Search API
The future vaccination plans for U.S. travelers and those living in dengue-outbreak areas, such as Puerto Rico, were disrupted yesterday.
Takeda announced on July 11, 2023, that the Company had voluntarily withdrawn the U.S. Biologics License Application (BLA) for its dengue vaccine candidate, TAK-003, following discussions with the U.S. Food and Drug Administration (FDA).
Takeda's press release stated that aspects of data collection could not be addressed within the current BLA review cycle.
On November 22, 2022, Takeda announced that the FDA had accepted and granted priority review of the TAK-003 BLA.
TAK-003, known internationally as QDENGA®, is approved in multiple endemic and non-endemic countries, such as the United Kingdom, Europe, and Brazil.
Gary Dubin, M.D., president of Takeda's Vaccines Business Unit, commented in a related press release, "The urgent global need to combat the growing burden of dengue remains, and we will continue to progress regulatory reviews and provide access for people living in and traveling to dengue-endemic areas while we work to determine next steps in the U.S."
QDENGA® is a tetravalent dengue vaccine preventing Dengue Fever or Severe Dengue caused by any of the four serotypes of the dengue virus.
During 2023, locally-acquired dengue has been confirmed in Florida and Texas.
While other second-generation dengue vaccine candidates are in development, the initial FDA-approved dengue vaccine Dengvaxia® remains available in the U.S. but has specific pre-vaccination requirements.

Dengue fever outbreaks continue to confront numerous countries in 2023. To extend access to dengue vaccines, the U.S. Food and Drug Administration (FDA) recently approved a supplement Biologics License Application (sBLA) for Dengue Tetravalent Vaccine, Live (Dengvaxia®).
On June 30, 2023, the FDA issued to Michael F. Stirr, Sanofi Pasteur, Inc. BL 125682/40, to include safety and efficacy data that support the use of Dengvaxia in individuals 6 through 16 years of age, with laboratory-confirmed previous dengue infection and living in endemic areas.
This FDA expansion is important as no specific medication to treat dengue infection exists.
As of July 3, 2023, the FDA's review of this supplement was associated with the following National Clinical Trial numbers: NCT01373281, NCT01374516, NCT00842530, and NCT01983553.
The three-dose Dengvaxia's (CYD-TDV) original BLA was approved by the FDA on May 1, 2019. It was first licensed in Mexico in 2015 for use in individuals 9-45 years of age and is now licensed in over 20 countries.
Dengvaxia is the only dengue vaccine recommended for routine use by the U.S. CDC's Advisory Committee on Immunization Practices.
Before being vaccinated with Dengvaxia, the CDC's vaccine committee says healthcare providers that if a patient has dengue symptoms or lives in or has recently traveled to an area with a risk of dengue and has not previously been infected, they are at increased risk for Severe Dengue disease when vaccinated and subsequently infected with the dengue virus.
Dengue is caused by infection with any of the four dengue viruses.
According to the CDC, these viruses are transmitted in tropical and subtropical regions by infected Aedes mosquito species.
During the summer of 2023, locally-acquired dengue cases have been reported in Florida, Texas, Puerto Rico, and Costa Rica.

Vaxcyte, Inc. today announced that the ongoing Phase 2 study of the VAX-24 pneumococcal conjugate vaccine (PCV) candidate in healthy infants is advancing to the second and final stage.
The Phase 2 study is evaluating the safety, tolerability, and immunogenicity of VAX-24, the Company’s lead, broad-spectrum 24-valent PCV designed to prevent invasive pneumococcal disease.
Vaxcyte’s Phase 2 infant study is being conducted in two stages and compares VAX-24 to the broadest-spectrum standard-of-care PCVs currently available.
Stage 1 of the study evaluated the safety and tolerability of a single injection of VAX-24 at three dose levels in a dose-escalation approach compared to VAXNEUVANCE™ (PCV15) in 48 infants.
The Stage 2 portion is evaluating the safety, tolerability, and immunogenicity of VAX-24 at the same three dose levels compared to PCV20 in approximately 750 infants.
