Search API
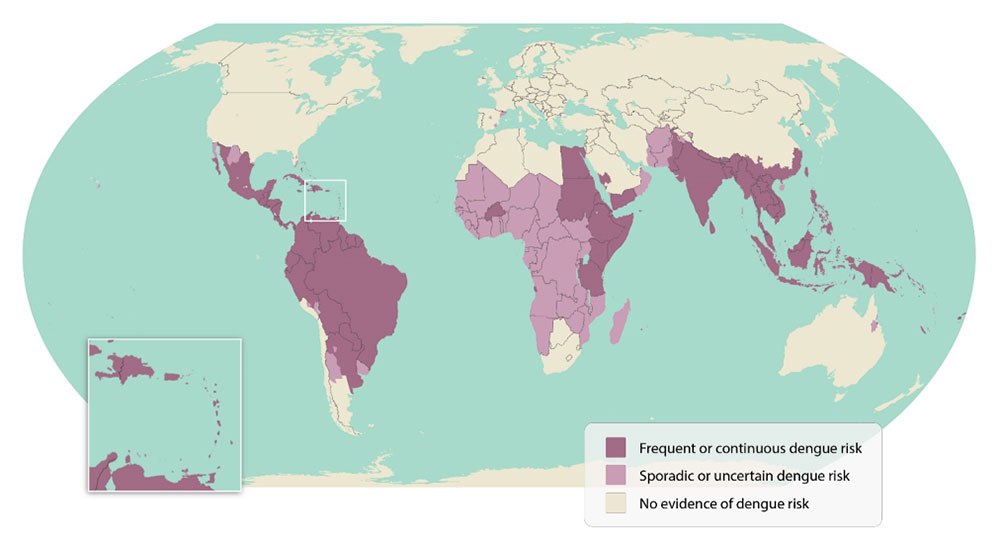
During the summer of 2023, the European CDC reported autochthonous / non-travel-associated dengue cases in Europe, from France and Italy.
Following investigations carried out by Bouches-du-Rhône, two new cases of autochthonous Dengue were identified in Gardanne. There are now 4 cases in France this year.
In the French Antilles, Martinique and Guadeloupe have entered an epidemic phase, as mentioned by Santé Publique France in an August 2023 press release.
Dengue cases have also been reported in Réunion and French Guiana this year.
On 18 and 20 August 2023, unrelated to travel, two confirmed cases of Dengue were reported by the Lombardy and the Lazio Regions in Italy. As of July 2023, 47 confirmed dengue cases were associated with overseas travel.
As of late August 2023, the U.S. CDC continues alerting international travelers of their health risks when visiting dengue outbreak areas. The CDC says that dengue is spread to people through the bite of an infected Aedes mosquito.
CSL Seqirus today announced it was selected by the Biomedical Advanced Research and Development Authority (BARDA) to deliver one bulk lot of H5N8 A/Astrakhan antigen to the U.S. government.
This acquisition of a bulk lot will increase BARDA's stockpile of vaccines to support rapid response in an associated influenza pandemic.
CSL Seqirus has been working with BARDA in a longstanding partnership for over a decade, including numerous R&D and manufacturing activities and awards supporting BARDA's pandemic preparedness objectives.
Confirmed on August 28, 2023, this is the third award CSL Seqirus has received from BARDA in the last two years related to the ongoing outbreak of HPAI in the United States.
As of August 2023, the Pan American Health Organization reported H5N1 viruses (clade 2.3.4.4b) had been detected in 15 countries in Latin America, the Caribbean, the United States, and Canada over the past 18 months.
This award follows the February 2022 award to produce an H5N8 A/Astrakhan virus vaccine seed and the subsequent October 2022 announcement of the selection of CSL Seqirus to deliver an H5N8 A/Astrakhan virus vaccine candidate for assessment in a Phase 2 clinical study.
