Search API
The U.S. Department of State published an updated Level 2: Exercise Increased Caution advisory for visitors to the Kingdom of Denmark, Greenland, and the Faroe Islands.
About 63 million international and domestic tourists visited Denmark in 2023, including over 600,000 from the United States.
As of September 17, 2024, the State Department advises travelers to be aware of their surroundings when traveling to tourist locations and crowded public venues. Additionally, travelers should enroll in the Smart Traveler Enrollment Program to receive alerts, which makes locating you in an emergency easier.
Furthermore, Denmark has excellent medical facilities, such as modern and fully equipped hospitals. However, medical facilities in Greenland and the Faroe Islands are limited, and evacuation is required for serious illness or injury. For emergency services in the Kingdom of Denmark, dial 112, and vaccine information is posted at this link.
The U.S. CDC says those travelers who may be at increased risk of an infectious disease due to their work, lifestyle, or underlying health problems should be up to date with recommended vaccines, which may need to be administered one month before visiting Denmark.
Health clinics and pharmacies in the U.S. generally offer travel vaccines.

The Minnesota Department of Health recently affirmed the greater Twin Cities area is experiencing an ongoing outbreak of measles cases, with the virus spreading mainly among unvaccinated children.
The Minneapolis—St. Paul's measles outbreak began in May 2024, and as of September 19, 2024, 51 cases had been confirmed.
Earlier this year, Chicago, Illinois, reported a more significant measles outbreak that impacted 64 people.
Overall, the U.S. CDC has reported 262 measles cases in 32 jurisdictions in 2024.
From a global health-risk perspective, the CDC has issued travel advisories for over 50 countries this year.
Measles is a vaccine-preventable disease. Vaccination is generally recommended for most people, and various vaccines are available at clinics and pharmacies in the U.S.

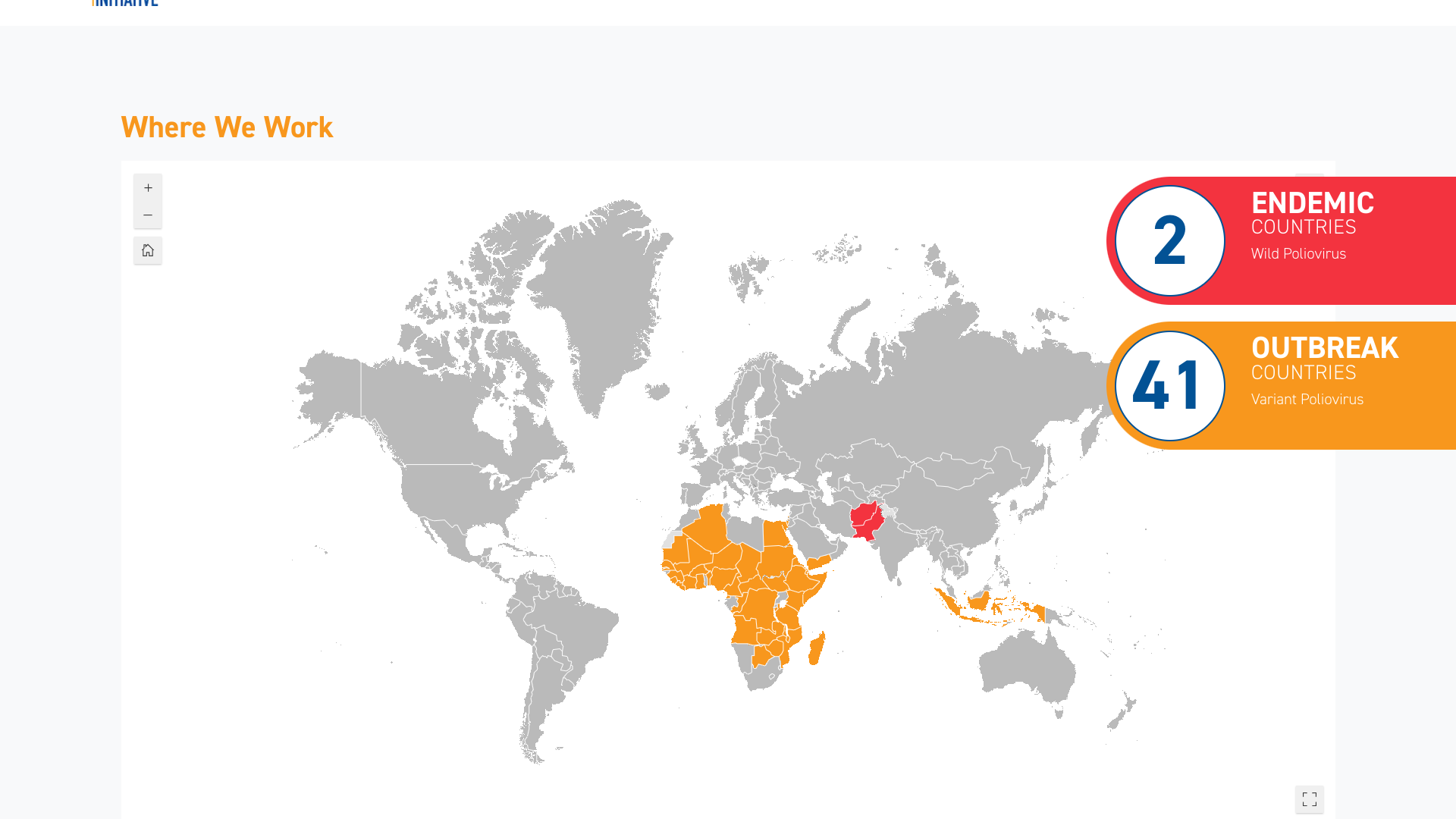
According to the weekly update of the Global Polio Eradication Initiative (GPEI), three countries recently reported new polio cases.
In 2024, Afghanistan reported 19 cases of wild poliovirus type 1 in Kandahar province.
Cameroon reported its first two cases of circulating vaccine-derived poliovirus type 2 (cVDPV2) from Est province this year.
