Japanese Encephalitis Outbreaks
Japanese Encephalitis Outbreaks September 2025
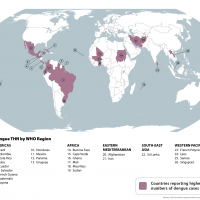
According to the World Health Organization (WHO), the Japanese encephalitis virus (JEV) is a flavivirus transmitted by mosquitoes, often contracted from infected pigs and sheep. Humans are not a dead-end host in the transmission cycle, and there is no human-to-human transmission of JEV. As of August 2025, JEV is the leading cause of viral encephalitis in 24 countries in the WHO South-East Asia and Western Pacific/Oceania Regions, exposing more than 3 billion people to infection risks. In 2025, the WHO published a technical brief titled "Encephalitis: Global Threats, Trends, and Public Health Implications." Japanese encephalitis (JE) cases are collected annually through the WHO/UNICEF Joint Reporting Form on Immunization. JE infections cause approximately 13,600–20,400 deaths in people annually. JE survivors are estimated to live normally, but 49% of patients report neurological sequelae.
Japanese Encephalitis in the United States
JEV was confirmed in the United States in the 1980s when the exotic mosquito species and secondary JEV vector, Aedes albopictus, was introduced into the country. As of July 2025, the U.S. Centers for Disease Control and Prevention (CDC) identified countries reporting JEV cases. The CDC states that the risk for JE varies based on destination, accommodations, activities, trip duration, and travel season. A risk assessment conducted in 2019 examined the potential mechanisms of introducing JEV into the U.S. It concluded that an infected adult mosquito posed a high risk of introduction via passenger aircraft. Geographically, the risk of JE introduction into the U.S. may be highest in California due to the frequency of international arrivals (as of August 2024) from Asia (particularly in LA County) and the abundance of Culex vectors and avian hosts. In July 2005, one JE case was reported to LA County regarding a California resident who traveled to the Philippines. One Japanese encephalitis vaccine (IXIARO) is U.S. FDA-approved and recommended for travelers in 2025.
Japanese Encephalitis in Australia
Australia's National Notifiable Disease Surveillance System dashboard has reported JEV cases from 2002 to 2025, with a peak of 41 cases in 2022. JE cases have been confirmed across Australia, including Queensland, New South Wales, South Australia, Victoria, the Australian Capital Territory, Tasmania, Western Australia, the Northern Territory, and parts of the Torres Strait region. Australia's government declared a JEV outbreak of National Significance in March 2022. In June 2023, the Joint National Japanese Encephalitis Virus Outbreak Response Plan (JEV Outbreak Plan) became the first Australian Response Plan for Japanese Encephalitis.
As of August 2025, eight JE cases have been confirmed in Australia. On March 14, 2025, the fourth JE-related fatality was reported since the virus was first detected in NSW in 2022. On February 15, 2025, a man likely acquired his JE infection while camping in the Murrumbidgee region in NSW. In January 2025, NSW Health listed Tamworth, Gunnedah, Moree, Narrabri, Gwydir, Inverell, Liverpool Plains, Tenterfield, and Upper Hunter local government areas as "high JE concern." JE virus was previously detected in mosquitoes in December 2024 in the Griffith area and feral pigs in the Narromine Shire local government area. No confirmed human cases of JEV have been acquired in NSW since October 2022. Between 2021 and 2022, 13 JEV cases were reported in New South Wales
Queensland health authorities reported in March 2025 that JEV was detected for the first time in mosquitoes collected in Brisbane's eastern suburbs in Hemmant. In January 2025, Queensland recorded its first locally acquired human case of JEV since 2022. This person was likely infected in the Darling Downs region near Goondiwindi. The JEV vaccine is available at over 100 vaccination providers across Queensland.
On January 20, 2025, the Victoria Department of Health confirmed that a human case of JE had been identified in a resident of northern Victoria, marking the first case in the state. Residents and visitors to northern Victoria, particularly those in inland riverine regions and near the Murray River, are at a higher risk of infection and should take measures to prevent mosquito bites. In Victoria, the JE vaccine is free of charge for specific groups at higher risk of exposure to the virus.
QIMR Berghofer senior researchers reported in May 2024 that the new JEV virus strain (genotype 4) impact on the brain is consistent with the seven human fatalities during the 2022 outbreak, which involved 44 confirmed human cases across Victoria, New South Wales, South Australia, Northern Territory, and Queensland. he findings of the two studies (May 2024), taken together with the broad geographic spread of human infections and infected piggeries over a relatively short period, indicate that the 2022 JEV outbreak was more extensive than initially thought. The health department recommends JE vaccination for travelers spending one month or more in endemic areas in Asia and Papua New Guinea during the period of virus transmission. E vaccination is recommended for residents of the outer islands in the Torres Strait who live or work on the outer islands for 30 days or more during the wet season. People who are at ongoing risk of acquiring JE may need booster doses.
In December 2022, the U.S. CDC updated a Travel Health Advisory—Level 2, Practice Enhanced Precautions—regarding the JE outbreak in eastern and southeastern Australia.