While the likelihood of sustained human-to-human transmission of bird flu is "low," according to the U.S. Centers for Disease Control and Prevention (CDC) and World Health Organization, there have been reported a small number of human cases of avian influenza A(H5), including one in the U.S. in April 2022, a case in Ecuador in January 20235 and Chile in March 2023.
"While human cases are rare, sporadic, and isolated, consistent detection of bird and mammalian cases demands vigilance," commented Marc Lacey, Executive Director, Pandemic Response Solutions, CSL Seqirus, in a press release.
"Ongoing surveillance and preparedness efforts are critical to minimize the public health risk."
CSL Seqirus used its cell-based influenza vaccine technology, as utilized for FDA-approved AUDENZ™ (Influenza A(H5N1) Monovalent Vaccine, Adjuvanted), to manufacture the H5N8 A/Astrakhan bulk vaccine at the company's Holly Springs, North Carolina, facility, which was built in partnership with BARDA.
CSL Seqirus has established and will maintain the required pandemic readiness to deliver 150 million doses of cell-based pandemic influenza vaccine within six months of an influenza pandemic declaration in the U.S.
This $46.3 million project has been supported in whole or in part with federal funds from the Department of Health and Human Services, Administration for Strategic Preparedness and Response; BARDA, under contract number 75A50122D00004.

According to media reports, the Dengue outbreak in Bangladesh accelerated in August 2023.
The Dhaka Tribune reported on August 26, 2023, that Bangladesh had its worst day ever for Dengue, with nine deaths and 1,960 hospitalized in a day.
This news increases Bangladesh's total number of dengue-related deaths to 537 in 2023.
Dengue is endemic in Bangladesh, resulting in high morbidity and mortality.
The World Health Organization says Dengue is the fastest-spreading mosquito-borne infectious disease and has emerged as a global public health problem.
As of August 28, 2023, two approved and various Dengue vaccine candidates are in development.
In addition to the ongoing Dengue outbreak, the U.S. CDC suggests various travel vaccines before visiting Bangladesh in 2023.

Valneva SE today reported positive initial Phase 3 safety data in adolescents for its single-dose chikungunya virus (CHIKV) vaccine candidate VLA1553.
On August 28, 2023, Valneva announced the initial safety data generated in the ongoing trial VLA1553-321, Valneva's first clinical trial in an endemic area (Brazil) and with individuals previously infected with CHIKV, showed that VLA1553 was generally safe and well tolerated in adolescents aged 12 to 17 years, regardless of previous CHIKV infection.
In this study, 754 individuals were vaccinated in trial VLA1553-321, and the present analysis includes safety data up to Day 29. An independent DSMB has continuously evaluated safety data during the trial and identified no safety concerns.
Overall, the adverse event profile is consistent with the profile observed in Valneva's pivotal Phase 3 trial in adults, reported in March 2022.
Immunogenicity data for this new trial are expected in November 2023.
Juan Carlos Jaramillo, M.D., Chief Medical Officer of Valneva, commented in a press release, "These new safety data in a younger population and individuals previously infected with the chikungunya virus confirm the safety profile we previously observed in adults and the elderly."
"Chikungunya represents a major threat for people traveling to or living in areas where chikungunya virus is endemic, it is, therefore, our objective to make this vaccine available to all age groups, especially as no vaccine or specific treatments are currently available for this debilitating disease."
Funded by the Coalition for Epidemic Preparedness Innovations and conducted in collaboration with Brazil's Instituto Butantan, the VLA1553-321 adolescent trial is intended to support label extension in this age group following a potential initial regulatory approval in adults from the U.S. Food and Drug Administration. The trial is also expected to support the vaccine's licensure in Brazil, which would be the first potential approval for use in endemic populations.
The present safety analysis will also enable regulatory submission to the European Medicines Agency in 2023.
If licensed, this would be the first CHIKV vaccine candidate approved.