In Nigeria, 53 cases of cVDPV2 were reported from Yobe province, with four new cases added recently.
Overall, two polio-endemic countries are reporting wild polio, Afghanistan and Pakistan, and 41 other countries reporting variant poliovirus.
As of September 21, 2024, the GPEI deploys two types of polio vaccines to stop virus transmission: inactivated polio vaccine (IPV) and oral polio vaccine (OPV). Developing these vaccines to prevent paralytic polio was one of the major medical breakthroughs of the 20th century.
In the United States, the IPV has been offered since 2000.
When planning a visit to a polio-risk country, the U.S. CDC suggests speaking with a travel vaccine expert at least one month before departure about prevention options.
The U.S. Food and Drug Administration (FDA) today announced it approved the nasal influenza vaccine FluMist® for self- or caregiver-administration by adults. This innovative flu shot is sprayed into the nose and has been used safely and effectively for many years.
It is the first influenza vaccine that does not need to be administered by a healthcare provider.
FluMist has been FDA-approved for preventing influenza disease caused by influenza virus subtypes A and B in individuals 2 through 49 years of age for two decades. It was initially approved by the FDA in 2003. In 2007, the FDA approved using FluMist to include children 2 through 5.
Iskra Reic, Executive Vice President of Vaccines and Immune Therapies, AstraZeneca, said in a press release, “The approval of FluMist for self-administration is an important step forward in making vaccines more accessible to fight the high annual burden of influenza."
The vaccine may be administered by a health care provider in a health care setting (including a pharmacy) or by the vaccine recipient or a caregiver who is 18 years of age or older. Vaccine recipients and caregivers who administer FluMist will receive the vaccine, the Prescribing Information, Information for Patients and their Caregivers, and Instructions for Use.
“Today’s approval of the first influenza vaccine for self- or caregiver administration provides a new option for receiving a safe and effective seasonal influenza vaccine potentially with greater convenience, flexibility, and accessibility for individuals and families,” said Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research, in a press release on September 20, 2024.
