Search API
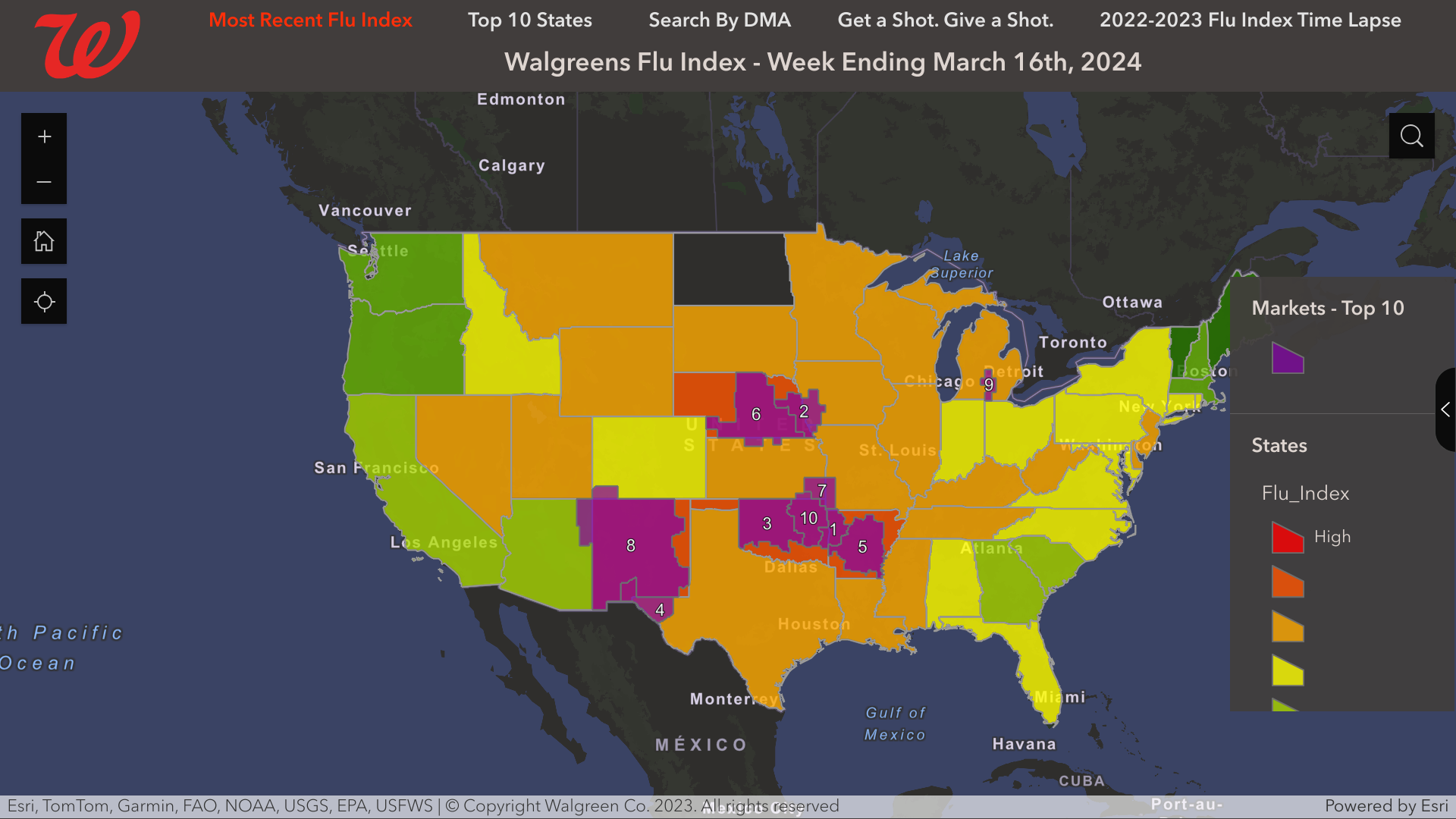
The Walgreens Flu Index® recently published information regarding flu activity compiled using retail prescription data for antiviral medications used to treat influenza across Walgreens locations nationwide.
As of March 16, 2024, Walgreens listed the Top Designated Markets with Flu Activity were:
- Ft. Smith-Fayetteville-Springdale-Rogers, Ark.
- Omaha, Neb.
- Oklahoma City, Okla.
- El Paso, Texas (Las Cruces, N.M.)
- Little Rock-Pine Bluff, Ark.
