Search API
The state’s Department of Fish and Game (ADF&G) recently confirmed the first moose to be diagnosed with rabies in Alaska.
On June 2, 2023, a moose was detected in and around the community of Teller, Alaska, and acting aggressively toward people. The moose was unbalanced, stumbling, drooling profusely, and had bare patches of skin.
ADF&G staff in Nome consulted with wildlife veterinarian Dr. Kimberlee Beckmen and dispatched the animal that afternoon due to its aggressive behavior and signs suggestive of rabies disease.
Rabies virus in the brain was detected on June 5, 2023, by the Alaska State Virology Laboratory.
On June 6, the Centers for Disease Control and Prevention further confirmed the virus was an Arctic Fox rabies variant. This is the same variant circulating in red foxes during the outbreak in the Nome/Seward Peninsula and North Slope arctic foxes this past winter, suggesting the moose contracted the virus from a fox.
Due to this new case, ADF&G plans to increase rabies surveillance by testing all brain samples from wild mammals found dead or euthanized from regions with enzootic fox rabies, including Western Alaska, when feasible.
Due to the largely solitary nature of moose, it is doubtful that any rabies outbreak will occur in the moose population, but isolated cases such as this one occur rarely.
Moose that are killed by hunters on the Seward Peninsula that show normal behavior and no signs of any abnormality or illness should still be considered safe to consume, says ADF&G.
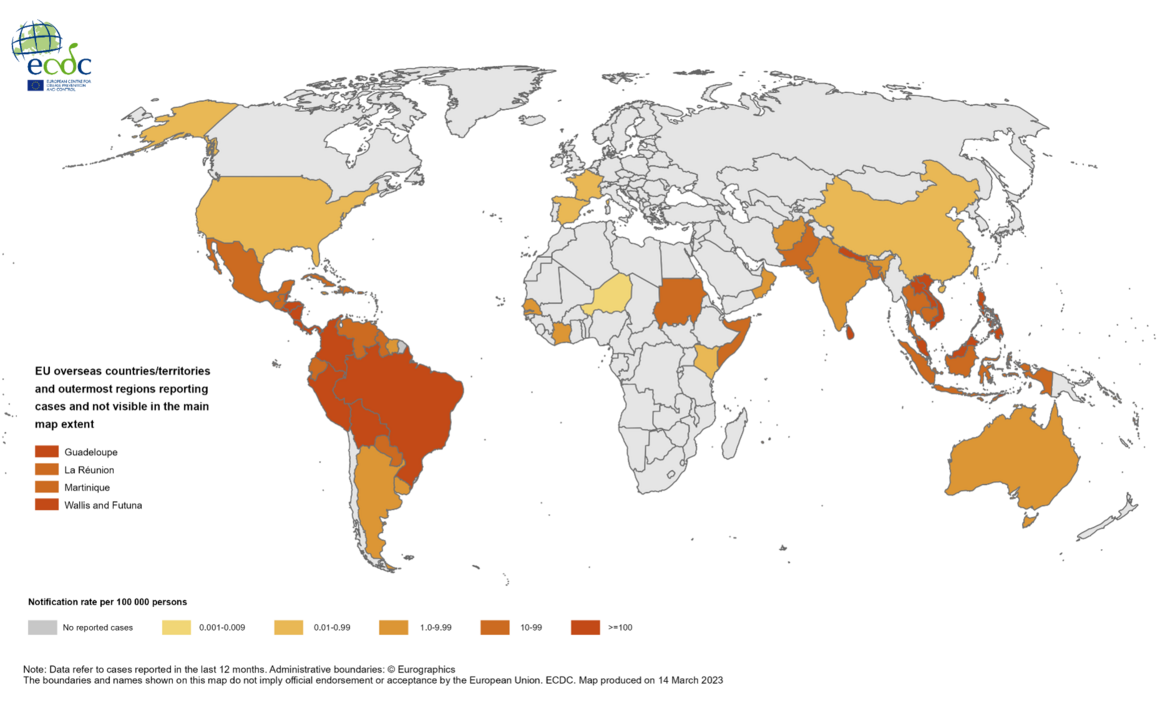
Rabies is a zoonotic infection found in more than 150 countries and territories, say the World Health Organization (WHO). Unfortunately, almost 60,000 people worldwide die from rabies annually.
