Search API
The European Medicine Agency safety committee (PRAC) reviewed new data on the known risk of myocarditis and pericarditis following vaccination with the Comirnaty and Spikevax vaccines.
These heart conditions can develop within just a few days after mRNA vaccination and have primarily occurred within 14 days. And they have more often been observed after the second vaccination in young men.
This PRAC review included two extensive European epidemiological studies.
One study was conducted using data from the French national health system, and the other was based on Nordic registry data.
Based on the reviewed data, the PRAC has determined that the risk for both conditions is overall “very rare.”
This finding means that up to one in 10,000 vaccinated people may be affected.
The EMA reconfirmed on December 3, 2021, that the benefits of all authorized COVID-19 vaccines continue to outweigh their risks, given the chance of COVID-19 illness and related complications, and as scientific evidence shows, that they reduce deaths and hospitalizations due to COVID-19.
The EMA is a decentralized agency of the European Union (EU) based in The Netherlands governed by an independent Management Board responsible for the scientific evaluation, supervision, and safety monitoring of medicines in the EU.
Tampa-based Moffitt Cancer Center says 'therapeutic cancer vaccines activate tumor-specific immune cell responses to help the immune system identify and attack cancer cells.'
And several vaccines focusing on breast cancers that are positive for human epidermal growth factor receptor 2 (HER2) are being studied in clinical trials.
Now, Moffitt Cancer Center researchers are developing a dendritic cell vaccine targeting HER3, a protein involved in the growth and spread of many different cancer types.
During November 2021, their pre-clinical work was published in the journal Cancer Immunology Research, which is excerpted below:
When overexpressed, HER3 can increase the likelihood that cancer will spread and cause treatment to fail.
Several therapies that target HER3 are in clinical development; however, none that take advantage of the tumor-fighting capabilities of the immune system to target HER3 are being tested.
Given the role of HER3 in the development and progression of cancer, Moffitt researchers wanted to assess the possibility of developing a HER3-targeted dendritic cell vaccine to act as either a preventive or therapeutic strategy against different tumor types.
The researcher team first confirmed that HER3 was overexpressed in several types of cancer, including bladder, breast, lung adenocarcinoma, prostate, and stomach, and was associated with poor survival in melanoma and pancreas cancer.
They then identified nine short peptide sequences of the HER3 protein that could be used to generate an immune response from CD4+ T cells in both healthy donors and breast cancer patients.
Notably, the researchers reported that the sequences could be used among a broad patient population based on data from receptor binding studies.
To assess whether the vaccine could offer protection against cancer development or decrease the growth of existing tumors, the researchers vaccinated mice with HER3-peptide stimulated dendritic cells, then injected them with breast cancer or melanoma cells.
Mice vaccinated with HER3-peptide stimulated dendritic cells had significantly delayed tumor growth and prolonged survival compared to mice that received control cells. Similarly, HER3-peptide stimulated dendritic cells also considerably slowed tumor growth and prolonged survival when injected into existing breast and melanoma tumors in mice, including a model of drug-resistant breast cancer.
The researchers confirmed that the HER3-peptide stimulated dendritic cells were producing immune responses mediated by CD4+ T cells and produced antitumorigenic cytokines.
"Developing HER3-specific cellular immunotherapy can be a novel and efficient treatment strategy for multiple cancer types overexpressing HER3 to improve patient prognosis and survival," explained Brian Czerniecki, M.D., Ph.D., chair of the Department of Breast Oncology at Moffitt, in a press statement issued on December 1, 2021.
More research is needed, but Czerniecki and his team hope to advance this discovery to human clinical trials in the future. Their study was supported by the National Cancer Institute, Department of Defense, and Pennies in Action.
Moffitt Cancer Center is dedicated to one lifesaving mission: to contribute to the prevention and cure of cancer. The Tampa-based facility is one of only 52 National Cancer Institute-designated Comprehensive Cancer Centers in the U.S.

The U.K.'s Department for Transport recently published what people must do before traveling to England and upon arrival.
These new requirements depend on whether you qualify as fully vaccinated under England's rules.
There are different rules if you have been in a Red list country or territory ten days before arriving in England. The Red list rules apply whether you are fully vaccinated or not.
- If you are fully vaccinated before visiting England, you must:
- book and pay for a COVID-19 PCR test – to be taken after you arrive in England
- complete a passenger locator form – to be completed in the 48 hours before you arrive in England
- You cannot use an NHS test for your PCR test. It would be best if you used a private test provider.
- You will need to enter your COVID-19 test booking reference number on your passenger locator form.
If you're in England for less than two days, you still need to book and pay for a day two COVID-19 test. And you must quarantine until receiving a negative PCR test or until you leave England, whichever is sooner.
And when a fully vaccinated traveler arrives in England:
- You must take a COVID-19 PCR test.
- You can take the test any time after you arrive and before the end of day two at the latest.
- It would be best if you were quarantined in your home or the place you are staying while you await your test result.
- If your test result is negative, you can end your quarantine.
- If your test result is positive, you must self-isolate for ten full days.
- If your test result is unclear, you must self-isolate for ten full days.
For additional clarifications, the U.K. publishes FAQs on this webpage.
Separately, the U.S. CDC and Department of State recently published high-level travel advisories that discourage visiting the U.K. this holiday season.