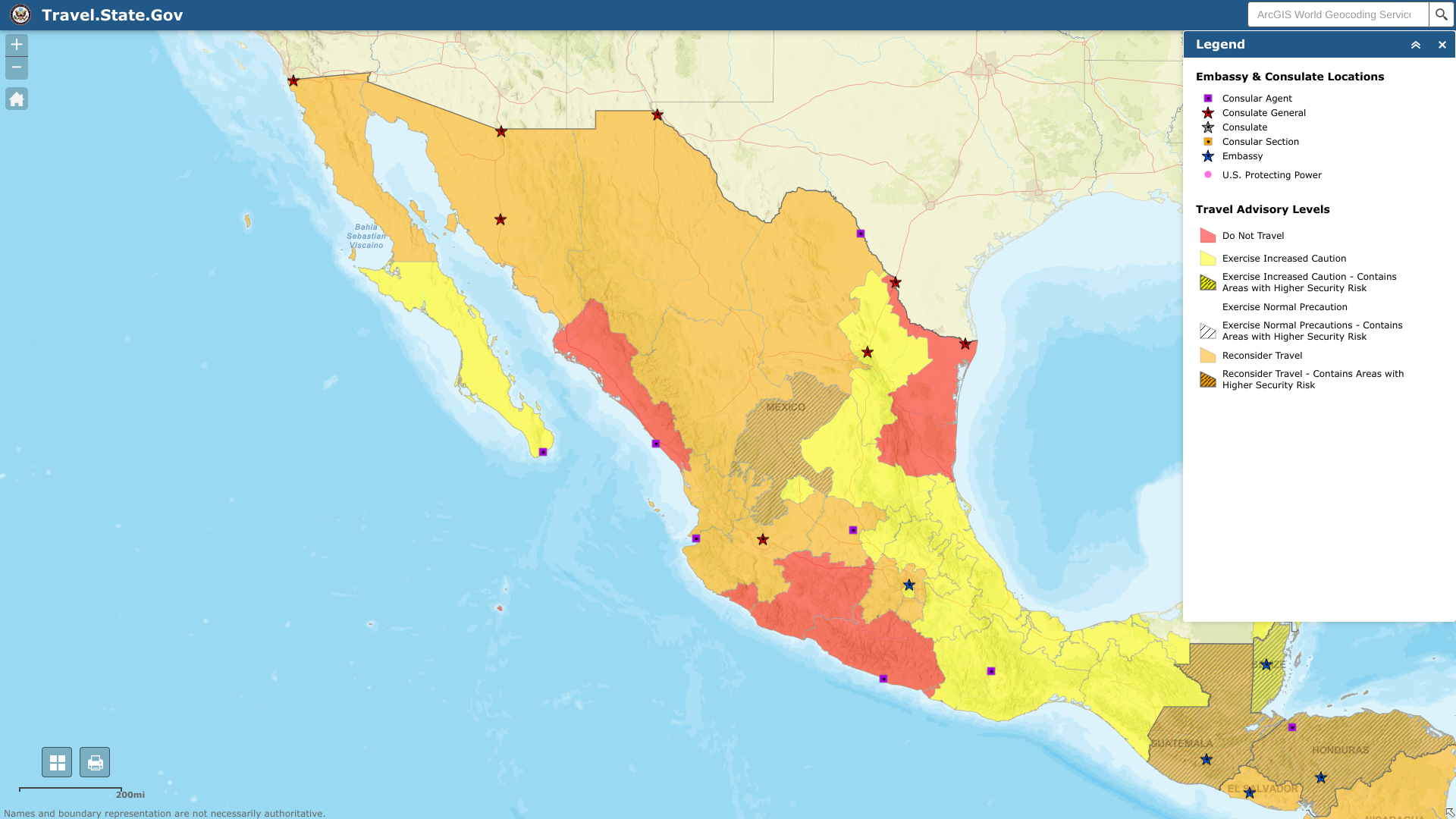
The U.S. Department of State reissued its unclassified travel advisory regarding extensive civil unrest throughout the United States of Mexico.
