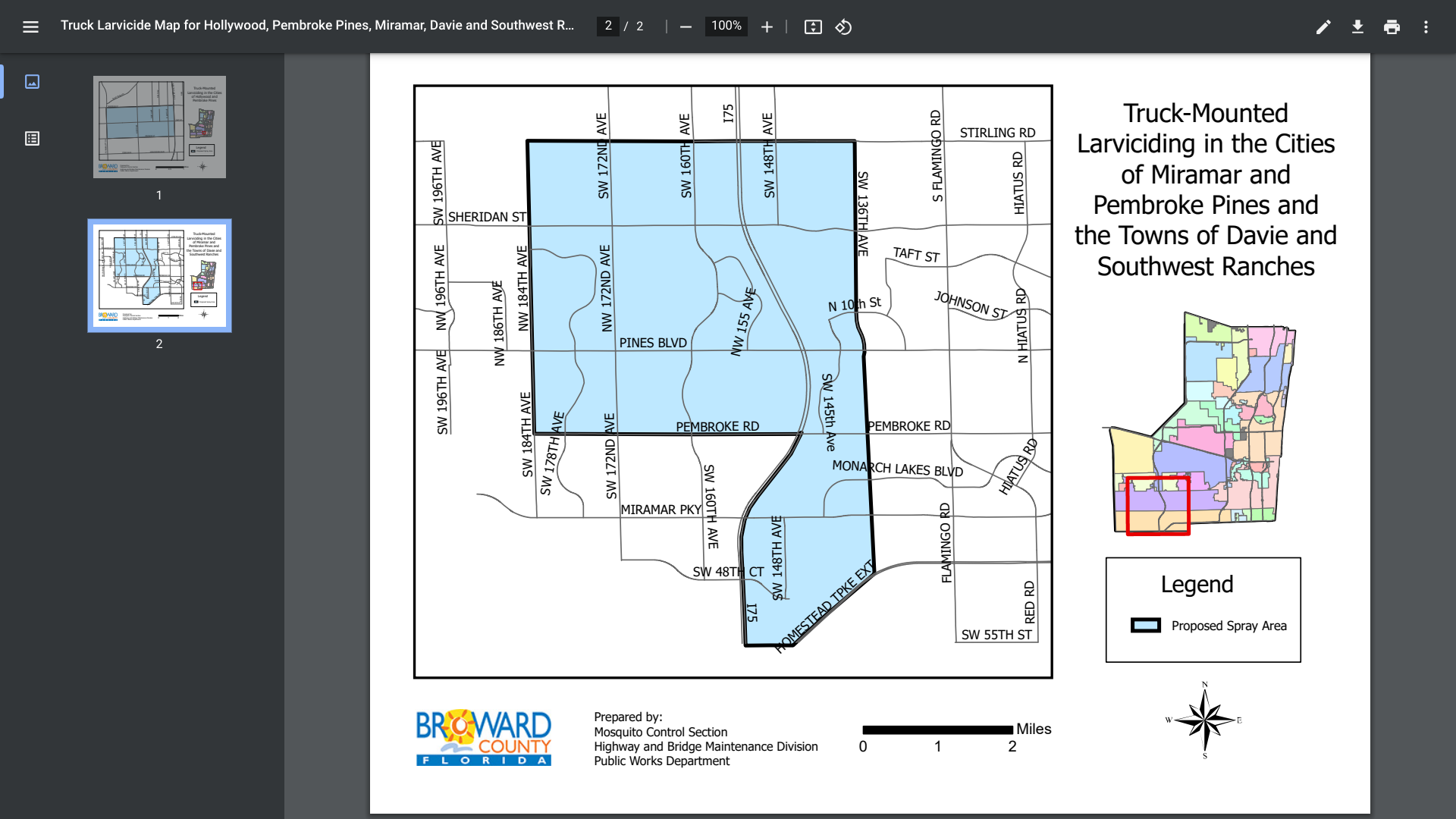
As a direct response, the Broward County Mosquito Control Section recently announced it would spray organic larvicide as part of an integrated pest management approach. Truck-mounted larviciding will be performed between August 5 - 22, 2020.