FluMist remains available at various clinics and pharmacies for the 2024-2025 flu season.
AstraZeneca markets FluMist® under the Fluenz® Tetra brand internationally.

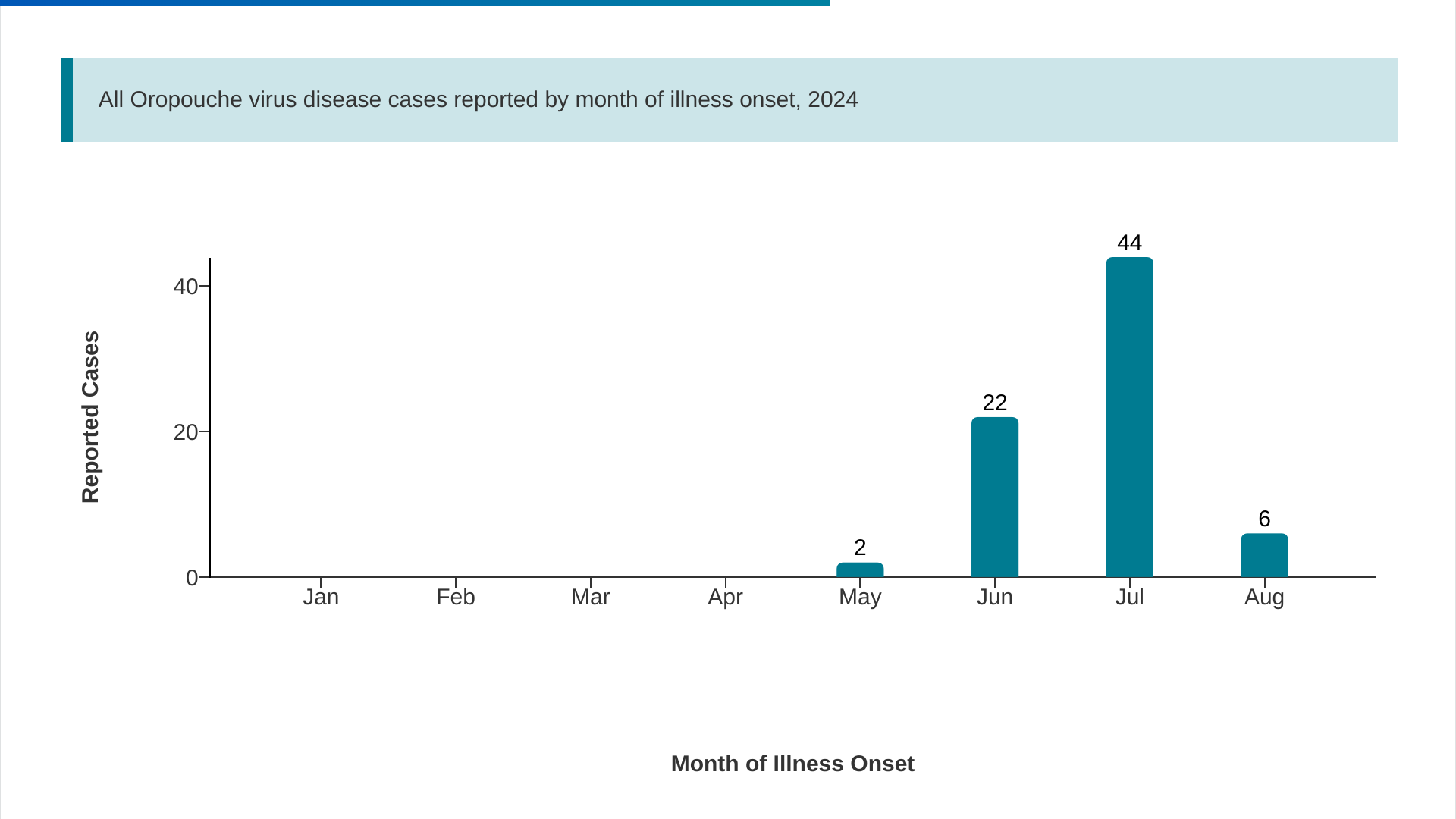
The U.S. Centers for Disease Control and Prevention (CDC) recently reported 22 additional imported cases of the Oropouche virus.