On August 22, 2023, the State Department reported it has limited ability to provide emergency services to U.S. citizens in many areas of Mexico, as travel by U.S. government employees to certain areas is prohibited or restricted.
In many Mexican states, local emergency services are limited outside the state capital or major cities, including Cancun.
Furthermore, U.S. government employees may not travel between cities after dark, may not hail taxis on the street, and must rely on dispatched vehicles, including app-based services like Uber and regulated taxi stands.
U.S. government employees should avoid traveling alone, especially in remote areas. U.S. government employees may not drive from the U.S.-Mexico border to or from the interior parts of Mexico, except daytime travel within Baja California and between Nogales and Hermosillo on Mexican Federal Highway 15D, and between Nuevo Laredo and Monterrey on Highway 85D.
From a health perspective, several disease outbreaks have been reported in 2023, and the U.S. CDC suggests various pre-trip vaccinations.
Since dengue outbreaks cause about 400 million infections yearly, the Pan American Health Organization (PAHO) and other agencies continue issuing health alerts for this deadly disease.
In the Americas, the total number of dengue cases reported was 2,997,097 through July 2023. Additionally, 1,302 deaths were reported in the Region.
To limit these deaths, two dengue vaccines have been approved and deployed in 2023.
According to a new study published in the journal Vaccines on August 22, 2023, the effectiveness of these vaccines varies.
Dengvaxia® has shown an efficacy of 60.8 % (95 % CI, 52.0–68.0) against symptomatic, virologically confirmed dengue (VCD) caused by any of dengue's four serotypes more than 28 days after the third dose in Asia (2 to 14-year children), and Latin America (9 to 16-year children) [15], respectively.
While QDENGA® has shown around 80.2 % (95 % CI, 73.3–85.3) efficacy.
And during a phase 1 clinical trial, the efficacy against VCD at 28 days after a single dose of a U.S. NIH-developed vaccine candidate was 79.6 %.
This study assessed the safety and immune response regarding nAbs induced by the SII Dengue vaccine in healthy adults in Australia.
The study showed the vaccine was safe and highly immunogenic in adults, primarily seronegative at baseline.
In the vaccine group, 59.0 % of participants showed DENV vaccine viremia post-vaccination.
This vaccine (Dengusiil) was formulated at Serum Institute of India Pvt. Ltd. (SII) to contain DENV 1, DENV 3, and DENV 4 serotypes at not less than 2.5 log10 PFUs and DENV 2 at not less than 3 log10 PFUs per single dose of 0.5 mL.
SII executive director Rajeev Dhere recently informed the TOI, "The Phase-I trial was conducted in Australia as we needed participants who had not been exposed to dengue previously."
"India has a significant proportion of people with dengue antibodies, so it was essential to test the vaccine's safety and effectiveness on individuals who were not already immune to the disease."
As of August 27, 2023, Dengvaxia is approved in the U.S., but availability requires pre-admission testing.
During 2023, the state of Florida and Puerto Rico have reported locally acquired and travel-related dengue cases.