Seperately the U.S. CDC reported five influenza-associated pediatric deaths during the 2023-2024 flu season during Week # 11. This data increases the flu season total to 121 pediatric deaths.
Last flu season, 184 influenza-associated pediatric deaths were reported.
As of March 24, 2024, various types of flu vaccines remain available at most community pharmacies. About 158 million flu vaccines had been distributed this season.
Note: The Walgreens Flu Index is not intended to illustrate levels or severity of flu activity but rather to illustrate which populations are experiencing the highest incidence of flu.
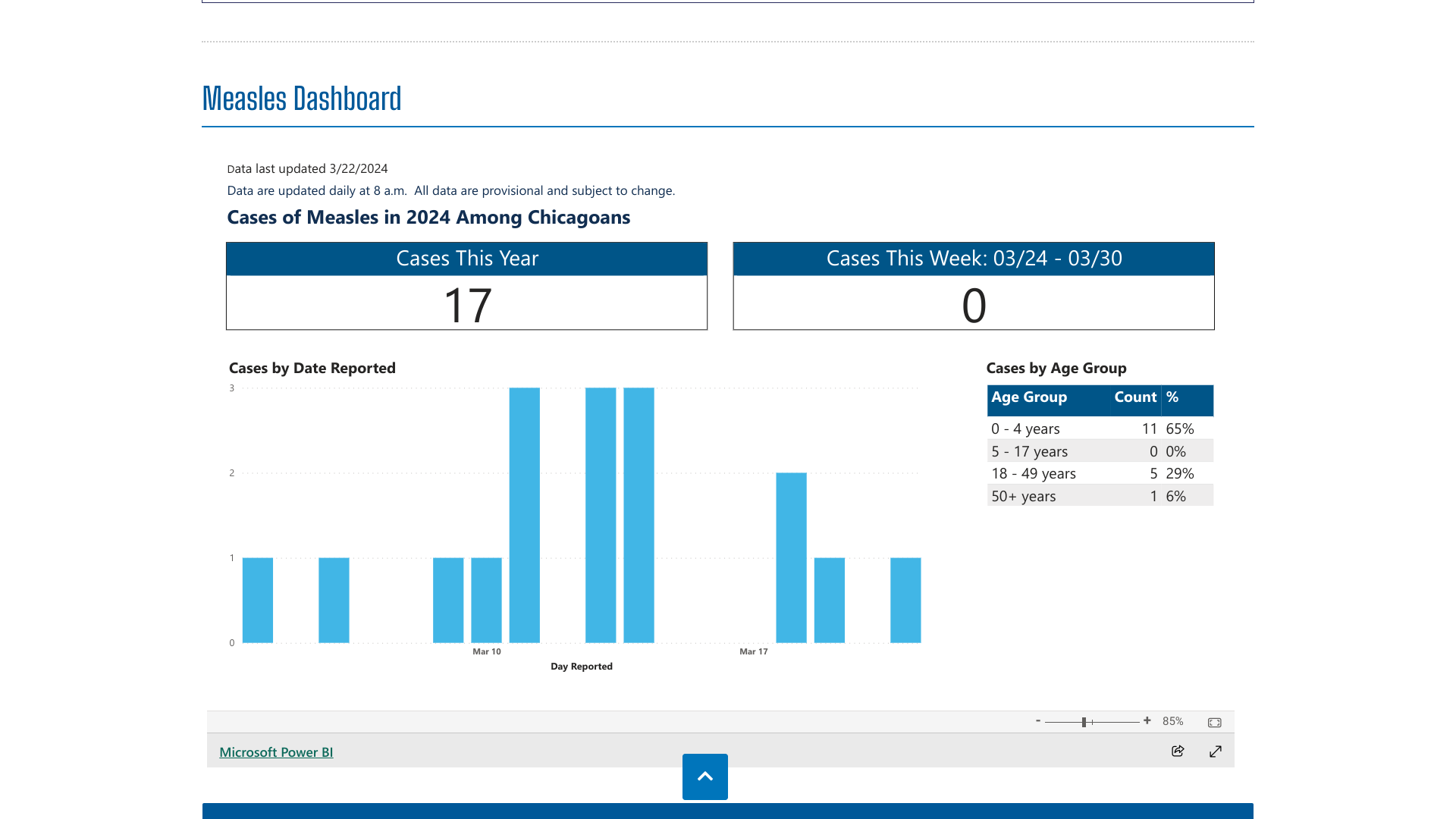
The Chicago Department of Public Health (CDPH) is responding to the first measles cases in the city since 2019 and a recent outbreak.