According to the WHO, rabies vaccination can prevent infections before and after exposure to the rabies virus.
On May 6, 2022, the U.S. CDC published: Using a Modified Preexposure Prophylaxis Vaccination Schedule to Prevent Human Rabies.

Filomeno Fortes, the Director of Portugal's Institute of Hygiene and Tropical Medicine, recently gave an interview on the importance of Takeda's QDENGA® vaccine against dengue, made available in Portugal in May 2023.
"The vaccine brings some innovation to the prevention of a disease that is considered by the World Health Organization (WHO) as one of the ten global threats to world health," commented Fortes.
Initially authorized in Indonesia in August 2022, QDENGA had been authorized as of June 9, 2023, in Argentina, Brazil, Europe, and the U.K.
In the U.S., the FDA is considering the authorization of QDENGA.
Since most dengue cases in the U.S. are travel-related, additional QDENGA authorization should reduce the incidence of this disease.
About 4 billion people live in areas with a risk of dengue.
For example, the Florida Health Department recently reported three additional travel-associated dengue cases, which increases the 2023 total to 80 patients.
In 2022, 903 travel-associated and 68 locally-acquired dengue cases were reported in Florida.
Dengue viruses are spread to people through the bite of an infected Aedes species mosquito, says the U.S. CDC. Dengue is often a leading cause of illness in at-risk areas.
The U.S. Centers for Disease Control and Prevention (CDC) today published a Morbidity and Mortality Weekly Report that confirmed children and infants have been infected with the mpox virus.
From May 17 to December 31, 2022, the CDC reported that 45 children aged ≤12 years were diagnosed with mpox.
And three were less than one week old. These infants likely had perinatal exposures.
The vaccination status (JYNNEOS®) of these children was not disclosed.
The CDC stated on June 9, 2023, when caring for a child with mpox, direct contact with the child’s rash should be avoided, and gloves should be worn. In addition, postexposure prophylaxis (TPOXX®) should be considered for all household members.
On May 18, 2023, the CDC confirmed TPOXX might be used for non-variola orthopoxvirus infection (e.g., mpox) under a CDC-held Expanded Access Investigational New Drug Protocol for children weighing at least 3 kg.
However, mpox postexposure prophylaxis efficacy is unstudied.
Additional mpox research was updated in June 2023.

WestVac Biopharma and West China Medical Center, Sichuan University, today announced Coviccine® Trivalent XBB.1.5-Recombinant COVID-19 Trivalent (XBB.1.5+BA.5+Delta) Protein Vaccine (Sf9 cell) was authorized by relevant authorities in China.
As of June 8, 2023, this is the first COVID-19 vaccine in the world authorized against XBB descendent lineages of the beta coronavirus SARS-CoV-2.
WestVac leveraged the rapid response of the insect cell expression platform in constructing the vector for Coviccine, which is of high purity and high quality for human use.
The subunit vaccine antigen is designed based on the structure of the targeting S-RBD and HR proteins of the COVID-19 subvariants XBB.1.5 and BA.5 and self-assembled into stable trimeric protein particles with squalene-based oil-in-water emulsion adjuvant added after purification and mixing.
This novel adjuvant significantly raises the titer of neutralizing antibodies, enabling the trimeric protein vaccine to induce a higher T-cell immune response.
Recent studies have shown that Coviccine induced a high titer of neutralizing antibodies against multiple subvariants.
Previously, the WHO Technical Advisory Group on COVID-19 Vaccine Composition advised on May 18, 2023, that new formulations of COVID-19 vaccines should aim to induce antibody responses that neutralize XBB descendent lineages.
As of the end of May 2023, the XBB family of variants accounted for about 90% of infections in China.
And in the U.S., over 90% of all variants are from the XBB family.