The Netherlands-based European Medicines Agency (EMA) vaccine safety committee today announced it has assessed the known risk of myocarditis and pericarditis following vaccination with mRNA COVID-19 vaccines Comirnaty and Spikevax and determined that the risk for both of these conditions is overall "very rare."
This means that up to one in 10,000 vaccinated people may be affected.
Additionally, the data show that the increased risk of myocarditis after vaccination is highest in younger males.
Myocarditis and pericarditis can develop within just a few days after vaccination and have often been observed after the second vaccination.
The French and Nordic studies estimate the number of extra cases of myocarditis in younger males following the second dose, compared to unexposed persons of the same age and gender.
For Comirnaty (Pfizer - BioNTech), the French study shows that, in seven days after the second dose, there were about 0.26 extra cases of myocarditis in 12- to 29-year-old males per 10,000 compared to unexposed persons.
In the Nordic study, in 28 days after the second dose, there were 0.57 extra cases of myocarditis in 16- to 24-year-old males per 10,000 compared to unexposed persons.
In the case of Moderna Inc.'s Spikevax, the French study showed that in seven days after the second dose, there were about 1.3 extra cases of myocarditis in 12- to 29-year-old males per 10,000 compared to unexposed persons.
The Nordic study shows that in 28 days after the second dose of Spikevax, there were around 1.9 extra cases of myocarditis in 16- to 24-year-old males per 10,000 compared to unexposed persons.
Myocarditis and pericarditis are inflammatory conditions of the heart that present a range of symptoms, often including breathlessness, a forceful heartbeat that may be irregular (palpitations), and chest pain.
Available data suggest that the course of myocarditis and pericarditis following vaccination is not different from myocarditis or pericarditis in general.
The EMA confirmed that the 'benefits of all authorized COVID-19 vaccines continue to outweigh their risks.'
The mission of the EMA is to foster scientific excellence in the evaluation and supervision of medicines for the benefit of public and animal health in the European Union.

Norway-based Ultimovacs ASA today announces that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation (ODD) for the company’s universal cancer vaccine UV1 to treat stage IIB – IV melanoma.
UV1, as an add-on therapy to checkpoint inhibitors ipilimumab and nivolumab.
And UV1 is currently being studied as a first-line treatment for metastatic melanoma in a Phase II trial named INITIUM.
The FDA Orphan drug designation provides certain benefits, including seven-year market exclusivity upon regulatory approval if received, exemption from FDA application fees, and tax credits for qualified clinical trials.
“We are very pleased to have been granted this orphan drug designation for UV1 in treating metastatic melanoma. The designation underlines the promise of UV1 that has been shown in our clinical studies in metastatic melanoma to date,” said Carlos de Sousa, CEO of Ultimovacs, in a press statement issued on December 2, 2021.
“We remain committed to further investigating UV1 in our ongoing Phase II clinical studies and to continuing our constructive dialog with regulators to bring UV1 to patients as soon as possible.”
In October 2021, the FDA granted Fast Track designation to UV1 as an add-on therapy to ipilimumab or pembrolizumab to treat unresectable or metastatic melanoma.
Melanoma is the fifth most common cancer in both men and women in the U.S., with more than 100,000 new cases of melanoma diagnosed every year.
UV1 is being investigated in combination with checkpoint inhibitors in Phase II trials covering advanced malignant melanoma, ovarian cancer, head and neck squamous cell carcinoma, malignant pleural mesothelioma, and non-small cell lung cancer.
In total, the five Phase II trials will enroll more than 650 patients at nearly 100 clinical centers across 15 countries.
Ultimovacs, based in Oslo, Norway, is developing immune-stimulatory vaccines to treat a broad range of cancers.