This month, portions of Hollywood, Pembroke Pines, Davie, and Southwest Ranches are being targeted in southeast Florida.
The larvicide used is VectoBac WDG, which is not harmful to humans, pets, bees, aquatic habitats, or environmentally sensitive areas. The active ingredient is Bacillus thuringiensis israelensis (Bti, strain AM6552), a naturally occurring, biodegradable bacterial mosquito larvicide.
Broward County Mosquito Control Section continues to work closely with the Florida Department of Health and Code Enforcement partners in Broward's 31 municipalities to reduce the population of mosquitoes and their habitats. Any Broward County resident experiencing mosquito problems can request service by calling 311.
Regarding disease prevention, the U.S. Centers for Disease Control and Prevention (CDC) recently recommended Valneva SE's IXCHIQ®, a monovalent, single-dose, live-attenuated chikungunya vaccine. Vaccination is advised for international travelers since five chikungunya cases with onset in 2024 have been reported in individuals with a travel history to Brazil.
As of August 10, 2024, the CDC has not issued vaccination requirements for Florida residents or visitors.
The Oregon Health Authority (OHA) recently alerted health providers regarding the ongoing community measles virus transmission. In its latest update, the OHA reported 26 confirmed cases, all involving unvaccinated people.
As of August 8, 2024, 27 jurisdictions had reported 211 measles cases to the U.S. CDC. And 45% of these cases were hospitalized for isolation or for management of measles complications.
For all of 2023, the CDC reported 59 measles cases in 20 jurisdictions.
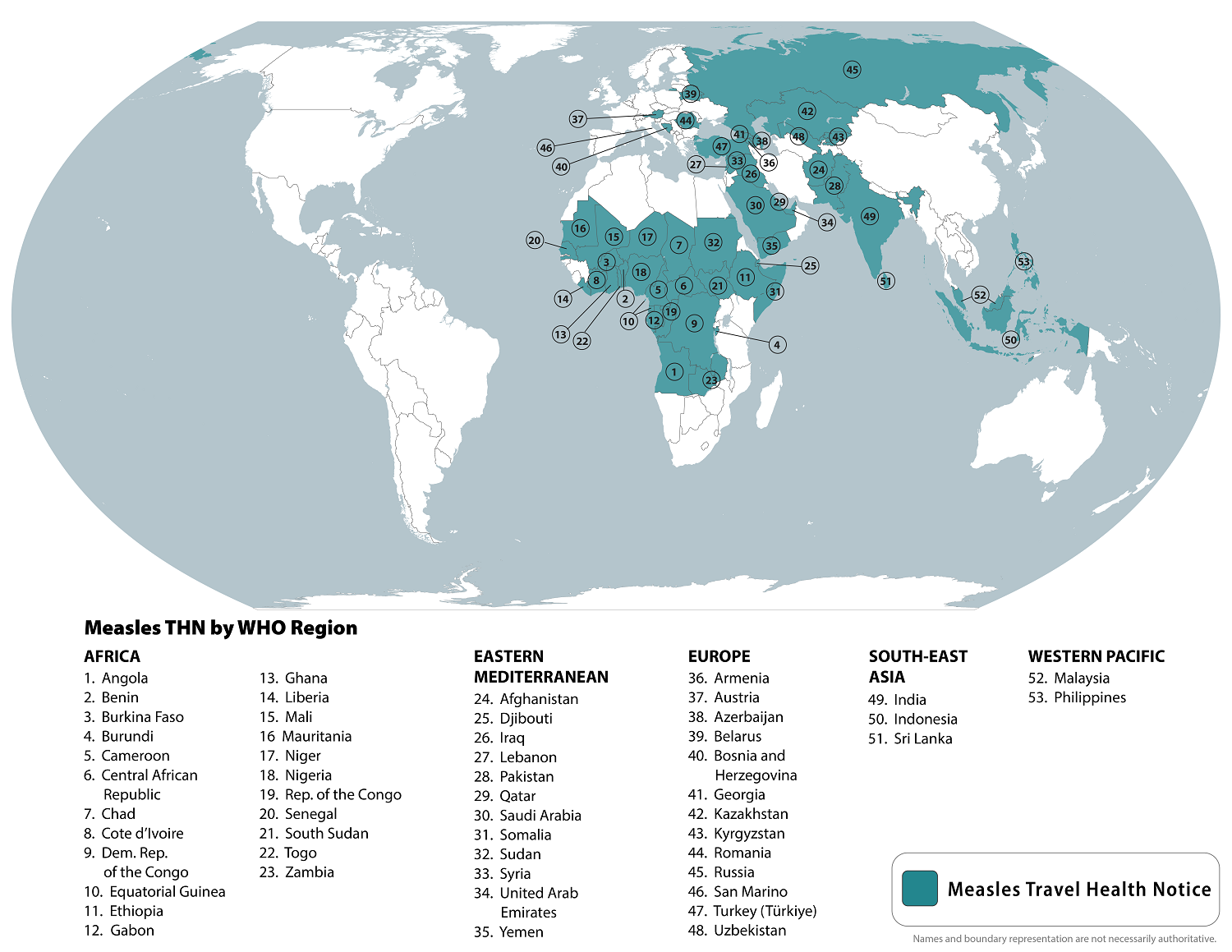
Did you know that measles is a health risk while traveling?
The CDC republished a global Watch-Level 1, Practice Usual Precautions, Travel Health Notice in late May 2024, identifying measles outbreaks in 53 countries.
The CDC recommends evaluating your family's need for early vaccine doses before any international travel. Measles vaccines are generally available at clinics and pharmacies in the U.S.