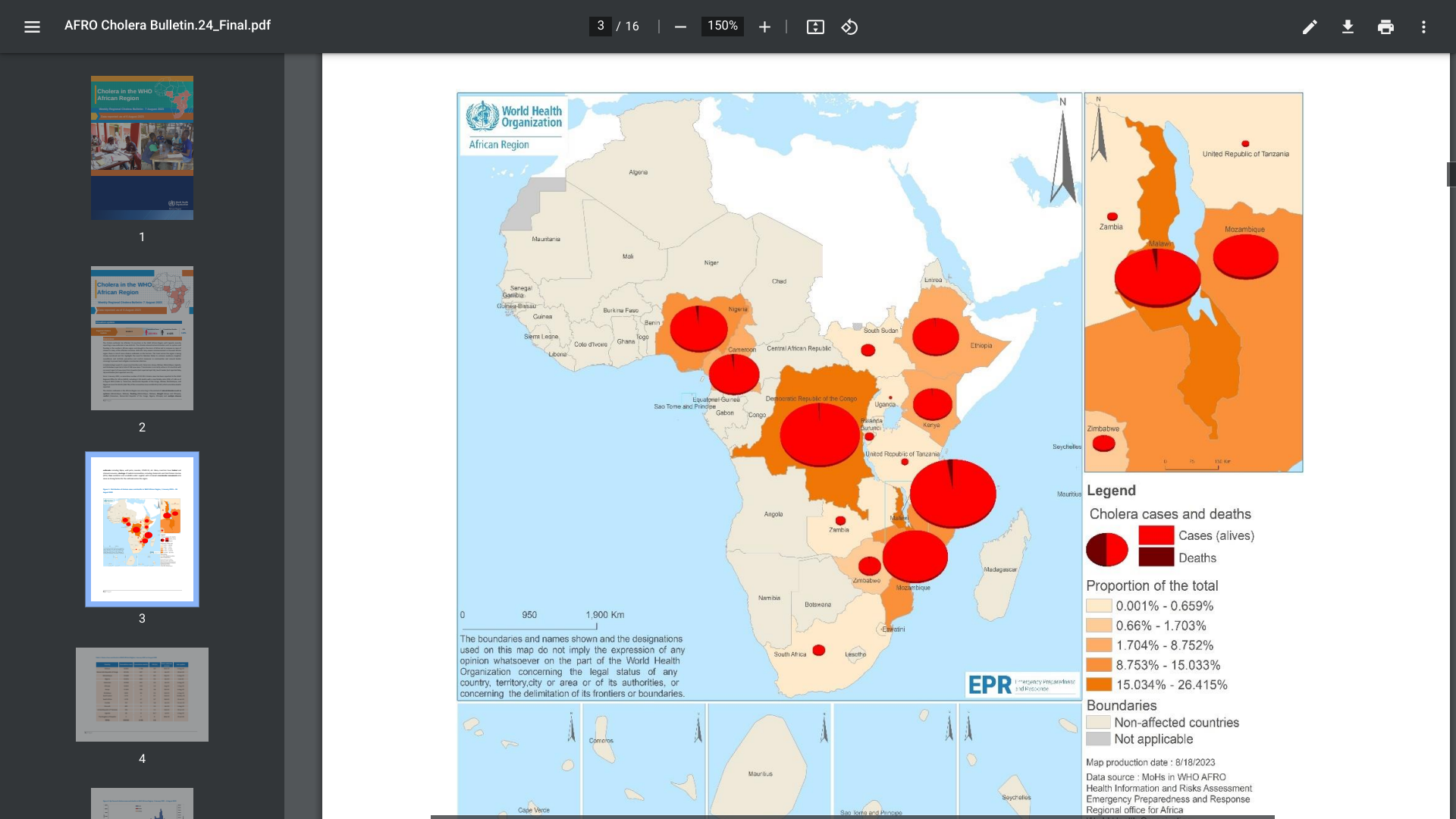
The ongoing, multi-country cholera outbreak was recently confirmed to impact African countries significantly.
The World Health Organization (WHO) Africa Region reported for Epidemiologic Week #31, seven African countries, Burundi, Cameroon, Kenya, Malawi, Mozambique, Uganda, and Zimbabwe reported 328 new cholera cases.
Cholera can kill people within hours when not treated, but immediate access to treatment saves lives.
Since January 2022, a cumulative number of 223,951 cholera cases has been reported to the WHO, including 4,125 deaths, with a case-fatality ratio of 1.8% as of early August 2023.
Based on the large number of cholera outbreaks and their geographic expansion, as well as a lack of oral cholera vaccines and other resources, the WHO continues to assess the risk at the global level as very high, as most cases are not reported.