In agreement with the U.S. Food and Drug Administration, Vaxcyte amended the study protocol for Stage 2 and changed the study comparator to PCV20, which is currently the broadest-spectrum PCV recommended by the U.S. CDC's Advisory Committee on Immunization Practices.
Grant Pickering, Chief Executive Officer and Co-Founder of Vaxcyte said in a press release on July 11, 2023, “We designed VAX-24 to deliver broader coverage and improved immune responses, and we look forward to sharing topline data from the primary three-dose immunization series by 2025", followed by topline data from the booster dose approximately nine months later.

Given an increase in outbreaks caused by different microorganisms associated with medical and health tourism, the Pan American Health Organization / World Health Organization (PAHO/WHO) recently announced it encouraged Member States to strengthen their capacity to detect and manage related infections.
On July 7, 2023, the PAHO/WHO stated in recent years, the Region of the Americas has experienced an exponential growth of international travel in search of health care. For example, millions of Americans travel to other countries for health care each year, primarily to Mexico, Canada, and other countries in Central America, South America, and the Caribbean.
It is estimated that for the United States alone, the annual number has increased from 750,000 to 1.4 million over ten years (2007 to
2017).
Additionally, the U.S. Centers for Disease Control and Prevention (CDC), the Mexican Ministry of Health, and U.S. state health departments are responding to a multinational fungal meningitis outbreak among 35 people who had procedures in Matamoros, Tamaulipas, Mexico.
Ten U.S. patients have confirmed cases of fungal meningitis, and eight have died, according to the U.S. CDC.
The CDC says anyone who had procedures under epidural anesthesia from January to May 13, 2023, is at risk for fungal meningitis.... and should go to the nearest emergency room as soon as possible to be evaluated for fungal meningitis, even if you do not currently have symptoms.
Fungal meningitis is a rare, life-threatening fungal infection that causes swelling of the areas around the brain and spinal cord. Starting treatment right away if you are found to have fungal meningitis greatly increases the likelihood of survival.