After you return from a flight, monitor your health for three weeks and call your healthcare provider if you or your child get sick with a rash and fever.
The European Centre for Disease Prevention and Control (ECDC) today alerted travelers and clinicians today about the risk of Oropouche virus disease, a zoonotic disease caused by the Oropouche virus (OROV).
The ECDC's Threat Assessment, published on August 9, 2024, reported that during June and July 2024, 19 imported cases of Oropouche virus disease were reported for the first time in EU countries: Spain (12), Italy (5) and Germany (2).
Eighteen of these cases had a travel history to Cuba and one to Brazil.
The principal vector (Culicoides paraensis midge) is widely distributed across the Americas but is absent in Europe. There has been a lack of evidence as to whether European midges or mosquitoes could transmit the virus.
In 2024, outbreaks of OROV disease were reported in several countries across South America, Central America, and the Caribbean.
The ECDC says this health risk is moderate for people traveling to or living in epidemic areas in South America, Central America, and the Caribbean.
However, it noted that the risk is higher for those visiting heavily affected areas, including Brazil's northern states and the Amazon region, and for those who don't take adequate protective measures.
Oropouche virus disease can manifest as an acute febrile illness with headache, nausea, vomiting, muscle and joint pains, and occasionally more severe symptoms. The prognosis for recovery is good, and fatal outcomes are infrequent.
Recently, the Brazilian Ministry of Health reported six possible cases of OROV disease being passed from mother to child during pregnancy. The potential risk during pregnancy and fetopathic effects of OROV infection are still under investigation and have not been confirmed.
Furthermore, horizontal, human-to-human virus transmission has not been documented.
The ECDC says areas affected by OROV, such as Brazil, are also classified with current or previous Zika virus (ZIKV) transmission. Therefore, travel advice for pregnant women combines ZIKV and OROV warnings.
Unfortunately, there are no vaccines to prevent OROV or Zika diseases.