Japanese Encephalitis in Canada
The Canadian government states that the risk of JEV for travelers is low, especially for those visiting urban areas. However, there is a higher risk of infection if they visit rural areas for extended periods and participate in outdoor activities.
Japanese Encephalitis in Europe
The European CDC published a study in 2023 that concluded that the environmental conditions in the European Union are expected to be suitable for the Japanese encephalitis virus to circulate.
Japanese Encephalitis in India
The first evidence of the JE virus's presence in India dates back to 1952, when the first case was reported. The first human JE case was reported in Vellore, Tamil Nadu. As of August 2025, JE remains a significant public health concern in India's various states, with over 468 cases and 56 related fatalities this year.
In June 2025, Assam, a northeastern state of India, had 32 patients admitted to the Gauhati Medical College and Hospital, with four confirmed deaths. According to data from the Integrated Disease Surveillance Programme, 1,548 JE cases were reported from 24 states and Union Territories in 2024, with about 925 JE cases detected in Assam alone. In 2023, 1,320 JE cases were reported, compared to 1,271 in 2022.
India's National Center for Vector-Borne Diseases Control (NCVBDC) confirmed in 2023 that adult JE vaccinations had started in 42 districts of three states with high JE incidence: Assam (9 districts), Uttar Pradesh (7 districts), and West Bengal (26 districts). In March 2025, the Pune Municipal Corporation initiated a JE vaccination drive targeting 1,98,874 children aged 1 to 10 years across multiple city zones, with an overall goal of vaccinating 10.43 lakh children.
Japanese Encephalitis in Indonesia
The U.S. CDC reports JE cases from many Indonesian islands, including Bali, Java, Kalimantan, Nusa Tenggara, Papua, and Sumatra. The WHO has actively supported Indonesia's Ministry of Health with interventions to control JEV infection, including preparations to introduce JEV vaccination in new endemic provinces, with a focus on West Kalimantan.
Japanese Encephalitis in Japan
The number of Japanese encephalitis cases in Japan decreased after the implementation of a national vaccination program. Sporadic JE cases are reported from all of Japan's islands except Hokkaido. As of 2022, only one case had been reported in Chiba and Ibaraki prefectures over the past 10 years, and both cases occurred in areas renowned for pig farming, far from Narita City. According to a study published in June 2025, three domestically infected JE cases occurred over the three consecutive years from a hospital in Narita, Chiba, where JE had not been reported in recent years.
Japanese Encephalitis in Papua New Guinea
The surveillance and detection of Japanese encephalitis in Papua New Guinea (PNG) have been confirmed. The U.S. CDC recommends considering JE vaccination for travelers spending less than a month in areas with Japanese encephalitis who will be engaging in activities that increase the risk of infection, such as visiting rural areas, hiking, camping, or staying in places without air conditioning, screens, or bed nets.
Japanese Encephalitis in the Philippines
Human, animal, and mosquito studies indicate transmission in 32 provinces of the Philippines.
Japanese Encephalitis in Nepal
In Nepal, Japanese Encephalitis (JE) has been a significant public health concern since 1978, particularly in the Terai region, which borders India. About 12.5 million people in Nepal are at high risk of JE infection. In 2005, JE infections killed nearly 2,000 people in Nepal's Tarai region.
In 2025, Nepal's Health Ministry's data show 33 JE cases and three fatalities. The WHO indicated in August 2025 that Nepal's national JE vaccination coverage surpasses 95%. The WHO also provides technical assistance for field monitoring and reaching children. Who are unvaccinated
As of September 2024, twenty-nine districts in Nepal, including those in the Kathmandu Valley, have reported infections from the deadly vi. Meanwhile, eight districts —Kailali, Kapilvastu, Palpa, Chitwan, Rautahat, Sarlahi, Siraha, and Suns —have reported deaths from the infection. In 2024, 23 people died, and 80 others were infected with the JE virus.
Japanese Encephalitis in South Korea
The U.S. CDC says Japanese encephalitis was a significant public health concern in South Korea until the late 1960s, with several thousand cases reported annually. In 2024, the Korea Disease Control and Prevention Agency (KDCA) reported 21 locally transmitted cases of Japanese encephalitis. The KCDC reported that in 2018, JE surveillance data showed an average of 20 JE cases per year.
Japanese Encephalitis in Thailand
The highest number of disease cases has been reported in Thailand's Chiang Mai Valley.
Japanese Encephalitis in Taiwan
In Taiwan (Republic of China), JE has been categorized as a mandatory notifiable infectious disease since 1955. This study confirmed cases of JE from the surveillance data of the Taiwan Centers for Disease Control (TCDC) between 2008 and 2020. As of July 2025, the TCDC confirmed six cases of Japanese encephalitis. In 2024, 25 JE cases were reported.
Japanese Encephalitis in the United Kingdom
In England, Wales, and Northern Ireland (EWNI), no cases of Japanese encephalitis were reported in 2024. The most recently reported case was in 2023. JE vaccine is available in the UK; however, it is only recommended for travellers at an increased risk of infection.
Murray Valley Encephalitis in Australia
As of March 2025, three cases of Murray Valley encephalitis had been reported in northern Western Australia, specifically in the Pilbara and Kimberley regions.