However, infections are not contagious and are not spread from person to person, says the CDC.

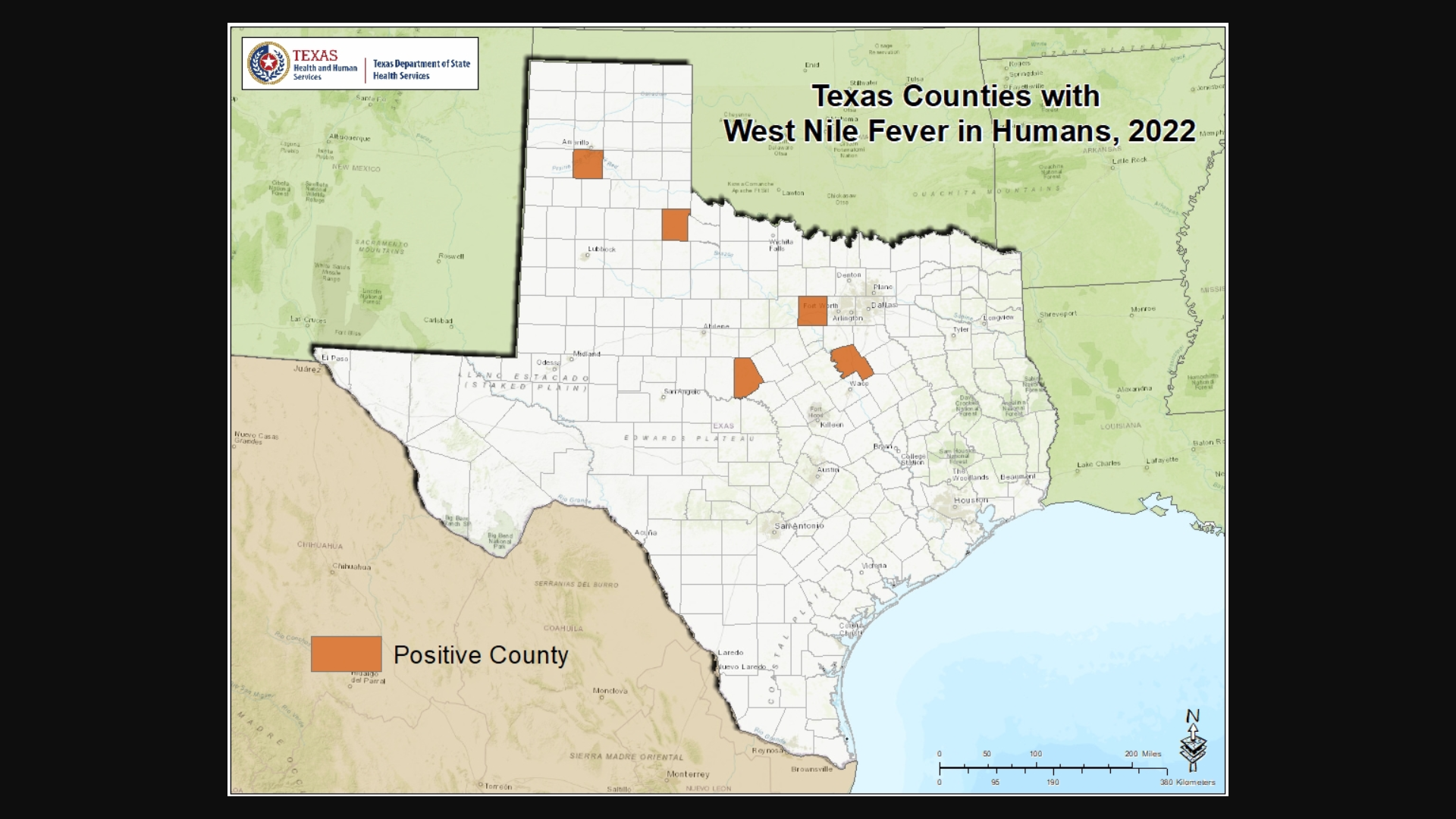
Dallas County Health and Human Services (DCHHS) today reported the first human case of West Nile Virus (WNV) in Dallas County for 2023.
The patient is a male resident and was diagnosed with West Nile Neuroinvasive Disease (WNND), which may affect the brain and spinal cord.
WNV is a disease that is spread by the bite of an infected mosquito. It is the leading cause of mosquito-borne disease in the U.S. The virus can infect humans, birds, mosquitoes, horses, and some other animals.
“WNV is transmitted to humans by the bite of an infected mosquito, and people should be careful when going out outside to enjoy outdoor activities,” said Dr. Philip Huang, DCHHS Director, in a press release on July 10, 2023.
Most people infected with WNV, about 80%, will not develop illness, says the Texas Health and Human Services.
Twenty percent of infected people develop a typically mild form of the disease known as West Nile fever, which may include fever, headache, body aches, and occasionally a skin rash on the trunk of the body and swollen lymph glands.
Only about one out of 150 people infected with West Nile virus will develop WNND.
As of late June 2023, there has been 10 WNND cases confirmed this year.
The U.S. CDC says there is no specific treatment for WNV infections nor is there an effective human vaccine.
The U.S. Centers for Disease Control and Prevention (CDC) recently issued a statement confirming when and explaining how the new COVID-19 vaccines will be available after September 2023.
The CDC stated on July 6, 2023, the new monovalent XBB.1.5 composition vaccines will be the first COVID-19 vaccines to be available directly from the pharmaceutical manufacturers as part of the commercial market rather than through the United States Government (USG).
It is anticipated that USG will stop the regular threshold/replenishment ordering mechanism for all COVID-19 vaccines and ancillary supplies on August 3, 2023.
Providers are encouraged to place necessary orders before that cutoff date.
Suppose a provider requires additional supply to be responsive to demand after USG closes the current ordering mechanism. In that case, COVID-19 vaccines will remain available for ordering via the established out-of-cycle request process.