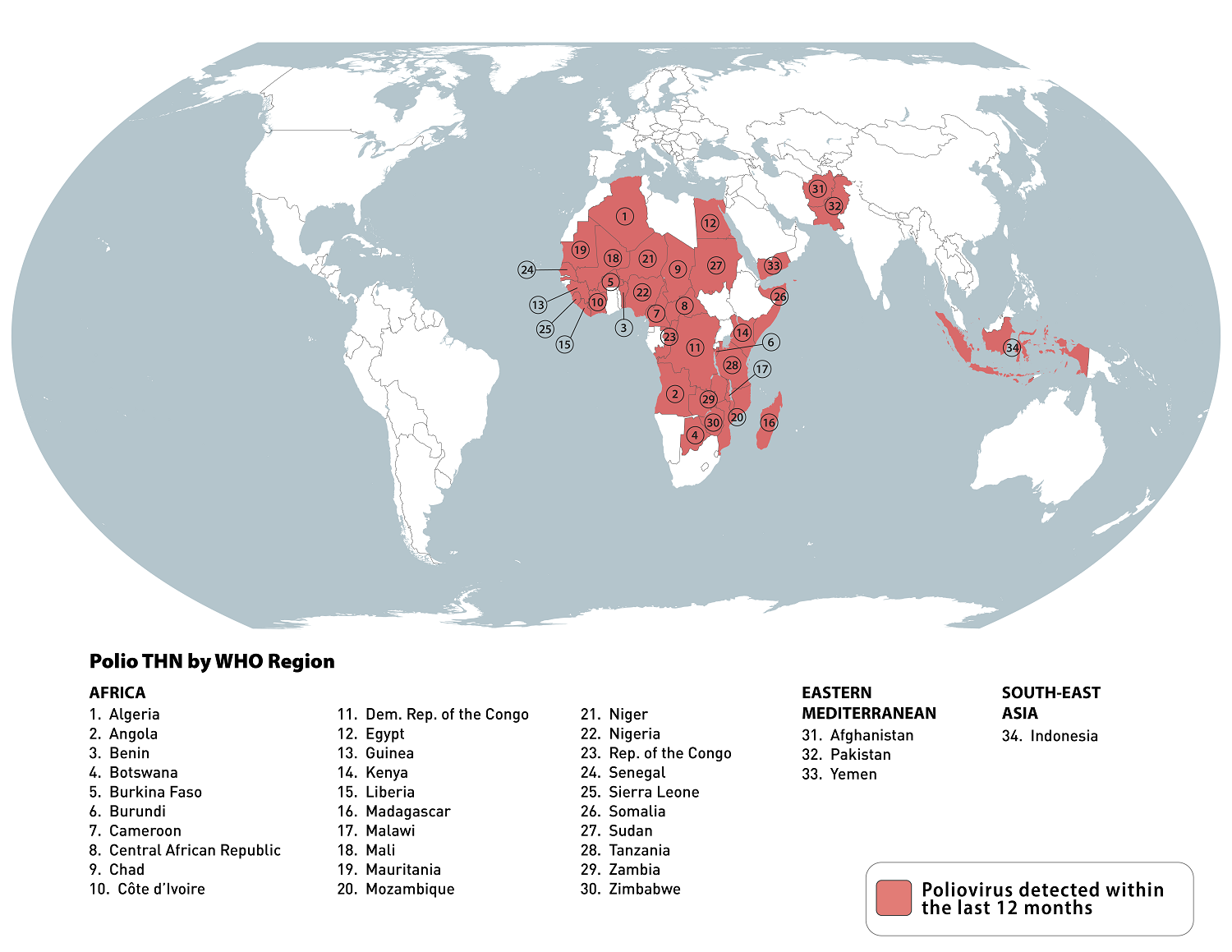
According to the weekly update from the Global Polio Eradication Initiative (GPEI), six countries reported poliovirus cases, including Afghanistan and Pakistan, with additional wild poliovirus type 1 (WPV1) cases.
The GPEI says both countries have already doubled the cases they reported in 2023.
As of August 7, 2024, Afghanistan reported two new WPV1 cases, bringing its total to 11.
Pakistan reported three more cases, increasing its total to 12 for 2024.
Four African countries reported cases involving circulating vaccine-derived poliovirus type 2 (cVDPV2).
The Democratic Republic of the Congo reported two cVDPV2 cases. Ethiopia reported one case, boosting its total to 12. Nigeria reported one case, elevating its total to 38, and South Sudan reported its 7th cVDPV2 case for 2024.