The Board of Gavi, the Vaccine Alliance, today approved an investment to support the malaria vaccine introduction, procurement, and delivery for countries in sub-Saharan Africa in 2022-2025.
An initial investment of US$ 155.7 million for 2022-2025 will initiate the implementation of the RTS,S malaria vaccine.
José Manuel Barroso, Chair of the Gavi Board, said in a press release issued on December 2, 2021, "Thanks to the collaborative efforts of the global health community, we are better armed to tackle this deadly disease, and once the vaccine is rolled out at scale, we will be able to help protect millions of lives."
The approval of the funding follows WHO's recommendation for wider routine use of the RTS,S malaria vaccine on October 6, 2021.
GSK's Mosquirix RTS,S/AS01e, is a recombinant malaria vaccine that aims to trigger the immune system to defend against the first stages when the Plasmodium falciparum malaria parasite enters the human host's bloodstream through a mosquito bite and infects liver cells.
Malaria is a disease caused by a parasite that spreads to humans through the bite of an infected mosquito.
Early symptoms of malaria resemble those of the flu, including fever, chills, sweats, headache, vomiting, and body aches. However, malaria can rapidly progress to severe illness and death without prompt diagnosis and treatment.
Following today's decision, technical guidance on the use of the vaccine alongside opening the funding window to allow applications from countries that receive support from Gavi.
The U.S. CDC recently issued a Level 1 Travel Advisory regarding the malaria epidemic in Burundi, a central Africa country.
Since January 2019, the Ministry of Health has reported nearly 6 million cases (out of a total population of approximately 12 million), with more than 1,800 deaths.
About 2,000 cases of malaria are diagnosed in the United States annually, mostly in returned travelers, says the U.S. CDC.

Another COVID-19 antibody treatment, Xevudy (sotrovimab), has today been approved by the U.K.'s Medicines and Healthcare products Regulatory Agency (MHRA) after it was found to be safe and effective at reducing the risk of hospitalization and death in people with mild to moderate COVID-19 infection who are at an increased risk of developing severe disease.
It is approved for individuals aged 12 and above who weigh more than 40kg.
Developed by GSK and Vir Biotechnology, sotrovimab is a single monoclonal antibody that works by binding to the spike protein outside the COVID-19 virus. This, in turn, prevents the virus from attaching to and entering human cells so that it cannot replicate in the body.
In a clinical trial, a single dose of the monoclonal antibody was found to reduce the risk of hospitalization and death by 79% in high-risk adults with symptomatic COVID-19 infection.
Based on the clinical trial data, sotrovimab is most effective when taken during the early stages of infection. So the MHRA recommends its use as soon as possible and within five days of symptom onset.
Xevudy (sotrovimab) is the second monoclonal antibody therapeutic approved by the MHRA following Ronapreve (REGEN-COV).
REGEN-COV is delivered via injection or IV, providing 'passive immunity and immediately protecting people from COVID-19. However, it must be re-administered to remain effective over time.
Sotrovimab is administered by intravenous infusion over 30 minutes.
Moreover, it is too early to know whether the Omicron virus variant impacts sotrovimab's effectiveness, but the MHRA is working with the company to clarify this new threat.
Additional antibody treatment news is published on this webpage.