CNBC reported today the U.S. FDA's Antimicrobial Drugs Advisory Committee voted 21-0 to recommend full approval for Beyfortus® (Nirsevimab) for infants and young children.
The FDA considers committee recommendations when finalizing its decisions.
Beyfortu has already been approved in Canada, Europe, and the United Kingdom.
Beyfortus is the first extended half-life monoclonal antibody offering passive immunization to prevent lower respiratory tract infections caused by the respiratory syncytial virus (RSV).
AstraZeneca and Sanofi developed this RSV therapy.
This antibody therapy is not an RSV vaccine. The FDA recently approved two RSV vaccines for seniors.

The U.S. CDC's Morbidity and Mortality Weekly Report published today indicates about 66% of mpox vaccine–eligible persons remained unvaccinated.
From May 2022–April 2023, a total of 748,329 first JYNNEOS® (MVA-BN) vaccine doses (of the two recommended) were administered in the United States.
During the initial months of the outbreak, lower vaccination coverage rates among racial and ethnic minority groups were reported.
Focusing on the racial and ethnic groups with more significant mpox vaccination shortfalls, prioritizing resources, and improving access to vaccination for these groups can reduce the overall shortfall in mpox vaccination while promoting health equity.
However, after the implementation of initiatives developed to expand access to mpox vaccination, coverage among racial and ethnic minority groups increased, stated the CDC on June 9, 2023.

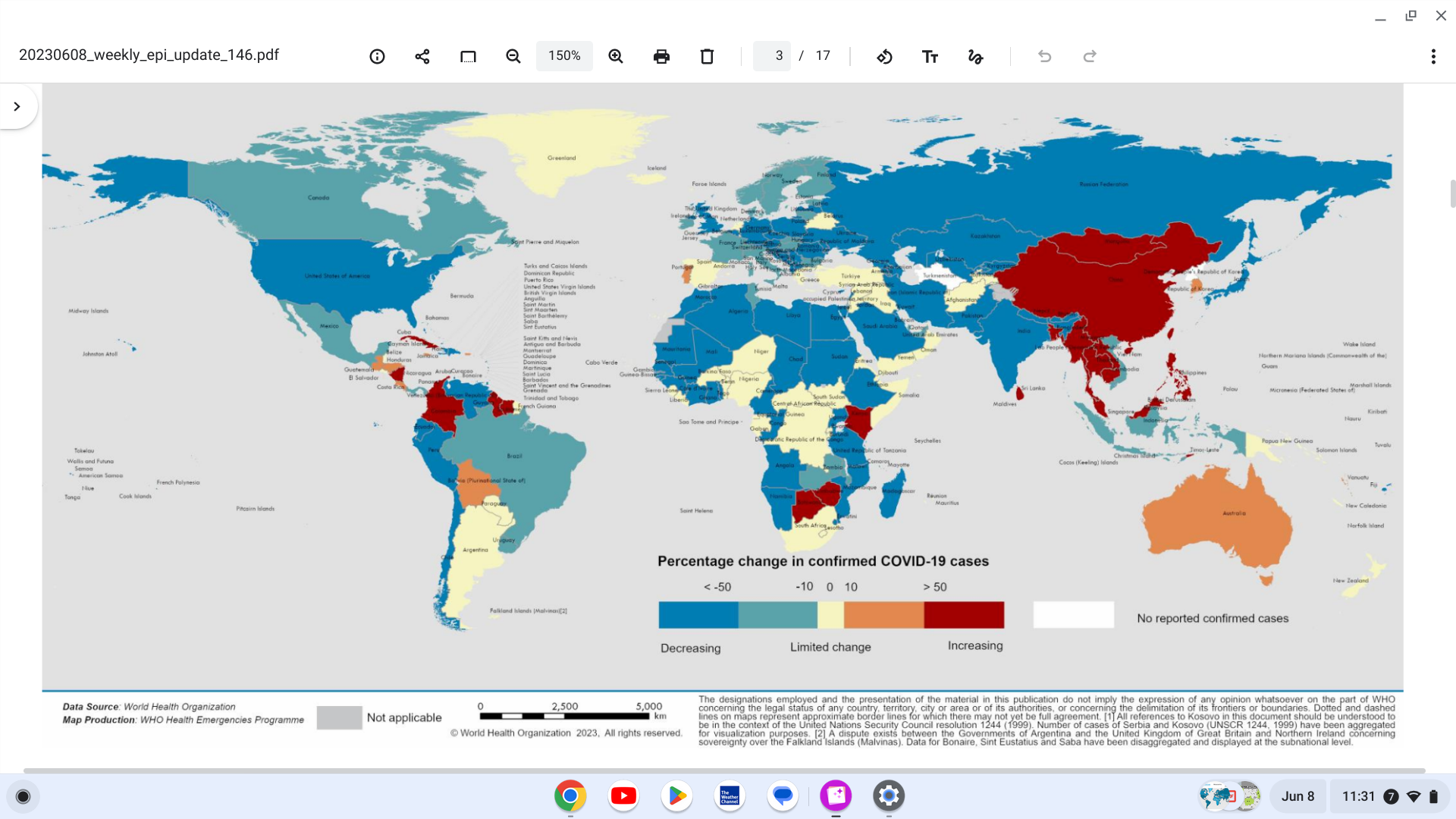
The World Health Organization (WHO) today reported over 10,000 fatalities related to COVID-19 were reported in the last 28 days, a decrease of 47% compared to April 10 to May 7, 2023.
During this 28-day reporting period, 144 of 243 (59%) countries and territories reported at least one COVID-19 case.
The situation at the regional level shows decreases in COVID-19 cases and fatalities in all six WHO regions.
Recently, the WHO and other authorities have announced their recommendations for updated COVID-19 vaccines for late 2023.
And the Forest plots displaying the effectiveness of COVID-19 vaccines against the Omicron variants are available on View-hub.org.
The outbreak of Marburg Virus Disease in Equatorial Guinea ended today with no new cases reported over the past 42 days after the last patient was discharged from treatment.