The U.S. CDC says most people with polio do not feel sick. Some people have only minor symptoms, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the arms and legs.
In rare cases, polio infection causes permanent loss of muscle function.
Polio can be fatal if the breathing muscles are paralyzed or if the brain is infected.
Furthermore, the CDC recommends that adults who previously completed the full, routine polio vaccine series may receive a single, lifetime booster dose of polio vaccine before traveling to any destination reporting polio cases. Polio vaccines are generally available at health clinics and pharmacies in the U.S.
HilleVax, Inc., a company focused on developing and commercializing novel vaccines, announced financial results for the June 30, 2024 quarter and highlighted recent progress.
As of June 30, 2024, and December 31, 2023, the company had cash, cash equivalents, and marketable securities totaling $245 million and $303.5 million, respectively.
On August 8, 2024, the company confirmed it is exploring the potential for continued development of its HIL-214 and HIL-216 norovirus vaccine candidates in adults.
However, the company has discontinued further development of HIL-214 in infants.
This is unfortunate news since no U.S. FDA-approved norovirus vaccines are available to meet disease prevention needs.
The U.S. CDC recently reported norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis among people of all ages and causes 58% of foodborne illnesses acquired in the United States.
Each year, there are about 2,500 reported norovirus outbreaks in the U.S., including on cruise ships.