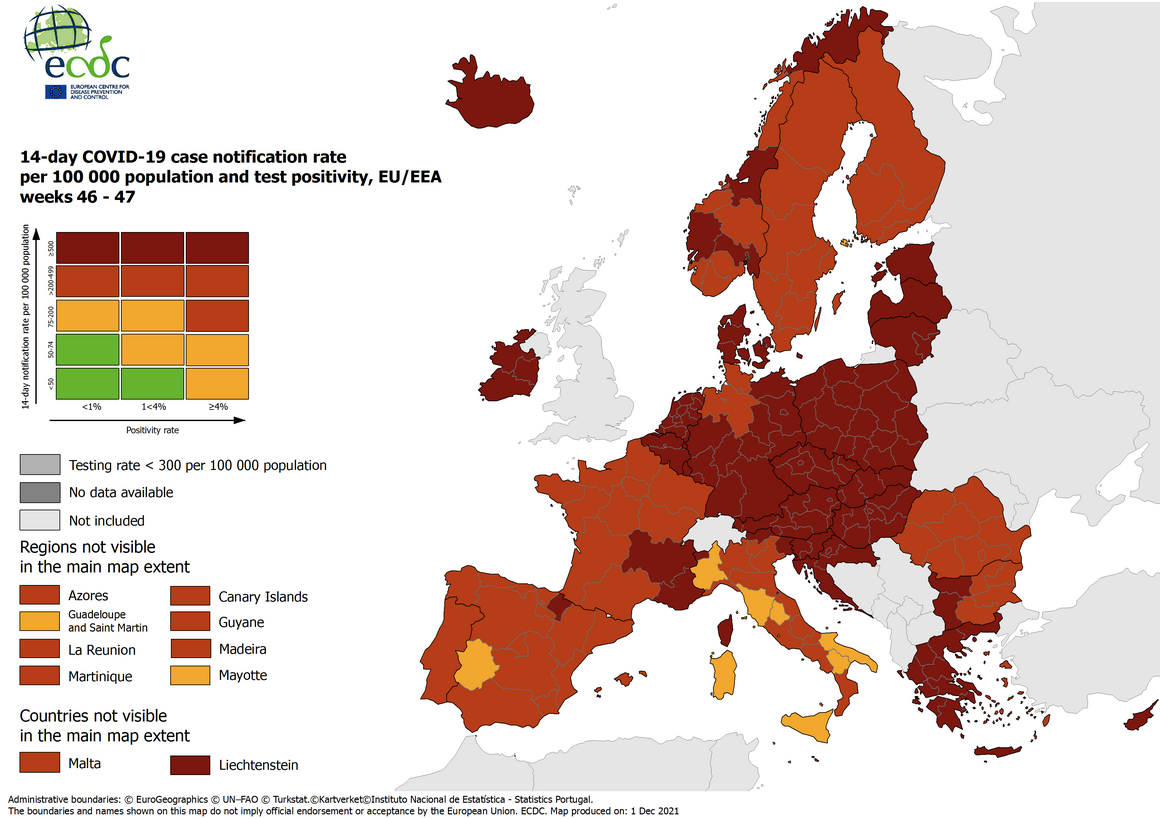
First detected on November 11, 2021, in Botswana, Africa, the number of countries reporting cases of the SARS-CoV-2 virus variant known as Omicron in the EU/EEA continues to increase, confirmed the ECDC today.
The number of countries reporting Omicron cases continues to increase globally, with a total of 352 confirmed cases reported by 27 countries as of December 1, 2021, including 70 confirmed cases reported by 13 European Union and European Economic Area (EU/EEA) countries.
There are several uncertainties around Omicron in terms of transmissibility, severity, and immune escape potential.
Based on mathematical modeling conducted by ECDC, there are indications that Omicron could cause over half of all SARS-CoV-2 infections in the EU/EEA within the next few months.
Temporary travel-related measures should be carefully considered in light of the latest epidemiological situation.
Such measures might include the testing and quarantining of travelers who have recently returned from affected countries. In addition, public information around the emerging situation and the public health measures in place are essential to raise awareness and support their effective implementation.
U.S. health officials confirmed today that the first case of the Omicron SARS-CoV-2 virus variant had been identified in a person currently in California.
During today's press conference, the Centers for Disease Control and Prevention revealed the individual returned from South Africa on November 22, 2021.
"The individual, who was fully vaccinated and had mild symptoms that are improving, and is self-quarantining. All close contacts have tested negative."
The new variant Omicron has been found in countries from Europe to the Middle East.
The ECDC reported as of December 1, 2021, a total of 59 cases have been reported by 11 European Union and European Economic Area countries: Austria (3), Belgium (2), Czechia (1), Denmark (4), France (1, in Réunion), Germany (9), Italy (4), the Netherlands (16), Portugal (14), Spain (2), and Sweden (3).
Cases have been reported in 12 countries and territories outside the EU/EEA - Australia, Botswana, Brazil, Canada, Hong Kong Special Administrative Region, Israel, Japan, Nigeria, Saudi Arabia, South Africa, Switzerland, and the United Kingdom.

Massachusetts-based VBI Vaccines Inc. today announced that the U.S. Food and Drug Administration (FDA) had approved the PreHevbrio™ vaccine for the prevention of infection caused by all known subtypes of hepatitis B virus (HBV) in adults age 18 years and older.
PreHevbrio contains the S, pre-S2, and pre-S1 HBV surface antigens.
It is the only Approved 3-antigen HBV vaccine for adults in the U.S. and is commercially available in Israel under the brand name Sci-B-Vac®.
VBI expects to make PreHevbrio available in the U.S. in the first quarter of 2022 and has partnered with Syneos Health to ensure commercial readiness.
Chari Cohen, DrPH, MPH, Senior Vice President of the Hepatitis B Foundation, stated in a press release, “Having more vaccine options will help us effectively expand vaccine uptake, ensure more people are protected from hepatitis B infection, and reach the 2030 goal of eliminating hepatitis B in the U.S.”
The approval of PreHevbrio was based on the results from two Phase 3 clinical studies, PROTECT and CONSTANT, data from which were published, respectively, in The Lancet Infectious Diseases in May 2021 and The Journal of the American Medical Association Network Open in October 2021.
Outside of the U.S., VBI continues to support the European Medicines Agency’s ongoing review of the marketing authorization application for the E.U.
And VBI expects to complete regulatory submissions to the U.K.’s Medicines and Healthcare products Regulatory Agency and Health Canada in 2022.
VBI is a biopharmaceutical company located in Cambridge, MA, driven by immunology to pursue powerful prevention and treatment of disease.