As of September 17, 2024, the total number of cases reported by five U.S. states to 74.
The state of Florida confirmed this week that eleven counties have reported 70 Oropouche cases involving travel to Cuba, which has reported over 500 cases.
The Miami-Dade area (28) has led Florida in reporting cases. The good news is the weekly trends have been decreasing.
In the Region of the Americas, 9,852 cases were confirmed in 2024.
Brazil remains the most affected country, with 7,931 cases and two deaths. Other currently affected countries include Bolivia, Peru, and recently, the Dominican Republic.
The virus is primarily transmitted through the bite of infected midges, small insects that usually bite during the day and inhabit humid areas with organic matter and in forested areas.
Regarding mother-to-child transmission, a total of one fetal death and one case of congenital anomaly have been confirmed in Brazil.
The CDC has confirmed there are not approved vaccines targeting Oropouche virus infections.
The U.S. Centers for Disease Control and Prevention (CDC) recently reported that Respiratory Virus (RSV) activity remained low but is expected to increase.
In the U.S., the annual RSV season usually begins in Florida and then migrates to the southeast, later to the north and west regions.
As of September 17, 2024, week #37, the Florida Department of Health reported increasing RSV positivity rates, decreasing hospital admissions, and no RSV outbreaks.
A recent study found that over the past few years, about 53% of children were infected with RSV during infancy, and 2.8% were hospitalized.
Unlike previous RSV seasons, the U.S. is well prepared to reduce the impact of this respiratory disease.
As of September 20, 2024, three RSV vaccines have been approved, and the CDC recommends a passive immunization (Beyfortus™ (Nirsevimab-alip) for most infants. Based on each state, these U.S. FDA-approved products are offered at health clinics and pharmacies.

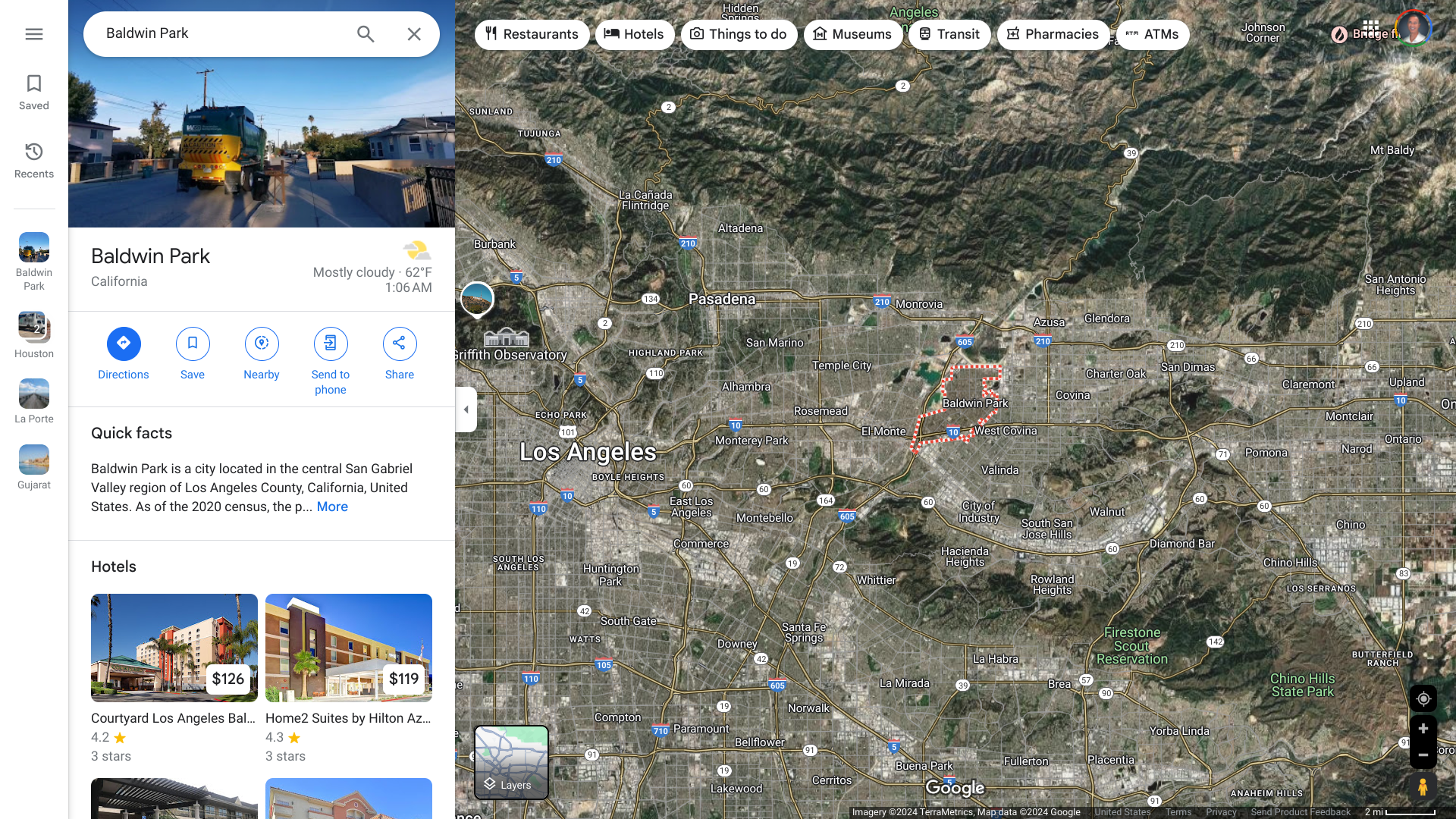
The global dengue fever outbreak recently reached one of the most populated cities in the United States.
The Los Angeles County Department of Public Health announced it is investigating its third locally acquired dengue case in the City of Baldwin Park.