According to the World Health Organization (WHO), the global Dengue fever outbreak continues to expand in August 2024.
Dengue outbreaks are being reported by 90 countries in 2024, with most of these cases reported in the Region of the Americas.
As of August 8, 2024, 43 countries and territories in the Region have reported over 11.1 million Dengue cases and about 6,135 related deaths this year.
The updated data is over 120% greater than recorded throughout 2023.
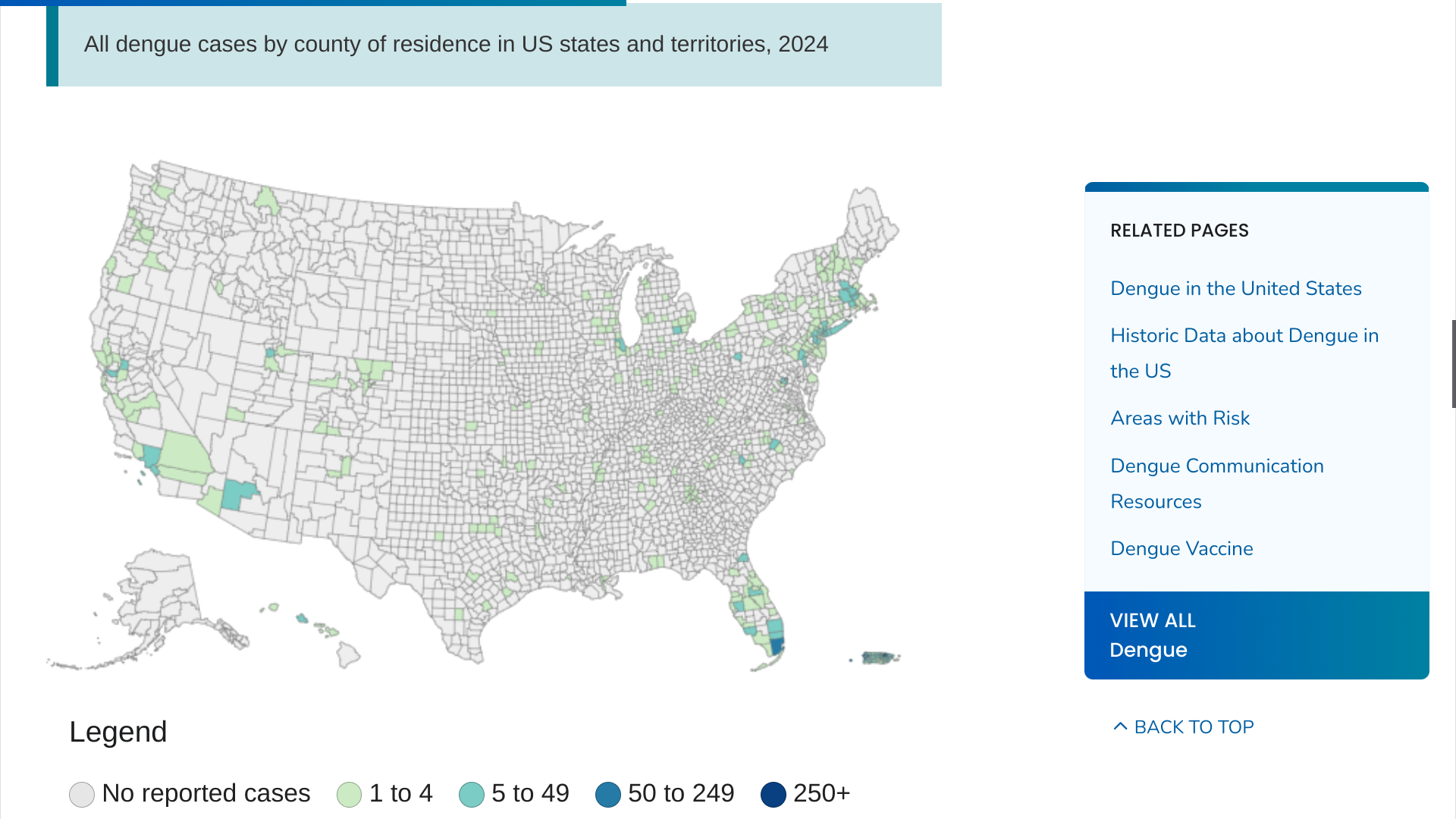
In the United States, the U.S. CDC reported on August 7, 2024, that 52 jurisdictions, led by Florida, New York/New Jersey, and Puerto Rico, had confirmed 3,290 dengue cases.
In 2023, only 2,343 Dengue cases were reported to the CDC.
The CDC says Dengue is endemic in the U.S. territories of Puerto Rico, American Samoa, the U.S. Virgin Islands, the Federated States of Micronesia, the Republic of Marshall Islands, and the Republic of Palau.
Currently, the CDC says the best way to prevent this mosquito-transmitted disease is to wear protective clothing, as no Dengue vaccine is available in the U.S.
However, in 2024, Takeda's QDENGA® (TAK-003) two-dose vaccine is available in over 20 countries. The WHO added QDENGA to its List of Prequalified Vaccines effective May 9, 2024.
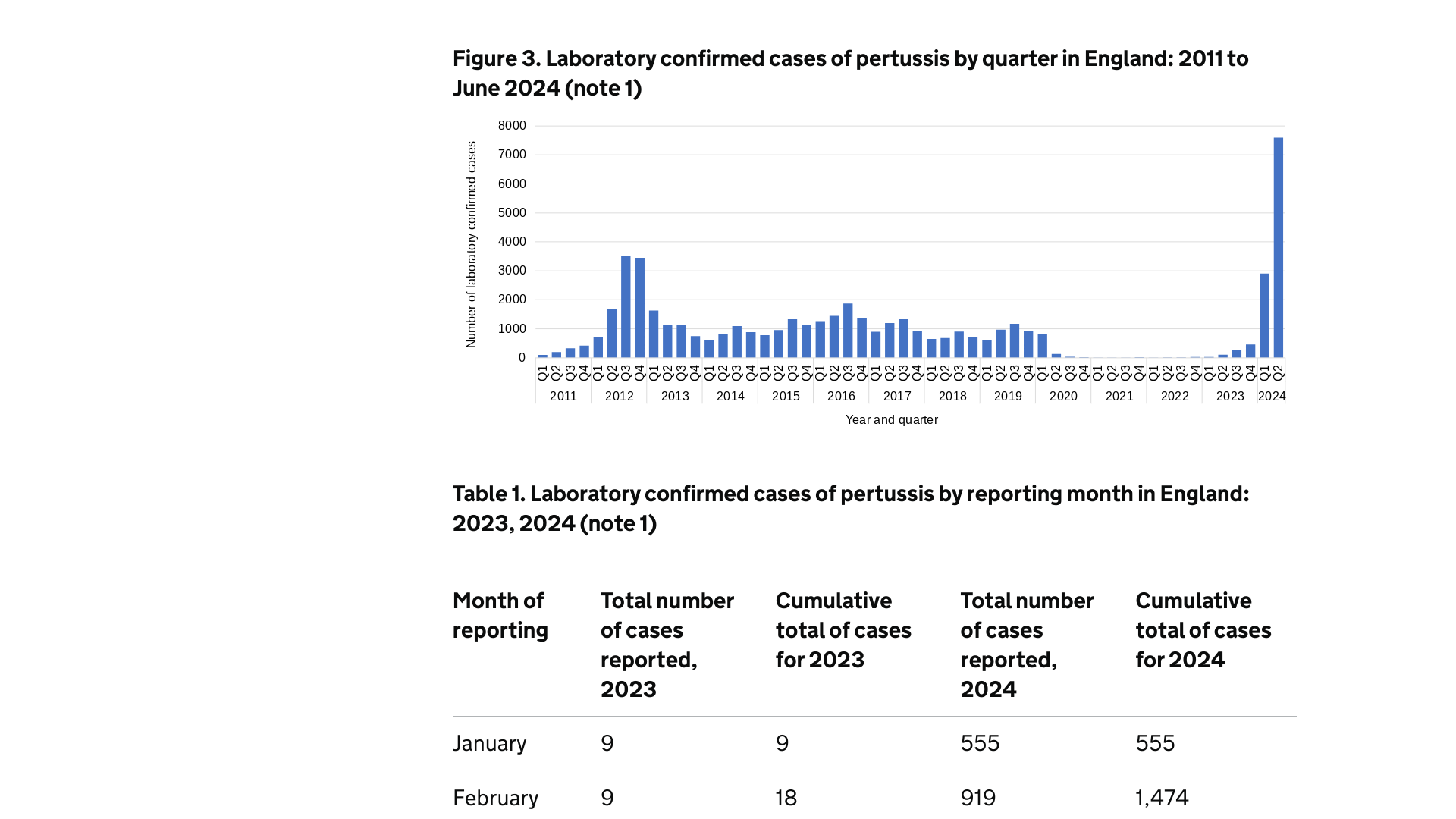
New whooping cough data published today by the U.K. Health Security Agency (UKHSA) shows that laboratory-confirmed cases have exceeded 10,400.
The latest data for England shows cases of whooping cough peaked in May 2024 but continue at high levels, with 2,427 cases reported in June.