The outbreak, declared on February 13, was the first in Equatorial Guinea.
A total of 17 laboratory-confirmed cases and 12 deaths were recorded.
Five districts in four of Equatorial Guinea’s eight provinces were affected.
The western Litoral province Bata district was worst-hit, with 11 laboratory-confirmed cases reported. Among the reported cases, many were closely linked either through social gatherings and networks or geographically.
“While outbreak-prone diseases continue to pose a major health threat in Africa, we can bank on the region’s growing expertise in health emergency response to act quickly and decisively to safeguard the health and avert widespread loss of life,” said Dr. Matshidiso Moeti, World Health Organization (WHO) Regional Director for Africa, in a press release on June 8, 2023.
“The hard work by Equatorial Guinea’s health workers and support by partner organizations has been crucial in ending this outbreak. WHO continues to work with countries to improve measures to detect and respond effectively to disease outbreaks,” Dr Moeti added.
To support Equatorial Guinea’s response to the just-ended outbreak, WHO deployed experts in epidemiology, clinical management, health operations, logistics, risk communications, and infection prevention and control.
The Organization worked with the health authorities to set up a treatment center, provided medical supplies, including antivirals, and trained health workers in the critical aspects of outbreak control.
The WHO also supported the efforts by the authorities in neighboring Cameroon and Gabon to ramp up outbreak readiness and response.
Although the outbreak has ended, WHO continues to work with Equatorial Guinea to maintain measures such as surveillance and testing to enable prompt action should flare-ups of the virus occur, with the training provided during the outbreak helping to strengthen readiness capacity.
Marburg is in the same family as the virus that causes Ebola Virus Disease.
The Marburg virus is transmitted to people from fruit bats and spreads among humans through direct contact with the bodily fluids of infected people, surfaces, and materials.
In Africa, the first outbreak of Marburg was recorded in South Africa in 1975, followed by two others in Kenya in the 1980s. Since then, outbreaks have been reported in Angola, the Democratic Republic of the Congo, Ghana, Guinea, Uganda, and most recently, Equatorial Guinea and Tanzania.