This is an unprecedented number of locally transmitted cases for a region of over 12 million people where mosquitoes have not previously transmitted dengue.
"The City of Baldwin Park is aware of the recent cases of locally acquired dengue in our community. While the risk of transmission remains low, we must take this situation seriously and act proactively," said Mayor Emmanuel J. Estrada, who serves as a trustee representing Baldwin Park on the San Gabriel Valley Mosquito and Vector Control District board, in a press release on September 18, 2024.
In 2024, the U.S. CDC confirmed that 50 jurisdictions, led by California, Florida, New Jersey, New York, and Puerto Rico, had reported 5,027 dengue cases as of September 20, 2024.
In the Region of the Americas, 43 countries and territories have reported over 11,712,499 dengue cases and 6,500 related deaths this year.
While dengue is a vaccine-preventable disease, no vaccine is currently available in the United States. However, Takeda's QDENGA® is an approved two-dose vaccine in about 40 countries.
GSK plc recently announced topline Phase 3 clinical trial data for a combination regimen of two of its vaccines: the RSV vaccine Arexvy and Shingrix, a market-leading shingles shot.
While GSK did not provide specific clinical trial (NCT05966090) data in its September 18, 2024 announcement, the company did confirm that co-administering Arexvy with Shingrix resulted in a “non-inferior immune response” compared with inoculation with the vaccines at separate visits.
The vaccine combo was also well-tolerated with an “acceptable” safety profile, according to GSK.
This is essential news as both RSV and shingles pose significant health risks to older adults, and these risks only increase with age as the immune system declines.
“With our co-administration studies, GSK is using its science and technology to help remove barriers to adult immunization, by potentially reducing the number of visits to the healthcare offices and pharmacies and ultimately help to get ahead of RSV and shingles,” Led Friedland, GSK’s vice president of scientific affairs and public health, said in the statement.
Results from this trial will be submitted for peer-reviewed scientific publication and used to support regulatory submissions to the U.S. FDA, the European Medicines Agency, and other regulators.