As of March 24, 2024, CDPH has identified 17 confirmed measles cases in Chicago, most of which have been found in the Pilsen new arrivals shelter on Halsted Street.
Of the 17 confirmed cases, 11 are in children below the age of 5.
CDPH has established vaccine operations at new arrival shelters and the landing zone. Since the measles outbreak began, about 4,000 people have received a measles-mumps-rubella (MMR) vaccine.
MMR vaccination remains the best and most effective way to prevent the spread of measles, and all Chicagoans should review their immunization records or contact their healthcare provider to ensure they are up to date on the vaccine.
MMR vaccinations are generally offered at health clinics and community pharmacies in Illinois.
During 2024, a total of 64 measles cases were reported by 17 jurisdictions: Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, Ohio, Pennsylvania, Virginia, and Washington.
In 2023, the U.S. CDC reported 58 measles cases in 20 jurisdictions.
As World Tuberculosis Day approaches on March 24, everyone should focus on preventing this disease to reduce its impact on society.
According to GlobalData, an analytics company, various TB vaccines are in late-stage development and hold promise in containing the disease burden.
GlobalData reported today that there are currently 11 TB vaccine candidates in the late stages of development.
For example, the M72/AS01E vaccine candidate could be the first licensed TB vaccine in decades.
While the 100-year-old Bacillus Calmette-Guérin (BCG) vaccine is up to 80% effective at preventing TB infection in young children, it provides reduced protection against pulmonary TB.
This means there is a significant need for improved prophylactic vaccines.
Currently, there are about 16 approved TB vaccines in use worldwide.
Anaelle Tannen, Infectious Disease Analyst at GlobalData, commented in a press release on March 22, 2024, "Progress in this area has the potential to save countless lives as well as reduce the health and socio-economic burden associated with this disease."
Tannen added, "Prevention and early diagnosis are key to stopping the ongoing spread of the disease. The BCG vaccine is currently the only prophylactic on the market. It is given to babies in countries where TB is common."
"In areas where TB is less common, it is only given to those at high risk, including those that are more likely to be exposed to the bacterium."
TB remains a global pandemic, with 1.8 billion people estimated to be infected with the bacteria, according to the World Health Organization (WHO). India leads most countries in reporting TB cases and deaths.
The disease exists in both a latent and active form; the latent type does not express symptoms and is not transmissible unless it develops into the active type.
The lifetime risk for latently infected persons is about 5-10%.
Antibiotics are typically administered for at least six months, and ensuring the course is completed is vital to prevent antibiotic resistance, says the WHO.
In the United States, the TICE® BCG vaccine is available at most health departments but not retail pharmacies.

During the recent Respiratory Syncytial Virus (RSV) season, two types of immunization were available to protect young children from this respiratory disease.
As of March 20, 2024, the RSVVaxView Dashboard indicated about 60% of children were protected during the 2023-2024 season.
RSVVaxView reported that 43% of mothers with infants under eight months reported that their child had received Beyfortus™ (Nirsevimab), a single-dose, extended half-life monoclonal antibody offering passive immunization to prevent lower respiratory tract infections caused by RSV.
In February 2024, 38.8% of pregnant women reported that they plan to get nirsevimab for their infant, while 43.7% of women who are trying to get pregnant also reported that they plan to get nirsevimab for their future infant.
In early March 2024, the U.S. CDC reported that nirsevimab was 90% effective at preventing RSV-associated hospitalization in infants during their first RSV season.
With the increasing availability of nirsevimab in future RSV seasons, the CDC will assess its effectiveness over an entire season.
Additionally, among pregnant women with a gestational age of ≥32 weeks, the overall RSV vaccine coverage was about 17.9%.
As of January 31, 2024, the vaccination coverage was highest among non-Hispanic Asian (25.2%) pregnant women.
The CDC wrote, 'These RSV prevention products remain our single most important tool to protect infants during RSV outbreaks.'

A clinical-stage intranasal vaccine company developing parainfluenza virus 5 (PIV5)-vectored vaccines that harness the full breadth of the immune system to protect against serious infectious diseases today announced preliminary data from the first two cohorts of a Phase 1/2a clinical trial studying BLB201, a vaccine candidate against severe respiratory syncytial virus (RSV) disease.
On March 21, 2024, Blue Lake Biotechnology, Inc., stated the data show that BLB201 is immunogenic and well tolerated, with no significant safety events reported to date following a single intranasal dose in RSV seropositive children 18-59 months of age.