On August 8, 2024, the UKHSA confirmed one additional infant death in June, bringing the total to 10 since the current outbreak, which began in November 2023.
Evidence from England shows that vaccination at the right time in pregnancy is highly effective, offering 92% protection against infant death.
The latest uptake data for the vaccination offered to pregnant women to protect newborn infants against whooping cough continues to decline - with coverage in March 2024 at 58.9% compared to the peak coverage (72.6%) in March 2017.
Dr. Mary Ramsay, Director of Immunisation at the UKHSA, said in a press release, "Vaccination is the best defense against whooping cough, and pregnant women and young infants must receive their vaccines at the right time. Pregnant women are offered a whooping cough vaccine in every pregnancy, ideally between 20 and 32 weeks."
"This (vaccination) passes protection to their baby in the womb so that they are protected from birth in the first months of their life when they are most vulnerable and before they can receive their vaccines."
Whooping cough, also known as pertussis, is a bacterial infection that affects the lungs. The first signs of infection are similar to a cold, such as a runny nose and sore throat, but after about a week, the infection can develop into coughing bouts that last for a few minutes and are typically worse at night, says the UKHSA.
In the United States, whooping cough vaccines are generally available at health clinics and pharmacies.
As of August 2024, the U.S. CDC has not issued a Travel Health Advisory regarding the U.K.'s whooping cough outbreak.