The public will continue to be directed to Vaccines.gov to find providers offering COVID-19 vaccines.
CDC will provide access to COVID-19 vaccines for uninsured individuals once COVID-19 vaccines become commercially available.
Uninsured children can receive COVID-19 vaccines through the existing Vaccines for Children program.
And uninsured adults can receive COVID-19 vaccines through a new temporary program called the Bridge Access Program for COVID-19 Vaccines and Treatments.
As of July 7, 2023, more than 304.7 million doses of COVID-19 vaccine have been administered and reported by Federal Retail Pharmacy Program participants in the US. This includes 8 million doses administered onsite to long-term care facilities in the early days of the COVID-19 vaccination program.
Furthermore, detail on the current recommended vaccine schedules for each age group can be found on the CDC website.

According to numerous reports, the Republic of Peru is confronted with another Guillain-Barré Syndrome (GBS) outbreak.
The Peruvian Government recently published Supreme Decree No. 019-2023-SA in the Official Gazette El Peruano, declaring a national health emergency due to the unusual increase in GBS cases in 18 of the country's 24 departments.
As reported on July 10, 2023, 182 cases of GBS have been confirmed, and four people have died since June 2023, per MercoPress.
Peru's president Dina Boluarte also issued a decree allocating $3.27 million for an action plan to improve patient care, including acquiring 5,000 immunoglobulin vials for treating patients affected by GBS.
Issued on July 8, 2023, this emergency declaration will be valid for 90 calendar days.
The U.S. Centers for Disease Control and Prevention (CDC) says GBS is the most common form of acute flaccid paralysis worldwide. It is characterized by motor weakness and other symptoms.
The CDC reported in a November 2020 Research Letter that from May 20–July 27, 2019, the Government identified 683 suspected or confirmed GBS cases in Peru.
Of the 683 GBS patients, 287 (42%) had descending muscle weakness, and 446 (65.3%) had ascending muscle weakness.
Of 426 patients for whom hospitalization data were available, 64 (15%) required mechanical ventilation.
Of 147 patients with an electrodiagnostic exam, 100 (68%) had acute motor axonal neuropathy.
The CDC stated this GBS outbreak was unusual because of the many cases. The incidence rate was nearly 25 times higher than expected.
And the rapid increase in numbers was followed by an equally precipitous decrease, which might suggest a point-source exposure.

Vaxart, Inc. recently announced positive topline data from the dose-ranging Phase 2 clinical trial of its oral pill bivalent norovirus vaccine candidate.
This study's preliminary results showed robust serum immune responses across all doses at Day 29 relative to Day 1.
Both doses showed a similar increase in serum antibody responses with no statistical difference between the medium and high dose arms, and the mucosal and cell-based assay data will be available later.
Dr. James F. Cummings, Vaxart's Chief Medical Officer, commented in a press release on July 6, 2023, "These data, additional forthcoming data from this study, and the data we expect from our norovirus challenge study, will help inform our selection of dosage levels in a larger Phase 2b study."
"And support an End-of-Phase 2 meeting with the U.S. Food and Drug Administration."
"Our bivalent vaccine is designed to target the most important genogroups, GI and GII, and specifically to cover the important strains, GI.1 and GII.4. GII.4 currently causes the majority of norovirus disease in humans."
This Phase 2 dose-ranging study demonstrated that the bivalent norovirus vaccine candidate was well tolerated, with a favorable safety profile.
This is the seventh clinical trial completed in Vaxart's norovirus program, and it supports previous findings of robust immunogenicity and benign tolerability.
As of July 10, 2023, Vaxart's vaccine is one of several norovirus vaccine candidates conducting clinical research.
Norovirus is a very contagious virus that causes vomiting and diarrhea. Anyone can get infected and sick with norovirus. The U.S. Centers for Disease Control and Prevention (CDC) says norovirus cases generally occur most frequently during late fall, winter, and early spring.
The CDC publishes the Norovirus Outbreak Map and posts Norovirus National Trends.