The ongoing trial is currently enrolling both RSV seropositive and RSV seronegative children as young as eight months of age.
No vaccine-related severe safety signals have been reported among the initial 10 participants ages 18-59 months who received the BLB201 study vaccine in this Phase 1/2a study (NCT05655182).
In the five participants who received the higher dose of 10⁷ PFU of BLB201, prominent increases in RSV neutralizing antibody (nAb) responses were observed at four weeks post-vaccination, with 80% having a 3.6- to 57-fold rise in nABs over baseline.
RSV-specific mucosal IgA antibody and cellular immune responses were also observed.
“Given the challenges of developing an RSV vaccine for children, it is highly encouraging that BLB201, our intranasal RSV vaccine candidate, has been well tolerated in this age group so far,” said Biao He, Ph.D., founder and CEO of Blue Lake Biotechnology, in a press release.
“It is also very exciting to see RSV-specific immune responses to our vaccine in children who have previously been exposed to RSV. We are eager to generate more data in younger children, including infants who have not had prior exposure to RSV, and to develop a highly effective and safe vaccine to protect this vulnerable population from RSV.”
As of March 2024, approved antibody drugs and a maternal RSV vaccine can provide passive immunity against RSV in infants. However, no RSV vaccine has been approved for generating prophylactic immunity in infants and children.

According to the WHO Regional Office for Europe and the European Centre for Disease Prevention and Control, an estimated 229,000 people were diagnosed with tuberculosis (TB) in the European Region in 2022.
Of these cases, about 83% were reported with pulmonary TB.
Furthermore, there were approximately 18,000 TB-related deaths among HIV-negative individuals in the European Region in 2022.
This represents a 6% increase in deaths compared to 2021.
In 2022, HIV prevalence in incident TB cases was estimated to be 12%, with an estimated 28,000 cases of co-infection in the Region.
Also of concern are signs that the management of TB and HIV co-infection is suboptimal. Only 48% of patients with both TB and HIV in the WHO European Region who started TB treatment in 2021 had been cured.
The TB surveillance and monitoring report published on March 21, 2024, also revealed that nearly 7,000 excess deaths from tuberculosis occurred in the WHO European Region between 2020 and 2022, compared to pre-2020 estimates.
This report stated that increased mortality was a direct result of the recent pandemic and would not have occurred if TB diagnosis and treatment efforts had not been disrupted during the pandemic.
To expedite efforts to reach the end TB targets, WHO and ECDC recommend scaling up initiatives to actively identify and treat missing cases of TB by strengthening TB testing, making preventive treatment options (vaccines) available to all those who need them, and implementing up-to-date, short, and fully oral treatment regimens.
Dr Hans Henri P. Kluge, Regional Director at WHO/Europe, commented in a press release, “The report also reveals another evolving, preventable tragedy - the prevalence of drug-resistant TB continues to rise. We urge national authorities to strengthen TB testing programs, diagnose promptly, and apply the latest WHO guidelines.”
Throughout Europe, versions of the TB-prevention Bacille Calmette-Guérin (BCG) vaccine remain available as of March 2024.
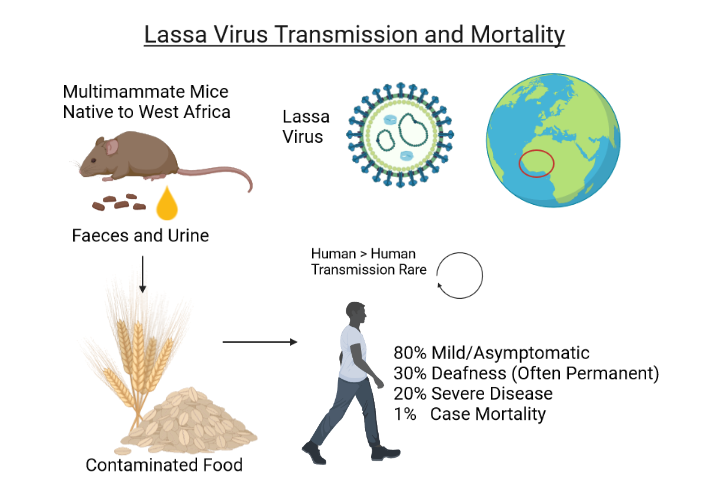
Despite extensive efforts, the Federal Republic of Nigeria continues to confront an expanding Lassa fever outbreak in 2024, reporting new cases and deaths.