The U.S. CDC previously confirmed an unprecedented global increase in cholera outbreaks in 2022 and 2023.
Nearly all cholera cases reported in the U.S. are acquired during international travel. The CDC's Clinician Outreach and Communication alert in 2023 identified Cholera as an acute intestinal infection that spreads through food and water contaminated with the bacterium Vibrio cholerae, often from feces. With safe water and sanitation, Cholera can be prevented.
As of August 27, 2023, access to cholera vaccines is constrained globally.
Pfizer Inc. recently announced in a press release that the European Commission (EC) has granted marketing authorization for ABRYSVO™, the company's bivalent respiratory syncytial virus (RSV) prefusion F (RSVpreF) vaccine, to help protect both infants through maternal immunization and older adults.
ABRYSVO is the first licensed vaccine designed and studied explicitly for maternal immunization. Now, a single dose of the vaccine could be administered in the EU between weeks 24 and 36 of gestation.
In addition, ABRYSVO has been studied in adults 60 and older.
"The approval of ABRYSVO in Europe marks significant progress in the scientific community's efforts to provide meaningful protection against RSV, a common respiratory virus that could potentially be severe and even life-threatening, especially for infants and older adults," commented Annaliesa Anderson, Ph.D., Senior Vice President and Head Vaccine Research and Development, Pfizer on August 24, 2023.
"Last year's significant number of newborns, children, and adults being hospitalized across Europe demonstrated the immense need for protection against severe RSV cases. The approval of the vaccine for both older adults and infants through maternal immunization is a triumph for public health, and we hope to see a tremendous impact for future (RSV) seasons."
This authorization is valid in all 27 EU member states, plus Iceland, Liechtenstein, and Norway.
RSV is a contagious virus and a common cause of respiratory illness worldwide.
In the EU, approximately 245,000 yearly hospital admissions were associated with RSV in children younger than five.
The disease burden for older adults is also significant. Each year, the virus causes more than 270,000 hospitalizations and about 20,000 deaths in individuals and older.
The virus can affect an infected individual's lungs and breathing passages, potentially causing severe illness or death.
As of August 26, 2023, two RSV vaccines are approved for seniors and available at clinics and pharmacies in the United States.

The U.S. CDC today published a Morbidity and Mortality Weekly Report (MMWR) that indicates, for the first time in ten years, human papillomavirus (HPV) vaccination initiations did not increase among adolescents in the United States.
Furthermore, coverage with one or more HPV vaccine dose among Medicaid beneficiaries declined by 3.3% in 2022 compared with coverage in 2021.
The cross-sectional analysis published on August 25, 2023, showed that HPV vaccination remained lowest among the uninsured (two of the four groups that constitute the Vaccines for Children (VFC) eligible population.
And the CDC disclosed that VFC vaccine ordering data provide additional evidence that HPV vaccination coverage might continue to decline in VFC-eligible populations.
VFC provider orders for HPV vaccines decreased 24% in 2020, 9% in 2021, and 12% during 2022 compared with 2019.
However, orders for non-HPV vaccines have rebounded to prepandemic levels (Whitlatch F, CDC unpublished data, 2023).
The HPV vaccine is the most expensive of all routinely recommended adolescent vaccines. And reimbursement levels for costs by private payers are adequate, but return margins are small for nonpediatric specialties, according to a study published in Annals of Family Medicine in July 2023.
In the U.S., the CDC's Advisory Committee on Immunization Practices recommends that children aged 11–12 years receive HPV vaccines, and some children can be started at age 9.
The CDC says HPV vaccination is the most effective way of preventing cervical cancer in women and other sexually transmitted HPV cancers.
Various HPV vaccines are available at most health clinics and pharmacies in the U.S.
This CDC report used two analyses of 2022 NIS-Teen data to examine vaccination coverage among U.S. adolescents 13 to 17 years of age.