Throughout 2024, Nigeria's Centre for Disease Control and Prevention (NCDC) confirmed 682 cases and 128 deaths, which is a Lassa fever case fatality rate of 18.8%, far exceeding the rate recorded in 2023.
The report identified 62% of confirmed cases originating from Ondo, Edo, and Bauchi states.
The NCDC wrote in 2023 that annual outbreaks of Lassa fever also involved infection and death of healthcare workers. This loss of life is not just a statistic but a significant loss of a loved family member, a spouse, a parent, and often a seasoned healthcare worker and team member. This exacerbates the challenge of insufficient human resources for health in the country.'
As of March 2024, the U.S. Food and Drug Administration and the European Medicines Agency had not approved a Lassa fever virus vaccine candidate.
However, four vaccine candidates (INO-4500, MV-LASV, rVSV∆G-LASV-GPC, and EBS-LASV) have entered the clinical clinical stage.
Without an available vaccine, the U.S. CDC says the risk of Lassa virus infection is associated with peridomestic rodent exposure, where inappropriate food storage increases the risk.
The CDC says people should practice safe food precautions and avoid handling, cooking, or eating raw or undercooked meat or animal products.
During the recent pandemic, many scientists were stunned by how fast government agencies authorized new vaccines. Traditionally, it took about eight years for a vaccine to progress through the various stages of clinical trials to obtain market approval.
Many scientists were amazed by the speed at which new vaccines were authorized by government agencies during the recent pandemic.
Traditionally, it took about eight years for a vaccine to progress through the various stages of clinical trials to obtain market approval.
However, new research published on March 21, 2024, suggests that the clinical development of innovative medicines and vaccines will continue to accelerate.
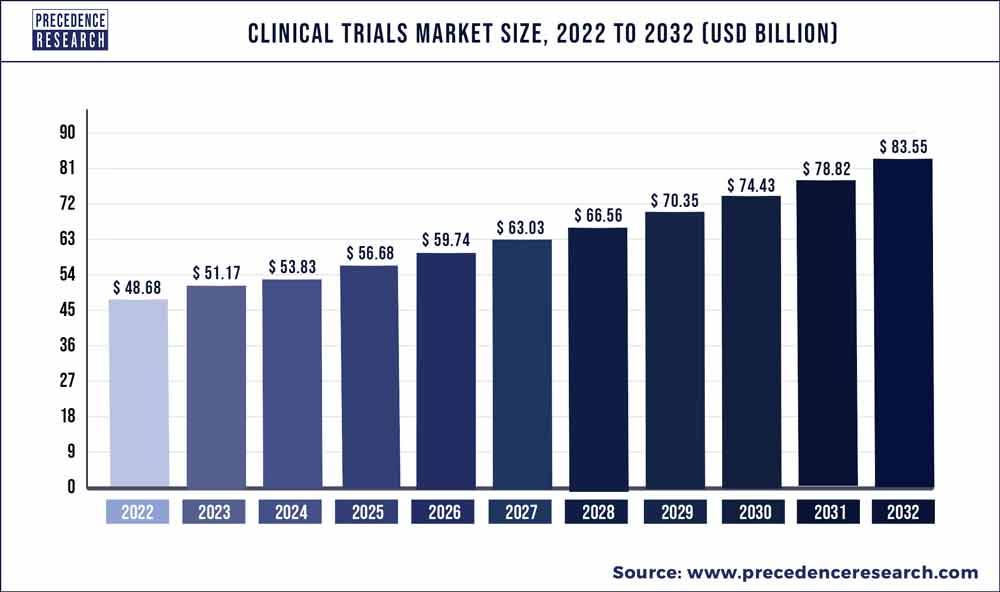
Precedence Research Pvt. Ltd. reported today that the global clinical trials market size was valued at $48.68 billion in 2022 and is predicted to reach about $83 billion by 2032. Clinical trial research was valued at $24.61 billion in the US sub-market in 2022.
The vaccine sub-market reached $102.9 billion in 2023 and is forecasted to expand by 47% to $35.1 billion by 2030.
Furthermore, there is plenty of investor interest in funding new, innovative vaccines.
In the past ten years, companies with infectious disease vaccine programs received 3.4% of the total ($6.5 billion) venture capital raised for biopharmaceutical companies.
Moreover, the promise of personalized vaccines tailored to subpopulations may disrupt the one-size-fits-all vaccination model, further expanding the need for clinical trial research.